Podcasts about metastatic
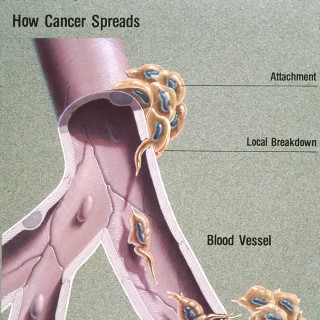
Spread of a disease inside a body
- 438PODCASTS
- 2,104EPISODES
- 30mAVG DURATION
- 5WEEKLY NEW EPISODES
- Mar 2, 2026LATEST
POPULARITY
Categories
Best podcasts about metastatic
Latest news about metastatic
- Oncolytics (ONCY) Initiates Phase 2 Trial for Metastatic Colorectal Cancer GuruFocus New Articles - Mar 2, 2026
- SystImmune and Bristol Myers Squibb Highlight Positive Phase III Interim Topline Results for izalontamab brengitecan (Iza-bren) in Previously Treated Unresectable Locally Advanced or Metastatic Triple-Negative Breast Cancer Drugs.com - Clinical Trials - Feb 26, 2026
- Combined Photothermal and mTOR‐Targeted Therapy Overcomes Immune Evasion and Enhances Checkpoint Blockade Efficacy in Metastatic Triple‐Negative Breast Cancer (Adv. Sci. 10/2026) Wiley: Advanced Science: Table of Contents - Feb 18, 2026
- Triple negative breast cancer cells use new strategy to boost metastatic ability The Medical News - Feb 6, 2026
- Salmonella Bacteria Membrane‐Fusion Paclitaxel Loaded Liposomes for Enhanced Therapy of Intraperitoneal Metastatic Ovarian Cancer Wiley: Advanced Healthcare Materials: Table of Contents - Jan 30, 2026
- Revolt in Trump's DOJ is 'metastatic and spreading quickly': expert Raw Story - Celebrating 18 Years of Independent Journalism - Jan 13, 2026
- Pfizer’s BRAFTOVI combination boosts response rates in metastatic colorectal cancer Breaking News on Seeking Alpha - Jan 12, 2026
- Seamlessly Overcoming Biological Barriers with a Small Photosensitizer to Treat Metastatic Tumors with Photodynamic Therapy Wiley: Angewandte Chemie International Edition: Table of Contents - Dec 31, 2025
- Mum diagnosed with metastatic cancer after finding lump on her neck The Independent - Dec 22, 2025
- Pyxis Oncology, Inc. (PYXS) Discusses Preliminary Phase 1 Data for MICVO in Recurrent and Metastatic Head and Neck Squamous Cell Carcinoma Transcript Seeking Alpha - Dec 18, 2025
Latest podcast episodes about metastatic
Episode 374: RERUN: Episode 374: Choices to Lower Breast Cancer Risk
Everyone is at risk of breast cancer. Some are more at risk than others due to hereditary factors – such as a family history of cancers – and lifestyle choices that affect our overall health. Knowing your risk of breast cancer can help you decide what steps to take to lower your risk. Joining me today is Dr. Jennifer Ligibel, a Susan G. Komen Scholar and Komen grantee, Professor of Medicine at Harvard Medical School, Senior Physician at the Dana-Farber Cancer Institute and an expert on the impact of lifestyle factors, cancer risk and outcomes. Through more than a dozen lifestyle intervention trials, Dr. Ligibel has evaluated the impact of exercise, weight loss, fitness, body composition and quality of life in cancer patients and survivors.
S16 Ep15: Six-Year CheckMate 9LA Data Reinforce Durable Survival in Metastatic NSCLC: With David Carbone, MD, PhD
In today's episode, we spoke with David Carbone, MD, PhD. Dr Carbone is a professor of internal medicine at The Ohio State University, co-leader of the Translational Therapeutics Program and director of the Thoracic Oncology Center at the Ohio State University Comprehensive Cancer Center–James, as well as the Barbara J. Bonner Chair in Lung Cancer Research in Columbus.In our exclusive interview, Dr Carbone discussed the 6-year data from the phase 3 CheckMate 9LA trial (NCT03215706), which not only reaffirmed the durability of benefit with nivolumab (Opdivo) plus ipilimumab (Yervoy) and chemotherapy but also highlighted particularly strong outcomes in historically poor-prognosis subgroups, including patients with PD-L1–negative tumors and those with squamous histology. Carbone also underscored the safety and tolerability of the regimen. Although dual immunotherapy carries higher toxicity than monotherapy, no new safety signals emerged at 6 years. Carbone also addressed the limitations of current biomarkers. Although PD-L1 remains the primary tool guiding immunotherapy decisions, it is an imperfect predictor.
S16 Ep11: Treatment Evolutions Affect First-Line Chemotherapy Selection in Metastatic Pancreatic Cancer: With Rachna T. Shroff, MD, MS, FASCO; and Kristen Spencer, DO
Welcome to OncLive On Air®! I'm your host today, Courtney Flaherty.OncLive On Air is a podcast from OncLive®, which provides oncology professionals with the resources and information they need to provide the best patient care. In both digital and print formats, OncLive covers every angle of oncology practice, from new technology to treatment advances to important regulatory decisions.In today's episode, Rachna T. Shroff, MD, MS, FASCO, and Kristen Spencer, DO, sat down with OncLive to discuss treatment goals and other patient factors weighed when navigating first-line chemotherapy selection in metastatic pancreatic cancer.Shroff is the associate director of clinical investigations and co-leader of the Gastrointestinal Clinical Research Team at the University of Arizona Comprehensive Cancer Center in Tucson. She also is a professor with tenure in the Department of Medicine, chief of the Division of Hematology and Oncology for the University of Arizona College of Medicine – Tucson, and medical director for the Oncology Service Line with Banner Health. Spencer is a medical oncologist and director of the Phase 1 Program at the New York University Langone Perlmutter Cancer Center.In the exclusive interview, Drs Shroff and Spencer discuss the evolving role of NALIRIFOX within the frontline treatment paradigm; the decision between standard first-line chemotherapy and clinical trial enrollment for patients with metastatic pancreatic cancer; and the importance of mentorship and leadership development for women in the field of gastrointestinal oncology._____That's all we have for today! Thank you for listening to this episode of OncLive On Air. Check back throughout the week for exclusive interviews with leading experts in the oncology field.For more updates in oncology, be sure to visit www.OncLive.com and sign up for our e-newsletters.OncLive is also on social media. On X and BlueSky, follow us at @OncLive. On Facebook, like us at OncLive, and follow our OncLive page on LinkedIn.If you liked today's episode of OncLive On Air, please consider subscribing to our podcast on Apple Podcasts, Spotify, and many of your other favorite podcast platforms,* so you get a notification every time a new episode is posted. While you are there, please take a moment to rate us!
