Podcasts about cancer clinic
- 28PODCASTS
- 31EPISODES
- 30mAVG DURATION
- ?INFREQUENT EPISODES
- Aug 22, 2024LATEST
POPULARITY
Best podcasts about cancer clinic
Latest news about cancer clinic
- Health minister provides cancer care update in Kelowna but motivation questioned Global News - Jun 28, 2024
- Caring for patients and cutting carbon: how a pioneering cancer clinic is reducing emissions The Guardian - Feb 15, 2024
- Private Cancer Clinic Owners Threaten to Sue Whistleblowers The Tyee | BC's home for today's news, analysis and updates - Feb 12, 2024
- First Stand-alone Cancer Facility in the Philippines Now Open in Laguna When In Manila - Dec 11, 2022
- University of Maryland Upper Chesapeake Health’s High-Risk Breast Cancer Clinic provides resources to those with higher risk of breast cancer Baltimore Sun - Oct 14, 2022
Latest podcast episodes about cancer clinic
Dr. Lillian Siu and Dr. Melvin Chua discuss the new technologies and novel therapeutics that were featured at the 2024 ASCO Breakthrough meeting. TRANSCRIPT Dr. Lillian Siu: Hello and welcome to the ASCO Daily News Podcast. I'm Dr. Lillian Siu, a medical oncologist and director of the Phase 1 Trials Program at the Princess Margaret Cancer Center in Toronto, Canada, and a professor of medicine at the University of Toronto. On today's episode, we'll be discussing key takeaways from the 2024 ASCO Breakthrough meeting in Yokohama, Japan. Joining me for this discussion is Dr. Melvin Chua, who served as the chair of Breakthrough's Program Committee. Dr. Chua is the head of the Department for Head, Neck and Thoracic Cancers in the Division of Radiation Oncology at the National Cancer Center in Singapore. Our full disclosures are available in the transcript of this episode. Dr. Chua, it's great to be speaking with you today and congratulations on a very successful Breakthrough meeting. Dr. Melvin Chua: Thanks Dr. Siu. It was really inspiring to come together again to showcase the innovative work of world-renowned experts, clinicians, researchers, med-tech pioneers, and drug developers from around the globe. Our theme this year was inclusivity and thus it was important to bring people together again in the Asia Pacific region and to foster international collaborations that are so important in advancing cancer care. This year, we invited 65 international faculty, of which 55% were from Asia. Also, importantly, we achieved approximately a 50-50 split for male to female representation. These are remarkable statistics for the meeting, and we really hope to retain this for future Breakthrough [meetings]. Dr. Lillian Siu: The meeting featured renowned keynote speakers who shared great insights on new technologies and therapies that are shaping the future of drug development and care delivery. Let's first talk about artificial intelligence and the keynote address by Dr. Andrew Trister. He gave a very interesting talk titled, “Plaiting the Golden Braid: How Artificial Intelligence Informs the Learning Health System.” What are the key messages from his talk? Dr. Melvin Chua: Couldn't agree with you more, Dr. Siu. Dr. Trister is the chief medical and scientific officer of Verily, a precision health company. He previously worked in digital health and AI at The Bill and Melinda Gates Foundation, and worked at Apple where he led clinical research and machine learning with Apple partners. But perhaps it was really his background and training as a radiation oncologist that was most pertinent as he was able to weave both the components of new AI models and the applications and pitfalls in the clinic to the audience. Dr. Trister provided a very high-level view through the history of AI and showcased the progression of the different AI models and he basically explained between deep and shallow methods as well as deductive logic versus inductive probabilistic methods. He then provided several clinical examples where these models have shown their utility in the clinic, for example, pathology and so forth. At the same time, he illustrated several pitfalls with these models. So overall, I think Dr. Trister's talk was very well received by the audience with several key messages, including the importance of [using] high-quality data as the basis of a good AI model. AI was also addressed in an Education Session that looked at Artificial Intelligence in the Cancer Clinic. And we had a panel of experts that highlighted current progress and successes with AI in the clinic, advances with AI assisted pathology for clinical research and precision medicine, large language models (LLMs) for applications in the clinic, and how we could leverage AI in precision oncology. And from this session, I had several key takeaways. Dr. Alexander Pearson [of the University of Chicago] gave a very illustrative talk on how multimodal information across clinical omics, radiological information and multi omics could be used to improve diagnostic tasks and clinical prediction across different cancers. And Dr. Joe Yeong [of Singapore General Hospital] gave a very good talk on how AI can be applied in digital pathology to accelerate research in immunology and help in the development of immunotherapies. Dr. Danielle Bitterman [of Brigham and Women's Hospital] shared very good examples of how LLMs could be used in a clinic. And I think the example that really stood out for me was how LLMs could be deployed to create responses to patient queries. And of course, the big question in the room was: How could AI eventually encapsulate compassion in their response? I think this again showcased how LLMs could really help to accelerate our clinical work going forward. And ultimately circling back to data, Dr. Caroline Chung [of MD Anderson] gave a very poignant description on the importance of data quality and how poor-quality data could eventually lead to underperforming AI models. So all in all, I think this was a great session. And what do you think, Dr. Siu? Dr. Lillian Siu: Melvin, I totally agree with you. I like all your comments and I really enjoyed the keynote as well as the session on AI in the cancer clinic chaired by Dr. Pearson. I think all these sessions were really informative. Discussions on the latest AI and machine learning, algorithms and technologies on digital pathology, LLMs and big data, as you said, really enables the attendees, especially clinicians like me, to gain a deep understanding of how AI can be translated to practical applications. Dr. Melvin Chua: Great. So, Dr. Siu, let's talk about some of the novel therapeutics that were featured at the meeting. Again, this was an important session for Breakthrough, and it's always been there. So could you share some highlights from the sessions on novel drug development from your perspective? Dr. Lillian Siu: Yes, indeed. Drug development is such an exciting aspect of this meeting. On Day 3 of the meeting, we had a keynote by Dr. Shimon Sakaguchi of Osaka University, who discussed “Targeting Regulatory T cells (Tregs) in Cancer: The Science, Trials, and Future.” And he talked about T cells, especially Treg biology, the role of Tregs in immune regulation, new developments in Treg immuno-oncology drugs, and how we can actually target Tregs to treat early cancers, etc. This talk is particularly exciting