Podcasts about Pulmonary fibrosis
- 111PODCASTS
- 302EPISODES
- 23mAVG DURATION
- 1EPISODE EVERY OTHER WEEK
- Feb 19, 2026LATEST
POPULARITY
Best podcasts about Pulmonary fibrosis
Latest news about Pulmonary fibrosis
- RIPK3 Orchestrates Scar‐Associated Macrophage Dysfunction to Drive Pulmonary Fibrosis Wiley: Advanced Science: Table of Contents - Feb 19, 2026
- DEVONIAN REPORTS POSITIVE RESULTS IN PULMONARY FIBROSIS STUDY GuruFocus New Articles - Feb 10, 2026
- FDA Approves Jascayd for Progressive Pulmonary Fibrosis Drugs.com - News for Health Professionals - Dec 30, 2025
- How cells switch from healthy to fibrosis spreaders Futurity - Dec 2, 2025
- Detection of Exosomal MicroRNA with Hybrid Plasmonic Nanoheater‐Driven PCR for Pulmonary Fibrosis Progression Wiley: Small: Table of Contents - Nov 17, 2025
- Innate Immune‐Cloaked Microgel‐Coated Mesenchymal Stromal Cells Reverse Persistent Pulmonary Fibrosis via Reparative Macrophages Wiley: Advanced Materials: Table of Contents - Sep 23, 2025
- POT1 gene mutation linked to pulmonary fibrosis through telomere dysfunction The Medical News - Sep 18, 2025
- Don director Chandra Barot dies at 86 after battling battling pulmonary fibrosis, Farhan Akhtar mourns the loss Bollywood News and Gossip | Bollywood Movie Reviews, Songs and Videos | Bollywood Actress and Actors Updates | Bollywoodlife.com - Jul 20, 2025
- Nerandomilast May Slow Down Progressive Pulmonary Fibrosis Medscape Medical News - Jun 26, 2025
- Inhalable myofibroblast targeting nanoparticles for synergistic treatment of pulmonary fibrosis | Science Advances AAAS: Science Advances: Table of Contents - Apr 30, 2025
Latest podcast episodes about Pulmonary fibrosis
A Quantitative Imaging Measure of Progressive Pulmonary Fibrosis and One-Year Change in Quantitative Computed Tomography Is Associated with Meaningful Outcomes in Fibrotic Lung Disease
Dr. Mohleen Kang chats with Dr. Stephen Humphries, Dr. Matthew Koslow, Dr. Justin Oldham, Dr. Jennifer Wang, Alexander Bankier, and Dr. David Baraghoshi about their articles, "A Quantitative Imaging Measure of Progressive Pulmonary Fibrosis" and "One-Year Change in Quantitative Computed Tomography Is Associated with Meaningful Outcomes in Fibrotic Lung Disease."
Pulmonary Fibrosis - Ep 49 - Introduction to Mindfulness - The Science of Stress
What happens in the body when we experience stress? Why is it especially important to talk about stress and mindfulness in the context of living with Pulmonary Fibrosis? Kim Hopkins, the Executive Director of the Shanthi Project, and Sarah Dennehy - Senior Director of Programs at the Shanthi Project, join the show to discuss the importance of mindfulness! It's the 'Pulmonary Fibrosis' podcast! Brought to you by the Wescoe Foundation for Pulmonary Fibrosis -- get more info at Wescoe.org!See omnystudio.com/listener for privacy information.
Veterans and Interstitial Lung Disease: Providing Specialized Care in Rural and Underserved Areas
Drs. Kaul and Adegunsoye discuss Veterans Affairs' innovative approach to understanding and treating pulmonary fibrosis among veterans by leveraging extensive electronic health records and data repositories. The work focuses on addressing healthcare disparities, exploring risk factors, and developing a hub-and-spoke telehealth model to provide specialized care to veterans in rural and underserved areas.
Pulmonary Fibrosis - Ep 48 - Jen Wescoe Recaps 2025
There was some learning to be done this year, there was some traveling to be done this year -- and there was some celebrating to do this year as well! Jen Wescoe of the Wescoe Foundation for Pulmonary Fibrosis joins Crockett to discuss all the wonderful events of 2025, and some of the exciting and revolutionary things she learned about on the road of battling IPF and ILD! It's the 'Pulmonary Fibrosis' podcast! Brought to you by the Wescoe Foundation for Pulmonary Fibrosis -- visit Wescoe.org for more!See omnystudio.com/listener for privacy information.
Highlights From CHEST 2025: Earlier Detection and Targeted Interventions
CHEST 2025 showcased exciting advances in interstitial lung disease treatment, featuring new anti-fibrotic therapies and more personalized approaches. Drs. Adegunsoye and Kaul discuss emerging strategies for earlier detection and more targeted interventions across different lung disease phenotypes.