Episode 373: HER: Beyond Biology: How Inequity Drives Breast Cancer Risk for Black Women
Today, in honor of Black History Month, we're exploring what happens when inequity itself becomes a risk factor for breast cancer in the Black community — shaping who gets screened, how quickly they're diagnosed and, ultimately, who survives. Our guest, Dr. Lori Pierce, is a renowned radiation oncologist, former ASCO president and Komen Scholar, and national leader in advancing equity in cancer care. She has dedicated her career to improving outcomes of women with breast cancer, with a focus on the underserved, by transforming not just treatments but the systems that deliver them. Her perspective is rigorous, compassionate and urgently needed.
Metastatic Hormone Receptor Positive (HR+) Breast Cancer Treatment Algorithm: Dr. Kevin Kalinsky
In this episode of the Oncology Brothers podcast we navigated the rapidly evolving treatment landscape of Metastatic Hormone Receptor-Positive Breast Cancer. We were joined by Dr. Kevin Kalinsky, Director of the Breast Cancer Program at the Winship Cancer Institute, Emory University, to discuss the implications of new targeted therapies, optimal sequencing strategies, and practical toxicity management. Listen us on: Spotify: https://open.spotify.com/show/31BXhY9FM4gPWG10WgE11o Follow us on social media: • YouTube: https://www.youtube.com/@oncologybrothers • X/Twitter: https://twitter.com/oncbrothers • Instagram: https://www.instagram.com/oncbrothers • Website: https://oncbrothers.com/ The discussion covered: • The critical role of NGS testing (tissue vs. liquid biopsy) in identifying PIK3CA, ESR1, AKT1 and PTEN alterations. • Frontline management of high-risk, endocrine-resistant disease with the inavolisib triplet (INAVO120) and its overall survival benefit. • Choosing between CDK4/6 inhibitors (abemaciclib vs. ribociclib) in de novo metastatic disease. • Post-CDK4/6 inhibitors on progression we covered, the use of oral SERDs (imlunestrant) and AKT inhibitors (capivasertib). • The "ADC explosion", sequencing T-DXd (DESTINY-Breast06), sacituzumab govitecan (TROPiCS-02), and datopotamab deruxtecan (TROPION-Breast01). • Clinical pearls for managing toxicities: stomatitis, hyperglycemia, rash, neutropenia, and ILD. Join us as we break down the latest data and provide actionable insights for the practicing oncologist. Don't forget to subscribe for more episodes in our breast cancer algorithm series! #MetastaticBreastCancer, #HRPositive, #ADCsequencing, #PIK3CA-AKT, #OncologyPodcast, #OncologyBrothers
ctDNA in Metastatic Invasive Lobular Carcinoma
JCO PO author Dr. Foldi at UPMC Hillman Cancer Center and University of Pittsburgh School of Medicine shares insights into the JCO PO article, "Personalized Circulating Tumor DNA Testing for Detection of Progression and Treatment Response Monitoring in Patients With Metastatic Invasive Lobular Carcinoma of the Breast." Host Dr. Rafeh Naqash and Dr. Foldi discuss how serial ctDNA testing in patients with mILC is feasible and may enable personalized surveillance and real-time therapeutic monitoring. TRANSCRIPT Dr. Rafeh Naqash: Hello, and welcome to JCO Precision Oncology Conversations, where we bring you engaging conversations with authors of clinically relevant and highly significant JCO PO articles. I am your host, Dr. Rafeh Naqash, podcast editor for JCO Precision Oncology and Associate Professor at the OU Health Stephenson Cancer Center at the University of Oklahoma. Today, we are thrilled to be joined by Dr. Julia Foldi, Assistant Professor of Medicine in the Division of Hematology-Oncology at University of Pittsburgh School of Medicine and the Magee-Womens Hospital of the UPMC. She is also the lead and corresponding author of the JCO Precision Oncology article entitled "Personalized Circulating Tumor DNA Testing for Detection of Progression and Treatment Response Monitoring in Patients with Metastatic Invasive Lobular Carcinoma of the Breast." At the time of this recording, our guest's disclosures will be linked in the transcript. Julia, welcome to our podcast, and thank you for joining us today. Dr. Julia Foldi: Thank you so much for having me. It is a pleasure. Dr. Rafeh Naqash: Again, your manuscript and project address a few interesting things, so we will start with the basics, since we have a broad audience that comprises trainees, community oncologists, and obviously precision medicine experts as well. So, let us start with invasive lobular breast carcinoma. I have been out of fellowship for several years now, and I do not know much about invasive lobular carcinoma. Could you tell us what it is, what some of the genomic characteristics are, why it is different, and why it is important to have a different way to understand disease biology and track disease status with this type of breast cancer? Dr. Julia Foldi: Yes, thank you for that question. It is really important to frame this study. So, lobular breast cancers, which we shorten to ILC, are the second most common histologic subtype of breast cancer after ductal breast cancers. ILC makes up about 10 to 15 percent of all breast cancers, so it is relatively rare, but in the big scheme of things, because breast cancer is so common, this represents actually over 40,000 new diagnoses a year in the US of lobular breast cancers. What is unique about ILC is it is characterized by loss of an adhesion molecule, E-cadherin. It is encoded by the CDH1 gene. What it does is these tumors tend to form discohesive, single-file patterns and infiltrate into the tumor stroma, as opposed to ductal cancers, which generally form more cohesive masses. As we generally explain to patients, ductal cancers tend to form lumps, while lobular cancers often are not palpable because they infiltrate into the stroma. This creates several challenges, particularly when it comes to imaging. In the diagnostic setting, we know that mammograms and ultrasounds have less sensitivity to detect lobular versus ductal breast cancer. When it comes to the metastatic setting, conventional imaging techniques like CT scans have less sensitivity to detect lobular lesions often. One other unique characteristic of ILC is that these tumors tend to have lower proliferation rates. Because our glucose-based PET scans depend on glucose uptake of proliferating cells, often these tumors also are not avid on conventional FDG-PET scans. It is a challenge for us to monitor these patients as they go through treatment. If you think about the metastatic setting, we start a new treatment, we image people every three to four cycles, about every three months, and we combine the imaging results with clinical assessment and tumor markers to decide if the treatment is working. But if your imaging is not reliable, sometimes even at diagnosis, to really detect these tumors, then really, how are we following these patients? This is really the unique challenge in the metastatic setting in patients with lobular breast cancer: we cannot rely on the imaging to tell if patients are responding to treatment. This is where liquid biopsies are really, really important, and as the field is growing up and we have better and better technologies, lobular breast cancer is going to be a field where they are going to play an important role. Dr. Rafeh Naqash: Thank you for that easy-to-understand background. The second aspect that I would like to have some context on, to help the audience understand why you did what you did, is ctDNA, tumor informed and non-informed. Could you tell us what these subtypes of liquid biopsies are and why you chose a tumor informed assay for your study? Dr. Julia Foldi: Yes, it is really important to understand these differences. As you mentioned, there are two main platforms for liquid biopsy assays, circulating tumor DNA assays. I think what is more commonly used in the metastatic setting are non-tumor informed assays, or agnostic assays. These are generally next-generation sequencing-based assays that a lot of companies offer, like Guardant, Tempus, Caris, and FoundationOne. These do not require tumor tissue; they just require a blood sample, a plasma sample, essentially. The next-generation sequencing is done on cell-free DNA that is extracted from the plasma, and it is looking for any cell-free DNA and essentially, figuring out what part of