because there are now anti CCR8 antibodies in the clinic that specifically target Tregs, and some early signals of anti-tumor activities are already being observed. Dr. Sakaguchi also emphasized the importance of combination sequence and timing of drugs for the successful use of cancer immunotherapeutic agents. I also want to emphasize the Education Session that followed, titled, “The Future of Immunotherapy, New Drugs and New Ideas.” In that particular session, we heard about engineering T-cell immunity to eradicate tumors. We heard about CAR T-cell therapy in GI cancers, novel immunotherapeutic combinations, and T-cell engagers, which are bispecifics in cancer. While success with some of these immunotherapeutic modalities, such as cell therapies and T-cell engagers have been largely seen in hematological malignancies, we are beginning to observe efficacy signals in solid tumors. For example, the CAR T targeting Claudin18.2 in gastrointestinal cancers and the recently approved FDA-approved DLL3/CD3 bispecific T-cell engager, tarlatamab, in small cell lung cancer are really exciting examples. We also heard from investigators who are exploring neoadjuvant therapies in the neoadjuvant therapy session, and the key takeaway from that session is that we have growing interest in using neoadjuvant therapy or perioperative therapy. In other words, neoadjuvant plus adjuvant therapy in different cancers. In the neoadjuvant session, there were updates provided by different experts on the roles of neoadjuvant therapy in melanoma, liver cancer, bladder cancer, and nasopharyngeal cancer. Increasingly, there is randomized trial evidence to support the use of neoadjuvant therapy or perioperative immunotherapy in several cancer types with survival-based endpoints. Very exciting indeed. Dr. Melvin Chua: Indeed, I couldn't agree with you more. I think one of the things that went into designing the case-based discussions this year was that we wanted to talk about cancers that were relevant to this part of the world and hence we again showcased lung cancers, gastric cancers and melanomas, and whereby we have again perspectives from an expert from the West coupled to an expert from the East, thereby showcasing the diversity of practice around the world. The other thing that we did this year was we decided to pair the case-based discussions with the keynotes and the Education Sessions as well. For example, on Day 3, we had Dr. Sakaguchi speak on Tregs, as you mentioned. And this was followed by an in-depth session on new immunotherapies, and then followed by a case-based discussion on different melanoma cases on the role of neoadjuvant immunotherapy in this disease, and the strikingly relevance of response to prognostication. This is an important trait that we're seeing now that seems to pan out across different cancers, where we find that neoadjuvant response to combination systemic therapies and/or radiotherapy is a strong prognosticator. Dr. Lillian Siu: So, Dr. Chua, we've discussed some breakthrough treatments and promising advances in cancer care, and we've touched upon some barriers to success in cancer treatment. I would like to ask you about the keynote address by Dr. Raffaella Casolino of the World Health Organization, who spoke passionately about efforts by the WHO and its partners to build equity in cancer care. Can you share some highlights with us? Dr. Melvin Chua: Absolutely, Dr. Siu. In spite of the tremendous advances we've seen in recent years in oncology, there are still major disparities in cancer care, such as cost and access, which affect patients worldwide. I think Dr. Casolino's talk was a very nice overview whereby she showed, first of all, the WHO's impact in terms of the WHO Cancer Resolution initiative that was implemented in 2017, where through this initiative, WHO has impacted 100 countries, invested $1 billion in funds, and that has led to millions of lives saved. But she then really drilled down to some of the key examples of the focus of the WHO in terms of equalizing care in cancer. I think one which struck me was the appreciation of the disparities in the clinical trials landscape. I think it is clear that there's still a huge barrier to clinical trials between the high- and middle-income countries and the low- and middle-income countries, and the majority of clinical trials these days are industry sponsored and we really need to look at leveling the playing field in this regard. Then she highlighted the WHO's work on trying to lower the barriers to precision oncology. And I think there are several issues in that sense, but I think what the WHO has really worked hard on is promoting education for genomic medicine, where they've done several reviews with experts around the world to educate the field across the world on how we interpret and apply genomics in the clinic. So all in all, it was very interesting to hear Dr. Casolino's insights from a policy perspective, and again, this emphasizes that there's so much work to be done at the end of the day and the dialogue needs to continue. We also heard about policy, academic and industry perspectives in the context of clinical trials, and that led to a discussion on real-world evidence generation for regulatory approvals. It was very nice that we had a session on that at the end of Breakthrough 2024 (Real-World Evidence and Clinical Trials: Beyond the Ivory Tower). And in that session, we heard from Dr. Shaalan Beg [of the NIH], and Dr. Janet Dancey [of Queen's University] who represented views from academia and Dr. Hidetoshi Hayashi [of Kindai University Hospital] shared perspectives on decentralized trials. I'd like to encourage our listeners to watch these sessions if they were unable to attend. The content is very rich, and I'm sure they'll learn from it. Dr. Lillian Siu: Thank you so much, Dr. Chua. Is there anything else you would like to cover before we wrap up the podcast today? Dr. Melvin Chua: Thank you, Dr. Siu. The thing I really want to emphasize is, apart from all these Educational Sessions and having very eminent keynote speakers, one of the key points that we really want to bring out for Breakthrough is to showcase the high-quality research. This year we had 300 abstracts submitted and they were all high quality, cutting across trials, omics research, AI and technology, and eventually we selected 235 of them and we were able to showcase some of them across three oral sessions over three days. I think this is an important component of Breakthrough that we really wish to continue building upon where people are now excited to use this forum to present their work. Dr. Lillian Siu: Thank you so much, Dr. Chua. I really enjoyed our discussions today. I look forward to seeing how the Breakthrough meeting will continue to grow in future years. Dr. Melvin Chua: Thank you again, Dr. Siu. Thank you for all your leadership and efforts in making Breakthrough a successful meeting series the past few years. Dr. Lillian Siu: Thank you to our listeners for your time today. You'll find links to the session discussed today in the transcript of this episode. Finally, if you value the insights that you hear on the ASCO Daily News Podcast, please take a moment to rate, review and subscribe wherever you get your