the cell-free DNA comes from the tumor is done through a bioinformatics approach. Most of these assays are panel tests for cancer-associated mutations that we know either have therapeutic significance or biologic significance. So, the results we receive from these tests generally read out specific mutations in oncogenic genes, or sometimes things like fusions where we have specific targeted drugs. Some of the newer assays can also read out tumor fraction; for example, the newest generation Guardant assay that is methylation-based, they can also quantify tumor fraction. But the disadvantage of the tumor agnostic approach is that it is a little bit less sensitive. Opposed to that, we have our tumor informed tests, and these require tumor tissue. Essentially, the tumor is sequenced; this can either be whole exome or whole genome sequencing. The newer generation assays are now using whole genome sequencing of the tumor tissue, and a personalized, patient-specific panel of alterations is essentially barcoded on that tumor tissue. This can be either structural variants or it can be mutations, but generally, these are not driver mutations, but sort of things that are present in the tumor tissue that tend to stay unchanged over time. For each particular patient, a personalized assay, if you want to call it a fingerprint or barcode, is created, and then that is what then is used to test the plasma sample. Essentially, you are looking for that specific cancer in the blood, that barcode or fingerprint in the blood. Because of this, this is a much more sensitive way of looking for ctDNA, and obviously, this detects only that particular tumor that was sequenced originally. So, it is much more sensitive and specific to that tumor that was sequenced. You can argue for both approaches in different settings. We use them in different settings because they give us different information. The tumor agnostic approach gives us mutations, which can be used to determine what the next best therapy to use is, while the tumor informed assay is more sensitive, but it is not going to give us information on therapeutic targets. However, it is quantified, and we can follow it over time to see how it changes. We think that it is going to tell us how patients respond to treatment because we see our circulating tumor DNA levels rise and fall as the cancer burden increases or decreases. We decided to use the tumor informed approach in this particular study because we were really interested in how to determine if patients are having response to treatment versus if they are going to progress on their treatment, more so than looking for specific mutations. Dr. Rafeh Naqash: When you think about these tumor informed assays and you think about barcoding the mutations on the original tumor that you try to track or follow in subsequent blood samples, plasma samples, in your experience, if you have done it in non-lobular cancers, do you think shedding from the tumor has something to do with what you capture or how much you capture? Dr. Julia Foldi: Absolutely. I think there are multiple factors that go into whether someone has detectable ctDNA or not, and that has to do with the type of cancer, the location, right, where is the metastatic site? This is something that we do not fully understand yet: what are tumors that shed more versus not? There is also clearance of ctDNA, and so how fast that clearance occurs is also something that will affect what you can detect in the blood. ctDNA is very short-lived, only has a half-life of hours, and so you can imagine that if there is little shedding and a lot of excretion, then you are not going to be detecting a lot of it. In general, in the metastatic setting, we see that we can detect ctDNA in a lot of cases, especially when patients are progressing on treatment, because we imagine their tumor burden is higher at that point. Even with the non-tumor informed assays, we detect a lot of ctDNA. Part of this study was to actually assess: what is the proportion of patients where we can have this information? Because if we are only going to be able to detect ctDNA in less than 50 percent of patients, then it is not going to be a useful method to follow them with. Because this field is new and we have not been using a lot of tumor informed assays in the metastatic setting, we did not really know what to expect when we set out to look at this. We did not know what was going to be the baseline detection rate in this patient population, so that was one of the first things that we wanted to answer. Dr. Rafeh Naqash: Excellent. Now going to this manuscript in particular, what was the research question, what was the patient population, and what was the strategy that you used to investigate some of these questions? Dr. Julia Foldi: So, we partnered with Natera, and the reason was that their Signatera tumor-informed assay was the first personalized, tumor-informed, really an MRD assay, minimal residual disease detection assay. It has been around the longest and has been pretty widely used commercially already, even though some of our data is still lacking. but we know that people are using this in the real world. We wanted to gather some real-world data specifically in lobular patients. So, we asked Natera to look at their database of commercial Signatera testing and look for patients with stage 4 lobular breast cancer. The information all comes from the submitting physicians sending in pathologic reports and clinical notes, and so they have that information from the requisitions essentially that are sent in by the ordering physician. We found 66 patients who were on first-line or close to first-line endocrine-based therapies for their metastatic lobular breast cancer and had serial collections of Signatera tests. The way we defined baseline was that the first Signatera had to be sent within three months of starting treatment. So, it is not truly baseline, but again, this is a limitation of looking at real-world data is that you are not always going to get the best time point that you need. We had over 350 samples from those 66 patients, again longitudinal ctDNA samples, and our first question was what is the baseline detection rate using this tumor informed assay? Then, most importantly, what is the concordance between changes in ctDNA and clinical response to treatment? That is defined by essentially radiologic response to treatment. Dr. Rafeh Naqash: Interesting. So, what were some of your observations in terms of ctDNA dynamics, whether baseline levels made a difference, whether subsequent levels at different time points made a difference, or subsequent levels at, let us say, cycle three made a difference? Were there any specific trends that you saw? Dr. Julia Foldi: So, first, at baseline, 95 percent of patients had detectable ctDNA, which is, I think, a really important data point because it tells us that this can be a really useful test. If we can detect it in almost all patients before they start treatment, we are going to be able to follow this longitudinally. And again, these were not true baseline samples. So, I think if we look really at baseline before starting treatment, almost all patients will have detectable ctDNA in the metastatic setting. The second important thing we saw was that disease progression correlated very well with increase in ctDNA. So, in most patients who had disease progression by imaging, we saw increase in ctDNA. Conversely, in most patients who had clinical benefit from their treatment, so they had a response or stable disease, we saw decrease in ctDNA levels. It seems that what we call molecular response based on ctDNA is tracking very nicely along with the radiographic response. So, those were really the two main observations. Again, this is a small cohort, limited by its real-world nature and the time points that ctDNA assay was sent was obviously not mandated. This is a real-world data set, and so we could not really look at specific time points like you asked about, let us say, cycle three of therapy, right? We did not have all of the right time points for all of the patients. But what we were able to do was to graph out some specific patient scenarios to illustrate how changes in ctDNA correlate with imaging response. I can talk a little bit about that. Dr. Rafeh Naqash: That was going to be my question. Did you see patients who had serial monitoring using the tumor informed ctDNA assay where the assay became positive a few months before the imaging? Did you have any of those kinds of observations? Dr. Julia Foldi: Yes, so I think this is where the field is going: are we able to use this technology to maybe detect progression before it becomes clinically apparent? Of course, there are lots of questions about: does that really matter? But it seems like, based on some of the patient scenarios that we present in the paper, that this testing can do that. So, we had a specific scenario, and this is illustrated in a figure in the paper, really showing the treatment as well as the changes in ctDNA, tumor markers, and also radiographic response. So, this particular patient was on first-line endocrine therapy and CDK4/6 inhibitor with palbociclib. Initially, she had a low-level detectable ctDNA. It became undetectable during treatment, and the patient had a couple of serial ctDNA assays that were negative, so undetectable. And then we started, after about seven months on this combination therapy, the ctDNA levels started rising. She actually had three serial ctDNA assays with increasing level of ctDNA before she even had any imaging tests. And then around the time that the ctDNA peaked, this patient had radiographic evidence of progression. There was also an NGS-based assay sent to look for specific mutations at that point. The patient was found to have an ESR1 mutation, which is very common in this patient population. She was switched to a novel oral SERD, elacestrant, and the ctDNA fell again to undetectable within the first couple months of being on elacestrant. And then a very similar thing happened: while she was on this second-line therapy, she had three serial negative ctDNA assays, and then the fourth one was positive. This was two months before the patient had a scan that showed progression again. Dr. Rafeh Naqash: And Julia, like you mentioned, this is a small sample size, limited number of patients, in this case, one patient case scenario, but provides insights into other important aspects around escalation or de-escalation of therapy where perhaps ctDNA could be used as an integral biomarker rather than an exploratory biomarker. What are some of your thoughts around that and how is the breast cancer space? I know like in GI and bladder cancer, there has been a significant uptrend in MRD assessments for therapeutic decision making. What is happening in the breast cancer space? Dr. Julia Foldi: So, super interesting. I think this is where a lot of our different fields are going. In the breast cancer space, so far, I have seen a lot of escalation attempts. It is not even necessarily in this particular setting where we are looking at dynamics of ctDNA, but in the breast cancer world, of course, we have a lot of data on resistance mutations. I mentioned ESR1 mutation in a particular patient in our study. ESR1 mutations are very common in patients with ER-positive breast cancer who are on long-term endocrine therapy, and ESR1 mutations confer resistance to aromatase inhibitors. So, that is an area that there has been a lot of interest in trying to detect ESR1 mutations earlier and switching therapy early. So, this was the basis of the SERENA-6 trial, which was presented last year at ASCO and created a lot of excitement. This was a trial where patients had non-tumor-informed NGS-based Guardant assay sent every three to six months while they were on first-line endocrine therapy with a CDK4/6 inhibitor. If they had an ESR1 mutation detected, they were randomized to either continue the same endocrine therapy or switch to an oral SERD. The trial showed that the population of patients who switched to the oral SERD did better in terms of progression-free survival than those who stayed on their original endocrine therapy. There are a lot of questions about how to use this in routine practice. Of course, it is not trivial to be sending a ctDNA assay every three to six months. The rate of detection of these mutations was relatively low in that study; again, the incidence increases in later lines of therapy. So, there are a lot of questions about whether we should be doing this in all of our first-line patients. The other question is, even the patients who stayed on their original endocrine therapy were able to stay on that for another nine months. So, there is this question of: are we switching patients too early to a new line of therapy by having this escalation approach? So, there are a lot of questions about this. As far as I know, at least in our practice, we are not using this approach just yet to escalate therapy. Time will tell how this all pans out. But I think what is even more interesting is the de-escalation question, and I think that is where tumor informed assays like Signatera and the data that our study generated can be applied. Actually, our plan is to generate some prospective data in the lobular breast cancer population, and I have an ongoing study to do that, to really be able to tease out the early ctDNA dynamics as patients first start on endocrine therapy. So, this is patients who are newly diagnosed, they are just starting on their first-line endocrine therapy, and measure, with sensitive assays, measure ctDNA dynamics in the first few months of therapy. In those patients who have a really robust response, that is where I think we can really think about de-escalation. In the patients whose ctDNA goes to undetectable after just a few weeks of therapy with just an endocrine agent, they might not even need a CDK4/6 inhibitor in their first-line treatment. So, that is an area where we are very interested in our group, and I know that other groups are looking at this too, to try to de-escalate therapy in patients who clear their ctDNA early on. Dr. Rafeh Naqash: Thank you so much. Well, lots of questions, but at the same time, progress comes through questions asked, and your project is one of those which is asking an interesting question in a rarer cancer and perhaps will lead to subsequent improvement in how we monitor these individuals and how we escalate or de-escalate therapy. Hopefully, we will get to see more of what you are working on in subsequent submissions to JCO Precision Oncology and perhaps talk more about it in a couple of years and see how the space and field is moving. Thanks again for sharing your insights. I do want to take one to two quick minutes talking about you as an investigator, Julia. If you could speak to your career pathway, your journey, the pathway to mentorship, the pathway to being a mentor, and how things have shaped for you in your personal professional growth. Dr. Julia Foldi: Sure, yeah, that is great. Thank you. So, I had a little bit of an unconventional path to clinical medicine. I actually thought I was going to be a basic scientist when I first started out. I got a PhD in Immunology right out of college and was studying not even anything cancer-related. I was studying macrophage signaling in inflammatory diseases, but I was in New York City. This was right around the time that the first checkpoint inhibitors were approved. Actually, some of my friends from my PhD program worked in Jim Allison's lab, who was the basic scientist responsible for ipilimumab. So, I got to kind of first-hand experience the excitement around bringing something from the lab into the clinic that actually changed really the course of oncology. And so, I got very excited about oncology and clinical medicine. So, I decided to kind of switch gears from there and I went back to medical school after finishing my PhD and got my MD at NYU. I knew I wanted to do oncology, so I did a research track residency and fellowship combined at Yale. I started working early on with the breast cancer team there. At the time, Lajos Pusztai was the head of translational research there at Yale, and I started working with him early in my residency and then through my fellowship. I worked on several trials with him, including a neoadjuvant checkpoint inhibitor trial in triple-negative breast cancer patients. During my last year in fellowship, I received a Conquer Cancer Young Investigator Award to study estrogen receptor heterogeneity using spatial transcriptomics in this subset of