podcast. Thank you. Disclaimer: The purpose of this podcast is to educate and to inform. This is not a substitute for professional medical care and is not intended for use in the diagnosis or treatment of individual conditions. Guests on this podcast express their own opinions, experience, and conclusions. Guest statements on the podcast do not express the opinions of ASCO. The mention of any product, service, organization, activity, or therapy should not be construed as an ASCO endorsement. Find out more about today's speakers: Dr. Lilian Siu @lillian_siu Dr. Melvin Chua @DrMLChua Follow ASCO on social media: @ASCO on Twitter ASCO on Facebook ASCO on LinkedIn Disclosures: Dr. Lillian Siu: Leadership (Immediate family member): Treadwell Therapeutics Stock and Other Ownership Interests (Immediate family member): Agios Consulting or Advisory Role: Merck, AstraZeneca/MedImmune, Roche, Voronoi Inc., Oncorus, GSK, Seattle Genetics, Arvinas, Navire, Janpix, Relay Therapeutics, Daiichi Sankyo/UCB Japan, Janssen, Research Funding (Institution): Bristol-Myers Squibb, Genentech/Roche, GlaxoSmithKline, Merck, Novartis, Pfizer, AstraZeneca, Boehringer Ingelheim, Bayer, Amgen, Astellas Pharma, Shattuck Labs, Symphogen, Avid, Mirati Therapeutics, Karyopharm Therapeutics, Amgen Dr. Melvin Chua: Leadership, Stock and Other Ownership Interests: Digital Life Line Honoraria: Janssen Oncology, Varian Consulting or Advisory Role: Janssen Oncology, Merck Sharp & Dohme, ImmunoSCAPE, Telix Pharmaceuticals, IQVIA, BeiGene Speakers' Bureau: AstraZeneca, Bayer, Pfizer, Janssen Research Funding: PVmed, Decipher Biosciences, EVYD Technology, MVision, BeiGene, EVYD Technology, MVision, BeiGene Patents, Royalties, Other Intellectual Property: High Sensitivity Lateral Flow Immunoassay for Detection of Analyte in Samples (10202107837T), Singapore. (Danny Jian Hang Tng, Chua Lee Kiang Melvin, Zhang Yong, Jenny Low, Ooi Eng Eong, Soo Khee Chee)
Dr. John Sweetenham shares highlights from Day 3 of the 2024 ASCO Annual Meeting, including selected studies on the treatment of cancer cachexia, surgical approaches in advanced ovarian cancer, and advanced colorectal cancer with liver metastases. TRANSCRIPT Dr. John Sweetenham: I'm Dr. John Sweetenham, the host of the ASCO Daily News Podcast, with my top takeaways on selected abstracts from Day 3 of the 2024 ASCO Annual Meeting. Today's selection features studies addressing the treatment of cancer cachexia and 2 studies of surgical approaches to the treatment of advanced ovarian cancer and of advanced colorectal cancer with liver metastases. My full disclosures are available in the transcript of this episode. Cachexia affects up to 80% of patients with advanced cancer and is thought to be directly responsible for 30% of cancer deaths, according to the National Cancer Institute. Despite these statistics, the condition remains understudied and there is no standard treatment. Current guidelines recommend dietary counseling and low-dose olanzapine or short courses of corticosteroids or progesterone analogues can be used to promote weight gain. However, the guidelines mainly point to evidence gaps. No drug therapy could be strongly endorsed to improve patient outcomes and no recommendations could be made regarding exercise. Dr. Tora Solheim from the Cancer Clinic at St. Olavs Hospital in Trondheim, Norway, today reported results from the MENAC trial in LBA12007, which tested an intervention that combined treatment with nonsteroidal anti-inflammatory medication ibuprofen, home-based exercise to improve endurance and muscle strength, nutritional counseling, and supplements containing omega-3 fatty acids, which, based on previous research, may enhance muscle mass in patients with cancer cachexia. This trial enrolled 212 patients with stage III or IV lung or pancreatic cancer from 17 sites in 5 countries. All patients were receiving palliative chemotherapy and either had cachexia or were at high risk of developing it. Half were randomly assigned to the intervention and half to standard care. For the exercise components of the intervention, patients were encouraged to engage in aerobic activity such as walking, swimming, or even household chores at least twice a week. They were also encouraged to perform strengthening exercises such as half squats, bicep curls, and knee lifts 3 times per week. Over 6 weeks, the trial found average body weight stabilized in the intervention group compared with a loss of 1 kg in the standard care group, but there were no differences between the two groups and the secondary endpoints of muscle mass and daily step count as measured by ActiGraph. Dr. Solheim pointed out that 6 to 8 weeks may be too early to observe any anabolic effects on muscle mass or function, but that this timeframe was chosen, she said, because previous studies, including her team's own feasibility study had encountered high dropout rates among similar patient groups after 6 to 8 weeks. Although these are interesting data, I think they also pose many questions: Is maintaining 1 kg of body weight a meaningful endpoint? Did the patients report any improvement in other symptoms? How was at-home exercise monitored for compliance? Did we know whether the patients were fulfilling adequate amounts of exercise? And there are many more questions. I think the investigators should be congratulated for demonstrating the feasibility of conducting a randomized trial in this challenging patient group, and this will hopefully provide a basis for future studies exploring new interventions. In LBA5505, Dr. Jean-Marc Classe presented data from the CARACO study, a randomized trial evaluating the use of retroperitoneal lymph node dissection in patients undergoing primary surgery or interval cytoreductive surgery after neoadjuvant chemotherapy for advanced epithelial ovarian cancer. To provide some context, an earlier study, the phase 3 LION trial, assessed the role of RPLD in patients with advanced ovarian cancer with complete resection and normal lymph nodes after primary surgery. In this trial, RPLD provided no significant improvement in overall or progression-free survival and was associated with a significant increase in serious postoperative complications and 60-day mortality. In recent years, the use of neoadjuvant chemotherapy and interval surgery has increased significantly in the U.S. and Europe, and it was unknown whether RPLD could have a benefit among these patients. The CARACO trial was undertaken to answer this question, enrolling patients treated with either primary surgery or neoadjuvant chemotherapy and interval surgery to reflect a real-world population. The multicenter trial enrolled 379 patients with FIGO stage III-IVA epithelial ovarian cancer with no suspicious retroperitoneal lymph nodes in whom optimal surgery was achievable with primary surgery or with interval cytoreductive surgery after neoadjuvant chemotherapy with residual tumor at less than 1 cm. Patients were randomly assigned to surgery with or without retroperitoneal lymph node dissection. Patients receiving primary surgery accounted for about 26% of the no RPL arm and 21% of the RPL arm. The primary endpoint was progression free survival, and secondary endpoints included overall survival, safety, surgical outcomes, and