breast cancers that have intermediate estrogen receptor expression. From there, I joined the faculty at the University of Pittsburgh in 2022. So, I have been there about almost four years at this point. My interests really shifted slowly from triple-negative breast cancers towards ER-positive breast cancers. When I arrived in Pittsburgh, I started working very closely with some basic and translational researchers here who are very interested in estrogen signaling and mechanisms of resistance to endocrine therapy, and there is a large group here interested in lobular breast cancers. During my training, I was not super aware even that lobular breast cancer was a unique subtype of breast cancers, and that is, I think, changing a little bit. There is a lot more awareness in the breast cancer clinical and research community about ILC being a unique subtype, but it is not even really part of our training in fellowship, which we are trying to change. But I have become a lot more aware of this because of the research team here and through that, I have become really interested also on the clinical side. And so, we do have a Lobular Breast Cancer Research Center of Excellence here at the University of Pittsburgh and UPMC, and I am the leader on the clinical side. We have a really great team of basic and translational researchers looking at different aspects of lobular breast cancers, and some of the work that I am doing is related to this particular manuscript we discussed and the next steps, as I mentioned, a prospective study of early ctDNA dynamics in lobular patients. I also did some more clinical research work in collaboration with the NSABP looking at long-term outcomes of patients with lobular versus ductal breast cancers in some of their older trials. And so, that is, in a nutshell, a little bit about how I got here and how I became interested in ILC. Dr. Rafeh Naqash: Well, thank you for sharing those personal insights and personal journey. I am sure it will inspire other trainees, fellows, and perhaps junior faculty in trying to find their niche. The path, as you mentioned, is not always straight; it often tends to be convoluted. And then finding an area that you are interested in, taking things forward, and being persistent is often what matters. Dr. Julia Foldi: Thank you so much for having me. It was great. Dr. Rafeh Naqash: It was great chatting with you. And thank you for listening to JCO Precision Oncology Conversations. Don't forget to give us a rating or review, and be sure to subscribe so you never miss an episode. You can find all ASCO shows at asco.org/podcasts. The purpose of this podcast is to educate and to inform. This is not a substitute for professional medical care and is not intended for use in the diagnosis or treatment of individual conditions. Guests on this podcast express their own opinions, experience, and conclusions. Guest statements on the podcast do not express the opinions of ASCO. The mention of any product, service, organization, activity, or therapy should not be construed as an ASCO endorsement.
Metastatic Bladder Cancer — Rapid Case Review Issue 2
Featuring patient case presentations by Dr Fern Anari and Dr Catherine Fahey, with commentary from Dr Matthew D Galsky, including the following topics: Case: A man in his early 60s with urothelial bladder cancer (UBC) is found to have metastatic disease shortly after surgery (0:00) Case: A man in his late 70s experiences disease progression after first- and second-line treatment for metastatic disease (7:39) Case: A fit man in his early 70s presents with metastatic disease (15:22) CME information and select publications
Metastatic Bladder Cancer — Rapid Case Review Issue 2
Dr Fern Anari from the Fox Chase Cancer Center in Philadelphia, Pennsylvania, and Dr Catherine Fahey from the Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina, present real patient cases on metastatic bladder cancer, with additional commentary from Dr Matthew Galsky from The Tisch Cancer Institute in New York, New York.CME information and select publications here.
Today's conversation is a deeply personal look at what it means to be diagnosed with breast cancer at just 30 years old. We often hear the statistics that more young women are being diagnosed, but numbers can't capture the shock of finding a lump before you think you're even old enough to worry… or the life-altering shift that happens when you are put into medically induced menopause. Caroline McNally knows the struggles of being in the thick of treatment and the isolation of being diagnosed younger than most. But she also knows about strength, hope and learning how to advocate for herself and others.
I Was Diagnosed With Stage 4 Breast Cancer at 26 — What 27 Years With Metastatic Disease Taught Me (Part 2)
I'm Still Here: Lessons from Life with Metastatic Breast Cancer with Heather Jose
Last week in Part 1, I shared the story of being diagnosed with metastatic (stage 4) breast cancer at just 26 years old — the shock, fear, and life-altering moment that changed everything.In Part 2, I talk about what came next.After living with metastatic disease for 27 years, my perspective on life, time, fear, and what truly matters has shifted in ways I never expected.This episode is about:• learning to live fully inside uncertainty• letting go of waiting for life to feel safe• naming the hard stuff without being consumed by it• and discovering meaning alongside ongoing treatmentIt's not about staying positive.It's about staying present.If you're living with cancer, loving someone who is, or navigating a season of life that feels uncertain or heavy, I hope this conversation reminds you that life can still be meaningful — even here.Available Now!
Welcome to Season 2 of the Orthobullets Podcast.In this episode, we review the high-yield topic of Metastatic Disease of Extremity from the Pathology section.Follow Orthobullets on Social Media:FacebookInstagramTwitterLinkedInYouTube
Treatment is a significant part of overcoming breast cancer, but what about the mental, physical and emotional challenges this disease presents? Sarah Cipolla and Tawana Davis both relied on their faith to get through breast cancer. Through it all – the ups and downs and good times and setbacks – they had hope for better days and trusted in their faith. Hope and faith are powerful forces during challenging times. Susan G. Komen leads Worship in Pink, a nationwide program that brings breast health education to faith communities. Through this effort, Komen can reach people who don't participate in breast health care and people who rely on their faith to overcome life's challenges. Thanks to Merck and Novartis for supporting the Worship in Pink Program
Episode 88: In the clinic - Metastatic Renal Cancer with Professor Ricky Frazer (part 1/2)
Send us a textJoin us is as we celebrate Kidney Cancer week with a Masterclass walk through metastatic Renal Cancer with Professor Ricky Frazer from Velindre Cancer Centre.Ricky is a co-host of the hugely successful Immunobuddies podcast and has a vast experience in immunotherapy management.We look at the indications for immunotherapy versus anti-VEGF TKI therapy.Should we just accept anti-VEGF TKI monotherapy in Favourable Risk patients?When should we try IO/IO combination versus IO/TKI combinations in the first line setting?All this whilst Ricky looks to put John in his place!!Enjoy
I Was Diagnosed With Stage 4 Breast Cancer at 26 — Living With Metastatic Disease for 27 Years (Part 1)
I'm Still Here: Lessons from Life with Metastatic Breast Cancer with Heather Jose
At 26 years old, I was diagnosed with metastatic (stage 4) breast cancer — a moment that changed everything in an instant.In Part 1 of my story, I share what led up to my diagnosis, the shock of hearing the words “stage four,” and what those early days of fear, uncertainty, and life-altering decisions were really like.This isn't a clinical cancer story.It's the human side — the emotions, the questions, the grief, and the beginning of learning how to live inside a life I never planned for.If you're newly diagnosed, supporting someone you love, or walking through something that feels overwhelming, this episode is for you.Part 2 will dive into how those early experiences shaped the way I live fully with metastatic disease today.Available Now!