quality of life. Although the trial initially planned to enroll 450 patients, enrollment slowed after the presentation of the results of the Lyon trial, leading to a premature closing of this trial to enrollment with 379 patients. The median age of enrolled patients was 64 - 65 years and 87% had serous or endometrioid carcinoma. Surgery was performed with no residual tumor in around 86% of the patients in the no RPL arm and 88% of patients in the RPL arm. Importantly, the median duration of surgery was 240 minutes in those with no RPL versus 300 minutes in the RPL arm, representing an additional hour for those who underwent retroperitoneal lymph node dissection. Severe morbidity within 30 days of surgery was significantly improved in the no RPL arm compared with the RPL arm as assessed by rates of transfusion or blood loss, re-intervention, and urinary injury. In an intent to treat analysis, there was no significant difference in progression-free survival in patients who did or did not receive retroperitoneal lymph node dissection. The respective median progression-free survivals were 14.8 and 18.6 months. Median overall survival was 48.9 months and 58.8 months, respectively, and on subgroup analysis, no benefit for retroperitoneal lymph node dissection was observed. Although the results of this study are slightly confounded by the failure to reach their target accrual, the data shows strong evidence that these patients can be spared the additional surgery and subsequent surgical complications without compromising progression free or overall survival. Dr. Classe and his colleagues hope to determine whether retroperitoneal lymph node dissection is useful in patients with suspicious nodes. The third selected abstract today is 3500, which describes a remarkable prospective study of chemotherapy plus liver transplantation versus chemotherapy alone in patients with unresectable colorectal cancer liver metastases. The results of the so-called TRANSMET study were presented by Dr. Adam from Villejuif, France, on behalf of a study group including centers from France, Belgium, and Italy. In the introduction to the study, the presenter pointed out that liver resection is currently the optimal treatment for liver metastases from colorectal cancer and offers the potential for long-term survival and even cure. But resection is only possible in 10% to 20% of patients. And although cytoreductive chemotherapy may convert some patients to a resectable status, this is relatively rare. The current standard of care is the use of chemotherapy, which may prolong survival but is not curative. Liver transplantation has been used in this context since the 2000s with apparent improvements in outcome, but TRANSMET is the first randomized trial to assess the benefit of adding liver transplantation to chemotherapy in this patient group. The TRANSMET study evenly randomized 94 patients to either undergo chemotherapy and liver transplantation or only chemotherapy. The patients were highly selective in terms of age, performance status, resection of primary tumor, months of tumor control, previous line of therapy, and tumor markers. It's noteworthy that of the 157 patients eventually considered, 63 failed to meet the demanding eligibility criteria on the review of the trial committee. The 5-year overall survival rate in the intent to treat analysis was 57% in the chemotherapy plus liver transplant cohort and 13% in the chemotherapy-alone arm. Progression-free survival was 17.4 versus 6.4 months, respectively. 28 of the 38 transplanted patients suffered relapses, 15 of which were in the lungs. Surgical resection and/or radio ablation were used in many of these patients. The authors concluded that liver transplantation is an option which should be considered in this highly selective patient group and that the outcomes reported here are comparable to outcomes for liver transplantation and other conditions. Understandably, this is a small study in a highly selective group, and it's difficult to know where this will gain traction. With a shortage of organs for donation, prioritization of this small patient group may be challenging. That concludes today's report. Join me again tomorrow to hear more top takeaways from ASCO24. If you value the insights that you hear on the ASCO Daily News Podcast, please remember to rate, review, and subscribe wherever you get your podcasts. Disclaimer: The purpose of this podcast is to educate and to inform. This is not a substitute for professional medical care and is not intended for use in the diagnosis or treatment of individual conditions. Guests on this podcast express their own opinions, experience, and conclusions. Guest statements on the podcast do not express the opinions of ASCO. The mention of any product, service, organization, activity, or therapy should not be construed as an ASCO endorsement. Follow ASCO on social media: @ASCO on Twitter ASCO on Facebook ASCO on LinkedIn Disclosures: Dr. John Sweetenham: Consulting or Advisory Role: EMA Wellness
The Attorney General did not advise the Chief Minister to stay away from the criminal investigation into the alleged hacking of the National Security Information System in 2020. Michael Llamas KC accepted that - in hindsight - an angry meeting between himself, the Chief Minister and the Commissioner of Police should NOT have happened. Mr Llamas accepted he didn't ask himself: maybe I shouldn't be in the room for this. But he said it all happened very quickly as Mr Picardo was angry and Mr McGrail was in the building, so they got together. Ros Astengo was in the studio to discuss the latest on the Inquiry in more detail.And, the Health Authority will be holding its annual Skin Cancer Screening Day soon and is inviting the public to make the most of the opportunity. The Dermatology Team and a visiting Consultant Dermatologist will be on hand to look at any notable skin changes, which could indicate skin cancer. 400 appointments will be available on the 12th May at the Primary Care Centre, on a first come first served basis. We spoke to the Director of Public Health, Dr Helen Carter. Hosted on Acast. See acast.com/privacy for more information.
Episode 133: All About Matthew Kalady, MD, and the James Colorectal Cancer Clinic
Providing the best possible care in a timely manner for colorectal cancer patients is the goal of Matthew Kalady, MD, for the new James Colorectal Cancer Center. “Everything starts with a vision and our vision is to be the best,” he said. In this episode, Kalady discusses how he fell in love with surgery during medical school and eventually came to specialize in colorectal cancer; his research on how the genetics of a colorectal tumor impact their development, growth and response to treatment; and his goals for the new, multidisciplinary colorectal cancer center, which is one of the first in the country. “The James is adept at taking translational research in the lab to patients and I'm excited to be part of that,” Kalady said. He also talks about the cancer journey of his father, who eventually died from cancer of the appendix. “What I learned from the process and seeing him go through it drives how I want to take care of patients,” he said. “Every time I see a cancer patient, I think of him.”
Breast cancer is the most common cancer diagnosis in women in the United States and currently accounts for the second most cancer deaths in women behind lung cancer. More than 260,000 diagnoses of breast cancer are made each year in this country. Advances in screening techniques and identifying who may be at higher risk for the development of breast cancer has allowed us to provide more targeted screening recommendations for our patients. In this episode of the All In Against Cancer podcast, we talk with Ochsner breast oncology nurse practitioners Erica Doubleday and Peggy Jo Alker to learn more the importance of and services provided by Ochsner's high risk breast cancer clinic.
The risk of breast cancer is identifiably higher for some people than it is for others. Those high-risk people require customized and specialized care, a form of high-risk breast cancer service. In this episode of the BayCare Clinic podcast, Dr. Natalie Luehmann, a breast surgeon with Aurora BayCare General & Vascular Surgery, discusses Aurora BayCare's High-Risk Breast Cancer Clinic, designed to aid those at higher risk of developing breast cancer. For more information about BayCare Clinic visit: https://baycare.clinic/2SkVAoD For more information about Aurora BayCare General & Vascular Surgery, visit: https://baycare.clinic/3B80KL6 For more information about Dr. Natalie Luehmann visit: https://baycare.clinic/3xAZPBg Find BayCare Clinic on Facebook: https://baycare.clinic/2g4hDFB Find BayCare Clinic on Twitter: https://baycare.clinic/2uMlLTW Find BayCare Clinic on LinkedIn: https://baycare.clinic/2SkC0Zx Find BayCare Clinic on YouTube: https://baycare.clinic/2vGO7YT
Tokyo Alumni Podcast: Episode 73- Dr. Minako Abe, M.D. (ASIJ 1988) - Director of Tokyo Cancer Clinic
Minako Abe, M.D. (ASIJ 1988) Director of the Tokyo Cancer Clinic Minako Abe is the director of the Tokyo Cancer Clinic in Japan. She attended ASIJ from 1976-1988 and after graduating, attended UC Berkeley for her B.A. and earned her M.D. at SUNY Stony Brook. She has dual U.S. board certifications in Emergency Medicine and Lifestyle Medicine. Practicing Emergency Medicine in NYC and NJ for over 15 years, she loved treating all kinds of illnesses and people from all walks of life, but found that nearly 80% of what she saw was related to unhealthy lifestyle choices. Chronic illnesses such as obesity, diabetes, stroke, heart disease, and even 30-50% of cancers are preventable. As such, she developed a strong interest in Lifestyle Medicine, particularly in relation to the field of immunology and oncology. In 2014, she and her family moved to Tokyo to help with her father's cancer immunotherapy clinic. Having lived outside of Japan for 26 years, she experienced a bit of culture shock, having to relearn Japanese and understanding a completely different medical system. However, with both of her children currently attending ASIJ, this has given her family a sense of belonging within this very special international community.A year into moving here, her husband was diagnosed with a rare spinal cord tumor, and when searching for the best treatment options in the U.S., she was surprised to find that the most advanced treatment options were actually right here in Japan. Even the patented cancer vaccines and immune cell treatments at the Tokyo Cancer Clinic is not widely known or available elsewhere in the world! This experience got her thinking – how isolating it is for expats in Japan to go through a cancer diagnosis while also navigating a foreign medical system. How are people to know that perhaps the best treatments and opportunities lie right here? Her passion project is to help cancer patients navigate the Japanese medical system, while coaching them to thrive and not just survive with Lifestyle Medicine and Mindset. You can find her at https://tokyocancerclinic.jp/ https://www.drminako.com/ Timeline 1:44 - Introduction 4:32 - Choosing the career path to become a doctor (from an international school student's perspective) / to work in Japan/USA? 10:50 - Can certain products "give you cancer"? 15:23 - Family history - nature v nurture when it comes to cancer? 17:37 - Sleep! 19:30 - Living in both Japan and the USA for 20+ years, a comparison of the two locations 25:04 - Comparing the perspective of ASIJ as a student vs as a parent 31:31 - What is to come
Episode 8 features Megan Hohl, Nurse Practitioner with Sparrow's High-Risk Cancer Clinic and she discusses what the High-Risk Cancer Clinic is and what services it provides for individuals at high risk for every type of cancer, including breast cancer.
Dr. Steven O’Day is the Executive Director of the John Wayne Cancer Institute and Cancer Clinic, and Director of Providence Los Angeles Regional Research. Today, Christina talks with Dr. O'Day to learn about some of the clinical trials that are taking place to combat COVID-19. He also reveals some of the more promising drugs researchers are looking at that could get us closer to solving this crisis, and he also addresses recent headlines regarding drugs like hydroxychloriquine and Gilead’s remdesivir.
Podcast #28: High Risk Breast Cancer Clinic: What Does it Mean? with Jennifer Davis
Who exactly is at an elevated risk for acquiring breast cancer within their lifetime, and what can they do about it? Information is meant to empower us; and early detection saves lives. Since patients who are at a high risk for developing breast cancer (above 20% lifetime risk) should discuss this with their providers and+ Read More
Health Suites: Surviving Breast Cancer in a Modern Age
Join Claressa Monteiro, as she speaks to Dr Lo Soo Kien, Medical Oncologist, The Harley Street Heart & Cancer Clinic, Mount Elizabeth Novena Hospital about her professional medical perspectives about Breast Cancer as well as her solutions to reduce the risks of getting struck by it.