Three years after finishing treatment for stage 1 breast cancer, Lea learned she had metastatic breast cancer, for which there is no cure today. Even after having to fight for an initial screening, not receiving a recommendation to start tamoxifen and not experiencing transparency from her doctor, Lea Leach kept advocating for herself and making changes be treated as a whole person. Today, she is living her life with purpose and is passionate about advocating for breast cancer awareness, particularly for women of color.
How the First Metastatic Site Shapes Survival in Breast Cancer Relapse
Presenter: Ryan Quigley Not all metastatic breast cancer is created equal. This AudioAbstract spotlights new data from a multicenter study in Japan that highlights how the first site of distant recurrence can significantly shape a patient's prognosis. By isolating cases with single-organ metastasis, the study draws sharp contrasts in survival based on metastatic location, revealing that patients with brain or liver involvement fare far worse than those with bone or lung metastases. Tune in to better understand how site and even biology and presentation can guide care for patients with metastatic breast cancer.
Episode 87: The Landscape for Metastatic Endometrial Cancer with Dr Gemma Eminowicz (Part 2/2)
Send us a textJoin us for Part 2 of our Metastatic Endometrial Cancer special with the amazing Dr Gemma Eminowicz from University College London Hospital. In episode 1 we looked at molecular profiling and immunotherapy.In this episode we explore the role of;- hormone therapy- Antibody drug conjugates- PARP inhibitorsEndometrial cancer is taking off in terms of new and exciting treatment options.Gemma does an amazing job talking us through them.Enjoy.
Welcome to the Komen Health Equity Revolution podcast series on Real Pink. Each month in this series, we bring together patients, community partners, health care providers, researchers and advocates to talk about real challenges and real solutions driving the health equity revolution. Today, we're exploring what happens when survival requires more than strength — it requires grace. Our guest, breast cancer survivor and advocate Joi White, discovered that letting go, softening and advocating for herself became the real pathway to healing. Her story is courageous, culturally resonant and deeply honest.
The present and future directions of metastatic prostate cancer treatment
In this episode, UROONCO PCa Associate Editor Assoc. Prof. Pawel Rajwa (PL) interviews medical oncologist Prof. Silke Gillessen Sommer (CH) about the present and future directions of metastatic prostate cancer treatment.They discuss the greatest survival gains in metastatic prostate cancer over the past decade, triplet therapy in mHSPC and patient selection, the role of PSMA-PET imaging and sequencing of systemic therapies in metastatic prostate cancer, biomarker-driven treatment selection, and finally where the future of metastatic prostate cancer treatment is heading.Here are the links to the articles and event which were mentioned in this podcast: EORTC GUCG 2238 De-escalate trialCAPItello-281 phase III studyAPCCC (Advanced Prostate Cancer Consensus Conference)For more updates on prostate cancer, please visit our educational platform UROONCO PCa.For more EAU podcasts, please go to your favourite podcast app and subscribe to our podcast channel for regular updates: Apple Podcasts, Spotify, EAU YouTube channel.
Metastatic Bladder Cancer — Rapid Case Review Issue 1
Featuring patient case presentations by Dr Fern Anari and Dr Catherine Fahey, with commentary from Dr Matthew D Galsky, including the following topics: Case: A man in his early 60s with metastatic urothelial bladder cancer (mUBC) and medical history of tobacco use receives first-line enfortumab vedotin (EV) and pembrolizumab with excellent response after 3 cycles — Dr Fahey (0:00) Case: A woman in her early 80s with tumor mutational burden-high mUBC receives pembrolizumab with complete response and later discontinues after developing Grade 1 pneumonitis has no further evidence of disease — Dr Anari (9:19) Case: A man in his early 70s with mUBC who received single-agent EV develops neuropathy and hyperglycemia — Dr Anari (19:10) CME information and select publications
Metastatic Bladder Cancer — Rapid Case Review Issue 1
Dr Catherine Fahey from the Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina, and Dr Fern Anari from the Fox Chase Cancer Center in Philadelphia, Pennsylvania, present real patient cases on metastatic bladder cancer, with additional commentary from Dr Matthew Galsky from The Tisch Cancer Institute in New York, New York.CME information and select publications here.
In this episode, we review the high-yield topic of Metastatic Brain Cancer from the Oncology section at Medbullets.comFollow Medbullets on social media:Facebook: www.facebook.com/medbulletsInstagram: www.instagram.com/medbulletsofficialTwitter: www.twitter.com/medbulletsLinkedin: https://www.linkedin.com/company/medbullets
Metastatic Prostate Cancer: What Actually Matters After the Cancer Has Spread
Even after a serious diagnosis, men can still pursue decisions that protect the life they want to live. In this episode, Dr. Stephen Petteruti addresses metastatic prostate cancer with a focus on what truly shapes outcomes after the disease has spread. He explains why castration resistance often determines prognosis, how conventional pathways can accelerate decline, and why alternative strategies like bipolar testosterone therapy aim to disrupt cancer biology while supporting vitality.Survival benefit must be weighed against real-world cost. Dr. Stephen walks through chemotherapy, advanced hormone blockade, radioactive therapies, and genetic-targeted drugs, translating statistics into months lived and quality preserved. The emphasis stays on informed choice and realistic expectations.Value clarity over coercion and vitality over hollow promises. Tune in to the episode of Metastatic Prostate Cancer: What Actually Matters After the Cancer Has Spread.Enjoy the podcast? Subscribe and leave a 5-star review on your favorite platforms.Dr. Stephen Petteruti is a leading Functional Medicine Physician dedicated to enhancing vitality by addressing health at a cellular level. Combining the best of conventional medicine with advancements in cellular biology, he offers a patient-centered approach through his practice, Intellectual Medicine 120. A seasoned speaker and educator, he has lectured at prestigious conferences like A4M and ACAM, sharing his expertise on anti-aging. His innovative methods include concierge medicine and non-invasive anti-aging treatments, empowering patients to live longer, healthier lives.Website: https://www.drstephenpetteruti.com/Practice: www.intellectualmedicine.comYouTube: https://www.youtube.com/@intellectualmedicineLinkedIn: https://www.linkedin.com/in/drstephenpetteruti/Instagram: https://www.instagram.com/dr.stephenpetteruti/Facebook: https://www.facebook.com/dr.stephenpetterutiMen's Vitality Community: https://www.intellectualmedicine.com/membership Consult with Dr. Petteruti: https://www.intellectualmedicine.com/consultation Provider training: https://www.imeduniversity.com/provider-growth-experienceYouTube: https://www.youtube.com/@intellectualmedicine Instagram: instagram.com/intellectualmedine Disclaimer: The content presented in this video reflects the opinions and clinical experience of Dr. Stephen Petteruti and is intended for informational and educational purposes only. It is not medical advice and should not be used as a substitute for professional diagnosis, treatment, or guidance from your personal healthcare provider. Always consult your physician or qualified healthcare professional before making any changes to your health regimen or treatment plan.Produced by https://www.BroadcastYourAuthority.com
No one should face breast cancer alone. Luckily, childhood friends Caryn Siegel Finley and Tammy Leyden didn't have to. The two grew up together on Staten Island and have been best friends since they were 7 years old. When they both were diagnosed with breast cancer in their early 40's, just one year apart, they were able to support each other through the process. Caryn and Tammy are here today to share their stories with us and how they are committed to supporting those affected by breast cancer.