Improving Timeliness of Oncology Assessment and Cancer Treatment through Implementation of a Multidisciplinary Lung Cancer Clinic
Hello, and welcome to the ASCO Journal of Oncology Practice Podcast. This is Dr. Nate Pennell, medical oncologist at the Cleveland Clinic and consultant editor for the JOP. On this month's podcast, we're going to be talking about a new study from the JOP Quality and Action series, titled Improving Timeliness of Oncology Assessment and Cancer Treatment Through Implementation of a Multidisciplinary Lung Cancer Clinic, published online in the JOP, January, 2019. Joining me today on this podcast is the author, Dr. Genevieve Digby, assistant professor in the division of respirology at Queen's University School of Medicine, where she's also the clinical lead for the lung diagnostic assessment program. She has an active interest in quality improvement projects, which is what led to this paper that we're going to be discussing today. Dr. Digby, thank you for joining me. Thank you so much for the invitation. Obviously, everyone likes to be seen as quickly as possible when they're trying to get into the doctor, but can you give us just a little bit of background into what led you to do this particular quality project? Why is the timeliness of care more important for cancer patients or, specifically, lung cancer patients? So great questions, Nate. Timely care is very important for patients, as you pointed out. In fact, the Institute of Medicine has timeliness as one of the six dimensions of quality. And for lung cancer patients this is particularly important, as we know that there's evidence to show that patients who have delays in their diagnosis or delays in treatment, that this is associated with progression of disease, and there's evidence to show that more advanced disease is associated with worse outcomes. And as we know from the lung cancer screening trials, earlier detection of disease is associated with better outcomes. Not only is timeliness of care important for patients from the point of view of getting their treatment underway, but it also is important in terms of the anxiety and distress that patients have. So we know that the longer delays are associated with more distress, and lung cancer patients to begin with are some of the patients who have the highest levels of anxiety and distress amongst oncology patients. So for us, the study arose because of an identification locally that there were delays in our care processes in regards to transitioning patients from the diagnostic phase of the lung cancer pathway to the treatment phase and a desire to improve those care processes. I think that that really resonates with me. I know at my institution we've been paying attention to the time to initiate treatment for a while, and it's not like going to see the dermatologist. When you're diagnosed with cancer, you really have a lot of anxiety, and you want to get in to get treatment as quickly as possible. And of course, as you've mentioned, especially for early stage lung cancer, there's pretty good data suggesting that the longer someone waits to make a diagnosis, the more likely they are to have their potentially earlier stage cancer turn into a later stage cancer with worse outcomes. So I applaud you for addressing this. And in your particular project, you focused on the establishment of a multidisciplinary clinic. And this is something where I think a lot of the literature out there on looking at processes and time to treatment has focused on that. So is there data suggesting that multidisciplinary clinics specifically are a good intervention for improving timeliness of care? So that's a good question. And the literature varies in terms of its robustness based on the type of cancer that we look at. So my group published a systematic review looking at multidisciplinary clinic models in lung cancer specifically. And we were surprised, actually, by the relative paucity of data in terms of what the optimal catalytic characteristics are, even just in terms of the number of studies that's actually evaluated a multidisciplinary clinic, per se. In other cancer types, there is evidence that multidisciplinary clinics lead to better collaboration between specialists. There is some evidence, even in lung cancer, that perhaps there's better compliance with staging guidelines and guideline-based care when care is delivered in a multidisciplinary clinic. And there's also some evidence, though limited again, especially for lung cancer, surrounding the patient experience and patient satisfaction with their care when it's delivered in a multidisciplinary clinic model. Yeah. Honestly, I don't think I've ever heard anyone argue that there's a downside to a multidisciplinary clinic. But I do appreciate studying measurable metrics that may demonstrate benefits because, of course, you have to get support for these sorts of things. So why don't you take me through your project's design, and what were the goals that you tried to achieve? So this is a quality improvement study. We started by identifying what our overall goals and outcome measures were and how we would go about achieving those goals. For us, the focus was to improve our transitions from the point of care of receiving a diagnosis of lung cancer through to starting treatment with an oncologist. So this particular setup was due to the fact that in our center we have a separate thoracic surgery program where patients with suspected early stage disease directly go to a thoracic surgery program and those with more advanced disease or suspected non-operable disease are initially managed by a respirologist, and then are seen through with the appropriate thoracic oncology specialist subsequently. So for us, we looked at our data, and we actually identified that that time from transition, where a patient receives a diagnosis of lung cancer, to when they're first assessed by an oncologist was upwards of about two weeks. The time then to go on and start their first treatment for cancer was in the range of 40 to 45 days. And we identified that there was room to improve and set a target of reducing both of these individual time frames by about 10 days. We hypothesized that if it could improve timeliness to seeing an oncologist from about 14 days to closer to 4 days-- 3 to 4 days-- that we would similarly lead to maybe about a 10-day improvement in time to treatment on the other end. So our improvement plan was to launch this multidisciplinary clinic. And we used a quality improvement called plan, do, study, act cycles, or PDSA cycles, to help facilitate that and fine-tune our multidisciplinary clinic along the way to make it even more efficient. That sounds great. It sounds like a very worthy project. So what did you find? We found that by implementing a multidisciplinary clinic, even within a very short time of implementing it, that we were able to significantly reduce the time from a patient's lung cancer diagnosis to when they were first assessed by an oncologist. In fact, just with the implementation of the clinic, we led to about a 10-day improvement. We fine-tuned our processes to help create sustainability of the teams. Initially, there was still some variability. And we were able to maintain about a 10-day improvement overall over time. What we found though, and what was really interesting, was that as we went about our change processes, we had ongoing improvement in time to treatment, so that time from lung cancer diagnosis to time to first treatment. With our initial clinic implementation, we had about a 10-day improvement in time to treatment as well. But as we noticed, as we fine-tuned our processes, that improvement actually increased such that we overall reduced time to treatment from about 40 days at baseline to 15 to 20 days by the end of our quality improvement initiative. And that is incredible. I think, to me, was the most impressive thing is not so much that you, by moving up your evaluation by 10 days, you improved time to treat by 10 days, which makes perfect sense, but that somehow implementing this entire project, you greatly exceeded your expected improvement in time to treat. And so, did you look at what specific interventions might have led to that even better improvement than you expected? So that's a great question. And as you said, what surprised us was the extent to which timeliness, in terms of receiving first treatment improved, even beyond just time to seeing an oncologist. And when we considered the data, some of the things that came out were likely the increase in collaboration that we were seeing amongst specialists, particularly medical and radiation oncologists in terms of being able to decide on a treatment plan a bit sooner and get that plan up and running. In fact, when we looked at the data, the patients that had the greatest improvement in time to treatment were those with stage 2 and 3 lung cancer, and also including patients with stage 4 lung cancer. And