Lakysha was diagnosed with breast cancer in 2018. Her cancer was caught early but test results showed there was a high chance of recurrence. She required surgery, chemotherapy, radiation and a hormone blocker for five years. She also had a hysterectomy to minimize her risk of other cancers. Life is a journey for her, filled with ups and downs, new challenges and triumphs. And Vonya is the friend we all need. She's the friend who helps you reframe your bad days and encourages you to focus on something that brings you joy. She helped Lakysha normalize what she was going through and accept her emotions as they came. She's also the friend who reminds you not to let one bad day spill into the next day.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Ibiayi Dagogo-Jack, MD, FASCO, Van Karlyle Morris, MD - Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/NYM865. CME/MOC/NCPD/CPE/AAPA/IPCE credit will be available until December 10, 2026.Calibrating Clinical Approaches for Metastatic Colorectal and Lung Cancers: Insights on Molecular Testing and BRAF Inhibitors in Community Settings In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported by an educational grant from Pfizer.Disclosure information is available at the beginning of the video presentation.
Redefining Cancer Treatment: Calidi Biotherapeutics' Approach to Enable Systemic Oncolytic Virotherapy for Metastatic Disease
Send us a textIn this episode of WTR Small-Cap Spotlight, host Tim Gerdeman and analyst Robert Sassoon speak with Eric Poma PhD, CEO of Calidi Biotherapeutics Inc (NYSE American: CLDI). The discussion focuses on how Calidi is solving the "delivery problem" in cancer treatment, and specifically how to transport cancer-killing oncolytic viruses systemically through the bloodstream without the body's immune system neutralizing them before they reach the tumor.
S14 Ep74: PRRT With 177Lu-Edotreotide Improves Outcomes vs Everolimus in Metastatic GEP-NETs: With Jonathan R. Strosberg, MD
In today's episode, the discussion features Jonathan R. Strosberg, MD, a professor and leader in the Neuroendocrine Tumor Division and the Department of Gastrointestinal Oncology Research Program at Moffitt Cancer Center in Tampa, Florida, who reviewed the clinical implications of peptide receptor radionuclide therapy (PRRT) with 177Lu-edotreotide (ITM-11) for patients with metastatic gastroenteropancreatic neuroendocrine tumors (GEP-NETs), drawing on efficacy and safety findings from the phase 3 COMPETE trial (NCT03049189).
There is no way around it, breast cancer is hard. But as our guest today will tell you, trying to remain upbeat throughout treatment can have a positive impact on your life. Amy Elizabeth Chalmers Hicks brings a unique perspective. She was adopted so she doesn't know her biological family's health history, leaving her to navigate two cancer diagnoses without the insights many rely on to understand risk. However, despite these unknowns, when she found a lump, she stayed at ease, started treatment right away, surrounded herself with people who were loving and supportive and made a deep commitment to keeping a positive attitude. She is here today to share her inspiring story with us.
Men often don't think of themselves as having breasts. For men, it's their chest or their “pecs.” So it may come as a surprise to learn men are at risk of breast cancer. The fact is men have breast tissue and can get breast cancer. In the U.S., less than 1% of all cases occur in men, but it does happen. Today we are joined by Jake Messier, a man living with metastatic breast cancer, after being misdiagnosed twice and finally learning in August 2024 that it had advanced. Jake openly shares his story across active social media platforms and is dedicated to spreading awareness of male breast cancer, as well as the distinct mental and physical health struggles that go largely unaddressed when a man is navigating what is typically seen as a woman's disease.
Metastatic HR+ Breast Cancer SABCS 2025 Highlights: Dr. Hope Rugo
Welcome to the Oncology Brothers podcast! In this episode, we dived into the key highlights from the SABCS 2025 conference, focusing on metastatic hormone receptor-positive breast cancer. Join us as we discussed: • The role of CDK4-6 inhibitors in frontline therapy, featuring updates from the AMBRE and MONALEESA-3 studies • Insights into second-line treatment options, including the VIKTORIA-1, evERA, EMBER-3, SERENA-6 trials • A critical look at the ASCENT-07 study, exploring the role of antibody-drug conjugates (ADCs) in endocrine-resistant disease We were thrilled to have Dr. Hope Rugo, a world-renowned breast medical oncologist from City of Hope, share her expertise and insights on these pivotal studies. Tune in for an informative discussion that unpacks the latest advancements in treatment options for metastatic hormone receptor-positive breast cancer, and learn how these findings may impact clinical practice. Follow us on social media: • X/Twitter: https://twitter.com/oncbrothers • Instagram: https://www.instagram.com/oncbrothers • Website: https://oncbrothers.com/ Don't forget to like, subscribe, and check out our other episodes for more insights on treatment algorithms, recent approvals, and conference highlights! #SABCS2025 #MBC #HRpositive #CDK46 #ADCs #OncologyBrothers
As we close out the year, we're shining a light on the quiet, powerful work happening every day inside Komen's Patient Care Center. In this special episode, we sit down with two of our remarkable patient navigators — Marcela Orozco and Ladoya Mayfield — to share the biggest impact stories of the year. From helping Spanish-speaking callers break through language barriers to supporting Houston communities facing some of the highest burdens of breast cancer, Marcela and Ladoya bring humanity, hope and heart into the lives of people going through one of their hardest moments.
Advancements and Challenges in Metastatic Colorectal Cancer Treatment
In this episode of the Oncology Brothers podcast, we dived into the latest discussions surrounding metastatic colorectal cancer, focusing on treatment strategies for refractory cases. We recapped our recent discussions with GI experts, including Dr. John Strickler, Dr. Chiara Cremolini, Dr. Namrata Vijayvergia, and Dr. Tiago Biachi. Key topics included: * The importance of next-generation sequencing (NGS) and biomarker testing in treatment planning. * An overview of second-line treatment options such as Tas-102 with Bevacizumab, Regorafenib, and Fruquintinib, along with their respective clinical trial data. * Insights into side effect management and quality of life considerations for patients undergoing palliative treatment. * A discussion on the recent STELLAR-303 study and its implications for immunotherapy in colorectal cancer. Join us as we bridge the gap between academia and community practice, emphasizing the need for improved treatment options and patient care in the realm of refractory colorectal cancer. Follow us on social media: • X/Twitter: https://twitter.com/oncbrothers • Instagram: https://www.instagram.com/oncbrothers • Website: https://oncbrothers.com/ Don't forget to subscribe for more practice-changing updates! #ColorectalCancer #mCRC #TAS102 #Regorafenib #PalliativeCare #OncologyBrothers #GIOcology
We are thrilled to be joined by the co-founder of the Home Edit. She is an Emmy-nominated, NY Times best-selling author, a mom, a wife and a breast cancer survivor - the amazing Clea Shearer. Clea is here to talk about her shocking breast cancer diagnosis at the age of 40, the ongoing reconstruction complications that she has had to endure over the past three years and the unexpected lessons that have come with all of it. Clea's new book is aptly called Cancer is Complicated and she is here to tell us all about how true that statement really is!
Lynsey P. Teulings, APRN - Ahead of the Immunotherapy Curve in Head and Neck Cancer: Preparing for Expanding Immune Options in Locally Advanced and Recurrent/Metastatic Disease
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/RMT865. CME/NCPD/CPE/AAPA/IPCE credit will be available until November 25, 2026.Ahead of the Immunotherapy Curve in Head and Neck Cancer: Preparing for Expanding Immune Options in Locally Advanced and Recurrent/Metastatic Disease In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported through educational grants from Bristol Myers Squibb and Johnson & Johnson.Disclosure information is available at the beginning of the video presentation.
Lynsey P. Teulings, APRN - Ahead of the Immunotherapy Curve in Head and Neck Cancer: Preparing for Expanding Immune Options in Locally Advanced and Recurrent/Metastatic Disease
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/RMT865. CME/NCPD/CPE/AAPA/IPCE credit will be available until November 25, 2026.Ahead of the Immunotherapy Curve in Head and Neck Cancer: Preparing for Expanding Immune Options in Locally Advanced and Recurrent/Metastatic Disease In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported through educational grants from Bristol Myers Squibb and Johnson & Johnson.Disclosure information is available at the beginning of the video presentation.
Lynsey P. Teulings, APRN - Ahead of the Immunotherapy Curve in Head and Neck Cancer: Preparing for Expanding Immune Options in Locally Advanced and Recurrent/Metastatic Disease
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups.For the full presentation, downloadable Practice Aids, slides, and complete CME/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/RMT865. CME/NCPD/CPE/AAPA/IPCE credit will be available until November 25, 2026.Ahead of the Immunotherapy Curve in Head and Neck Cancer: Preparing for Expanding Immune Options in Locally Advanced and Recurrent/Metastatic Disease In support of improving patient care, PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.SupportThis activity is supported through educational grants from Bristol Myers Squibb and Johnson & Johnson.Disclosure information is available at the beginning of the video presentation.
Children can be one of life's greatest blessings. Breast cancer survivors Alex Miles-Stiffler and Sara Galher-Barlow long for larger families but their diagnoses put those dreams farther and farther out of reach. Alex struggled to start a family before her diagnosis. The heart ache she felt after two miscarriages was unbearable at times, and her fertility challenges only grew after breast cancer treatment, but she wasn't giving up on the family she dreamed of having. Sara always knew she wanted several children. She was blessed with a precious daughter prior to being diagnosed, but her cancer was aggressive and treatment couldn't wait. She had to forego egg preservation, and the uncertainty of fertility along with the cost of fertility treatments will make it harder to grow her family.
Knowledge is power, and when it comes to breast cancer, having access to accurate, up-to-date information can make all the difference. That's why Susan G. Komen is committed to providing trusted educational resources that empower patients, caregivers and families to make informed decisions about their care. Today we are joined by Jessica Thompson, who is both a survivor and health communication scientist, to walk us through where the breast cancer community can turn to find comprehensive, unbiased information, what they will find there and the vigorous review process that Komen uses to create its content, starting with their long standing partnership with Dana-Farber/Harvard Cancer Center.
JAMA Oncology : Metastatic Recurrence Among Adolescents and Young Adults With Cancer
Interview with Ann Brunson, MS, and Theresa H. M. Keegan, PhD, MS, authors of Metastatic Recurrence Among Adolescents and Young Adults With Cancer. Hosted by Vivek Subbiah, MD. Related Content: Metastatic Recurrence Among Adolescents and Young Adults With Cancer Metastatic Recurrence in Adolescent and Young Adult Cancer—Key Drivers of Early Mortality
Episode 360: Bridging Tradition and Treatment: Navigation in Native Communities
Patient navigation has become one of the most powerful tools for improving breast cancer outcomes — and in Native American communities, it can be lifesaving. From long travel distances to specialty care, to navigating complex referral systems, to ensuring communication is culturally grounded and respectful, navigation helps Native patients feel supported every step of the way. In celebration of Native American Heritage Month, we're joined by Linda Burhansstipanov, MSPH, DrPH (Cherokee Nation) — founder of the Native American Cancer Research Corp. and a pioneer in developing culturally appropriate patient navigation models for Indigenous American communities. Dr. Burhansstipanov shares insights about how navigation strengthens trust, improves follow-through on screening and treatment, and supports families and entire communities. She also breaks down practical ways health systems and partners like Komen can work together to meet people where they are and help Native patients feel seen, respected and cared for.
Episode 359: How to rebuild energy & vitality after treatment ends
Breast cancer can be one of the toughest experiences anyone can face, but it can also be a transformative journey. While both the physical and emotional challenges are daunting, the path to healing offers a chance to rediscover resilience and joy in unexpected ways. Today, we are excited to welcome Aastha Saggar, a stage 3 breast cancer survivor and the founder of Still Strength Wellness, where she helps survivors, patients and caregivers reclaim peace, strength, and purpose. Aastha believes that rebuilding energy and vitality is not just possible but can be a beautiful new beginning. Get ready to be inspired as she shares her personal story, along with practical strategies that will empower our listeners to not only survive but thrive.
For many Americans, health insurance open enrollment is underway. They're deciding which coverage they need and how they can afford out-of-pocket expenses. They may be learning about high-deductible plans, health savings accounts, flexible spending accounts and so many other options when it comes to health insurance. So how do you know which plan is right for you? Joining me today is Valerie Nelson, manager of federal policy and advocacy at Susan G. Komen, and Mari Montesano, a manager at Komen's Breast Care Helpline, who assists individuals in need of information, support or help navigating their breast health issues.
Today on Real Pink, we are joined by someone w ho knows what it means to care deeply for others and what it feels like when life suddenly requires that same care and compassion be turned inward. She's a devoted mother and caregiver to her son, and when she was diagnosed with breast cancer, she found that she was more mentally prepared to navigate it than expected. Sabrina Thomas is here to tell her story, including how she advocated for herself and learned to accept help from others when she's so used to being the one who gives it. This conversation is a reminder that strength comes in many forms.



































