those are often-- especially stage 2 and 3-- where patients are most likely to need a concurrent chemoradiation, where the treatment plans are often decided together amongst the radiation oncologist and the medical oncologist. And so having that ability to discuss the treatment plans and come up with a clear plan sooner is what we hypothesized is leading to be faster kind of treatment. To evaluate this further, we actually also have recently completed a qualitative study, where we interviewed physicians, and including patients and caregivers, about the impact of a multidisciplinary clinic. And while I don't want to give away all the results yet before it's published, one of the themes that comes up certainly for the physicians and particularly oncologists is just the overall ability to collaborate and have real-time discussions with each other and with the patients about what their treatment plans would be, leading to a faster implementation of that plan. Well there you go, listeners. You're getting a sneak peek of a future study going to be coming out of this group. But I think that makes perfect sense. So again, as a group that has, at least internally, been focusing on improving our time to getting patients to treatment, I think just having an emphasis on studying how long it takes to treat and that everyone understanding that it's a priority to try to make that as short as possible seems to just lead to improvements because everyone's aware that it's an important aspect of treatment. And things tend to show improvements without any real specific interventions taking place. And then, of course, the multidisciplinary clinic. It makes perfect sense that multidisciplinary care would be better coordinated. So I think that that's a really nice validation of what you were trying to do. So how would other centers that maybe are starting to look at this, how would they take what you've done and apply it to their own programs? So that's a great question. I think there's a few things to consider. Firstly, quality improvement processes can be instituted in any organization. And part of quality improvement is identifying what the main barriers are to achieving the timeliness of care goals that an individual center has and just implementing the PDSA cycles at their own institution to help achieve those targets because the barriers can be different between different organizations. So where possible, I think eliminating the silos that exist in our care models of the traditional model of seeing one person at a time and really trying to get people to work together, that can be challenging administratively. But once those barriers are overcome, it's actually more convenient for people to really work collaboratively to improve patient care as a whole. That's great. And this really fits in nicely with both the US National Cancer Institute and ASCO, in particular, have really paid a lot of attention in recent years to teamwork and building team science to help improve outcomes. And I think that your study is a wonderful example of how that can lead to direct and measurable improvements in care. Well, thank you. We certainly think that we've led to some improvement locally and hope that other centers can learn from what we've learned to help drive change. Dr. Digby, thank you so much for talking with me today about your study. And I really want to thank you for sharing the results of your project because I think high quality quality improvement projects that are going on all over the world, really, but oftentimes don't get shared outside of the individual team or institution where they're doing them. And this is going to allow, hopefully, a lot of people to see how investments in teamwork and trying to improve on these metrics can lead to really important results for our patients. I completely agree. It's important to share the knowledge that's learned, particularly with quality improvement. We're all working towards common goals for delivering better patient care, and it's great to be able to share those learned experiences with others. And I also want to thank our listeners out there who joined us for this podcast. The full text of the paper was published online at ascopubs.org/journal/jop on January 7, 2019. This is Dr. Nate Pennell for the Journal of Oncology Practice signing off.
CHEMO IS THE INVISIBLE THREAT TO CANCER CLINIC STAFF
IT HAS LONG BEEN KNOWN THAT HANDLING AND ADMINISTERING CHEMOTHERAPY IS A HEALTH HAZARD FOR CANCER CENTER CLINIC STAFF, ESPECIALLY NURSES AND PHARMACIST OWING TO ITS POTENT TOXICITY. SO CAN ONE BE PROTECTED? TUNE IN FOR DETAILS.
Episode 22: The Spielman High-Risk Breast Cancer Clinic with Doreen Agnese
Doreen Agnese, MD, is the director of the Stefanie Spielman Comprehensive Breast Cancer Center's High-Risk Breast Cancer Program here at the James. Dr. Agnese and her team use genetics, screenings, early detection and advances in research & treatment to save a lot of lives.
Mastodons Men's Basketball Coach Jon Coffman Previews 2018 Coaches vs. Cancer Clinic
The University of Purdue-Fort Wayne Mastodons men's basketball coach Jon Coffman joins the show to preview their 2018 Coaches vs. Cancer clinic and more.
RebuiltU #49 Great Mexico Cancer Clinic
You can’t afford to NOT know about this secret Mexican clinic. This is about the most dangerous thing you might face in your life. I was talking to a patient yesterday about this email and I said “statistically” 1 in 2 males gets this. “That means either you or I will get cancer”. He laid there thinking for a minute. Then I told him 1 in 3 women get cancer. He asked me if that was ALL types. It is. When you think about it, that’s really what matters. Cancer is cancer, no matter where it is. I have something very special for you today. I sat down with a long time friend, Dr. Shetlin, and we talked about cancer as husbands and fathers and not as doctors. Why would we do that? Most of you know, I write a lot about breast cancer this time of year. I help out a breast cancer charity for survivors, and I’ve lost two close relatives to cancer. I will likely lose another relative very soon. Dr. Shetlin’s wife is currently battling cancer and he was kind enough to sit down with me and talk about it and the alternative treatments they are doing. We talk about the clinic she is going to, in Mexico, and why? We talk about the treatment she is getting. We talk about why it was the best option. Most importantly, we talk a lot about what you can do, right now, to improve your life. This is an hour interview of information on the most important health topic of our time. Neither of us treats cancer, but both of us know a lot about prevention and being proactive in your life. Remember, 1 in 2 males, and 1 in 3 females will face cancer. That puts a lot of gravity on this topic.
Combination therapies pairing conventional treatments, such as radiation and chemotherapy, with metabolic, dietary strategies offer a number of advantages to the cancer patient, including reduced side effects and improved outcomes. Dr. Dawn Lemanne, a board-certified medical oncologist, describes her care model using this integrative therapeutic approach and provides practical advice for patients.
Inside controversial Mexican cancer clinic and woman mauled by shark in Botany Bay: News Wrap February 25
Kristen Tsiamis with the top stories for Sunday February 25 See acast.com/privacy for privacy and opt-out information.
012: Healing Home vs Cancer Clinic… And Fruit vs. Keto!: Terry Tillaart
Terry Tillaart has helped thousands of people make their way through a cancer diagnosis to the other side to good health. He tells us the approach he’s developed over the years to help maximize your budget, no matter what it is, and really make every dollar count in addressing the fundamentals of healing from cancer. Terry is also very big on a “species appropriate diet” and tells us why we should not only not be afraid of natural whole food fruit sugars, but get as much of them as we can! For more cancer healing and preventing: www.mykidcurescancer.com www.youtube.com/mykidcurescancer www.facebook.com/mykidcurescancer To support our work: www.mykidcurescancer.com/crowdsponsor Terry Tillaart graduated with a PhD in Natural Medicine in 2016, an accomplishment he is proud of, that however was really viewed as a formality given results, not credentials are what matter and he has been educating people for 15 years. He has produced many great seminars including a North American Speaking Tour called “Cancer: The Fear Ends Here” that reached thousands of people. He has shared the stage with many prominent experts and is also a featured expert in an upcoming documentary on cancer again alongside many other international experts on the subject. He has created multiple health programs and has successfully taught people how to strategically heal from many health challenges including Cancer, Autism, Rheumatoid Arthritis and many more by focusing on results and proper testing.
Prostate cancer is the most common cancer among Canadian men
Cars and Cancer Podcast 3: Prostate Cancer Prostate cancer is not an easy topic for most men to discuss. This episode of cars and cancer features Dr. Michael Brundage our regional expert on prostate cancer who is also a researcher, professor at Queens and practices at the Cancer Clinic of South Eastern Ontario. We will also speak to Ike a patient who explains his own journey after a prostate diagnosis. Prostate cancer is one of the most curable forms of cancer if caught early and treated.
Learning about Our Ancestor, Part 11: Mrs. Maud Proudfoot’s Service Above Self
Born July 5,1893 in Colon, Panama, as 1st-born to Emma Blake & John Brouwer, Mrs. Maud Virginia Brouwer Proudfoot came to the Virgin Islands as a very young child. Married March 3, 1918 to Leslie Proudfoot, Mrs. Proudfoot started her career of public service in the 1920's with the American Red Cross, where she began her life of social work. Appointed by Gov. Paul M. Pearson July 1, 1933 as the first and only social worker in the newly established Dept. of Social Welfare, where she served in various capacities until she retired in 1963. For more than 60 years and for as long as she was able, Mrs. Proudfoot devoted her personal and professional life to those in need. Even though she considered herself a humble servant of the needy, her untiring commitment to the betterment of her fellow man resulted in an outstanding life's work. Most important to her were the times she could spend encouraging and supporting the elderly and the shut-ins; arranging a dignified burial for those who died without family or loved ones; reading and writing letters for the illiterate; accompanying patients to the Cancer Clinic in Puerto Rico; and lending an empathetic ear to those in need of counseling. Her life has been a testimony to her personal credo: “He has shown you, O mortal, what is good. And what does the Lord require of you? To act justly and to love mercy and to walk humbly with your God.” ~ Micah 6:8 (The New International Version)
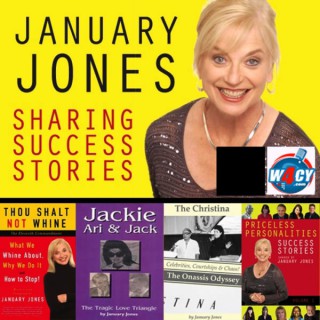
January Jones-Smiles From Cancer Clinic
Rajiv Samant is the author of: Smiles From The Clinic: A Humorous Look At Cancer. At present, he lives with his children in Ottawa where he practices as a Radiation Oncologist. He continues to see patients at The Ottawa Hospital Cancer Centre, and teaches in the Faculty of Medicine at the University in Ottawa (Canada). As a teacher, educator and researcher interested in improving how we deal and communicate with patients and their families.www.smilesfromtheclinic.comThis show is broadcast live on W4CY Radio (www.w4cy.com) part of Talk 4 Radio (http://www.talk4radio.com/) on the Talk 4 Media Network (http://www.talk4media.com/).
Skin Cancer Clinics - Sales and marketing strategies that will enable a skin cancer clinic to grow
✔What Would We Do✔ - Niche Specific Sales & Marketing Inspiration - ✔Be Inspired✔
This episode of What Would We Do, delves into Skin Cancer clinics in Queensland.It profiles some learnings from a highly successful marketing campaign for a Qld skin cancer clinic as well as provides ideas and inspirations that Skin cancer clinics should consider and use to boost revenue as well as provide a broader service to the patients they serve. David Twigg and Chris Bugden deliver an insightful discussion that will inspire you and arm you with new ideas.
How to Live Cancer Free – “Defeat Cancer by Connie Strasheim”
Bill Henderson interviews Connie Strasheim, author of a very informative book called Defeat Cancer. Connie has interviewed 15 holistic cancer doctors. All but one of them run clinics in 5 countries where they treat cancer patients with various natural treatments. Reading this book is like taking a tour of all these clinics in the U.S., Denmark, Mexico, Germany and … Read more about this episode...
How to Live Cancer Free – Understanding Radiation Hormesis
Bill Henderson discusses Cancer-in-the-News: Vitamin D3 and radiation hormesis. Are these the “wonderful new Cancer treatment” they’re cracked up to be? Bill then interviews Andy Scholberg, a freelance writer who has toured Cancer clinics in Mexico, Germany and the U.S. and written three e-books about his experiences; Cancer Defeated, Cancer Breakthrough USA, and German Cancer Breakthrough. Andy … Read more about this episode...
Dr. Eric Topol explains how the cancer clinic of the future will look.
Drs. Ross Camidge and Corey Langer: Which New Targets and Therapies Could We Bring to the Lung Cancer Clinic in the Near Future?
Drs. Ross Camidge and Corey Langer offer their perspectives on the most encouraging emerging targets that could become valuable additions to our lung cancer treatment menu in the next several years.
Drs. Ross Camidge and Corey Langer: Which New Targets and Therapies Could We Bring to the Lung Cancer Clinic in the Near Future?
Drs. Ross Camidge and Corey Langer offer their perspectives on the most encouraging emerging targets that could become valuable additions to our lung cancer treatment menu in the next several years.
Drs. Ross Camidge and Corey Langer: Which New Targets and Therapies Could We Bring to the Lung Cancer Clinic in the Near Future?
Drs. Ross Camidge and Corey Langer offer their perspectives on the most encouraging emerging targets that could become valuable additions to our lung cancer treatment menu in the next several years.
Multidisciplinary Prostate Cancer Clinic - March 8, 2010
Guest: Joseph Herman, MD Host: Lee Freedman, MD Dr. Herman discusses this impressive program available to patients who have been diagnosed with pancreatic cancer. In a single day, patients get diagnostic studies and recommendations for treatment from a multidisciplinary group of experts in the field.