EP 110: The Free Resource That's Helping People With Lung Disease Feel Less Alone with Tiffany Quicke
FOR MEDICAL PROFESSIONALS:SIGN UP FOR OUR FREE TRAINING Jan 10th! The Countertransference & Chronic Illness Intensive https://www.thechronicillnesstherapist.com/countertransference-chronic-illness-intensive
Tackling pulmonary fibrosis: Boehringer Ingelheim's new drug + AI approach
In this episode we sit down with Martin Beck, Senior Vice President and Head of the Inflammation Business Unit at Boehringer Ingelheim. Martin grew up just down the road from the company's headquarters in Germany, joined as a scholarship student more than 20 years ago, and never really left – and you'll hear why he still loves it.We spend most of the episode focused on a disease that doesn't get nearly enough attention: idiopathic and progressive pulmonary fibrosis. These are rare, fatal lung-scarring conditions that kill faster than many cancers, yet patients often shrug off the first symptoms as “just aging.” Martin walks us through why half the people on today's treatments stop taking them, how BI just brought the first new medicine in over a decade to the U.S. market, and why an AI tool that spots microscopic changes on lung scans might finally help doctors diagnose and treat these patients' years earlier. 01:24 Meet Martin Beck04:21 About Boehringer Ingelheim07:12 Understanding idiopathic & progressive pulmonary fibrosis10:16 Current treatments & high discontinuation rates12:25 BI's long-term investment in PF16:02 eLung AI tool for earlier diagnosis22:16 A new oral PDE4B inhibitor28:13 Key data highlights from the recent ERS congress30:31 FDA approval & global rollout plansInterested in being a sponsor of an episode of our podcast? Discover how you can get involved here! Stay updated by subscribing to our newsletterTo dive deeper into the topic: Idiopathic pulmonary fibrosis: Refoxy, Boehringer, Insilico, and more on the hunt for curative treatmentsEight respiratory disease companies advancing innovative therapies in 2025BI: Life with pulmonary fibrosis
AMJ Podcast | Episode 3: Shifting the Silence: The Evolving Landscape in Pulmonary Fibrosis
This content was funded by Boehringer Ingelheim, who had no influence or involvement in the development of the content. This material is intended for U.S. healthcare professionals. Pulmonary fibrosis remains one of the most challenging respiratory diseases – often underdiagnosed, undertreated, and misunderstood. In this AMJ podcast, Ayodeji Adegunsoye and Toby Maher share their expert perspectives on how the field is changing, how recent data are shaping clinical decision-making, and why holistic, patient-centered care is critical. Chapters: 03:02 – 15:34 – A Decade Without New Options 15:34 – 27:47 – Understanding the Latest Clinical Trial Data 27:47 – 39:28 – From Hesitancy to Action: Reaching the Community Clinician 39:28 – 54:10 – Psychosocial Support and Patient-Centered Care 54:10 – 01:02:07 – The Role of Primary Care in ILD Diagnosis 01:02:07 – 1:07:48 – Call to Action Speakers: Ayodeji Adegunsoye, MD, PhD – Assistant Professor of Medicine, Biological Sciences Division, University of Chicago, Illinois, USA Toby Maher, MD, PhD – Professor of Clinical Medicine, Keck School of Medicine, University of Southern California, USA
NEJM Interview: Andrew Gabrielson on cuts to the U.S. research agency charged with safeguarding workers' health.
Andrew Gabrielson is a pediatric urology fellow at Lurie Children's Hospital of Chicago. Stephen Morrissey, the interviewer, is the Executive Managing Editor of the Journal. A.T. Gabrielson and C. Corwin. Occupational Health and Safety on the Chopping Block — What's at Stake? N Engl J Med 2025;393:1353-1355.
Pulmonary Fibrosis Podcast - Ep 47 - Help. Hope. Live. With Katherine Lacouture
An organization out there to help meet the changing needs of patients & families?! We are all about that! Katherine Lacouture of Help. Hope. Live. (HelpHopeLive.org) discusses the mission of her team -- medical fundraising for the expenses insurance doesn't cover! We discuss how HHL has a different fundraising model from typical crowdfunding, what community building look like both online & offline -- and how you can get more information for you and your loved ones! It's the 'Pulmonary Fibrosis' podcast! Brought to you by the Wescoe Foundation for Pulmonary Fibrosis -- and the PAIPF Support Network -- visit PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Performance Characteristics for Physiological Measures of Progressive Pulmonary Fibrosis and Progress in Progressive Pulmonary Fibrosis
Dr. Mohleen Kang chats with Dr. Justin Oldham, Dr. Chad Newton and Dr. Jesse Roman about their papers, "Performance Characteristics for Physiological Measures of Progressive Pulmonary Fibrosis" and "Progress in Progressive Pulmonary Fibrosis."
Unpacking Rare Lung Diseases: Interstitial Lung Disease: Treatment Advances & Road Ahead
In this episode, host Saranya Ravindran is joined by Toby Maher to explore the often-overlooked world of interstitial lung diseases. From clarifying common misconceptions to highlighting AI innovations and personalised treatments, the series dives deep into what clinicians need to know about these serious lung conditions. Whether you're new to interstitial lung diseases or experienced in respiratory care, this series offers timely insights and expert takeaways. Timestamps: 00:00: Introduction 00:40: Mainstays of treatment 04:42: Limitations of current antifibrotics 07:50: The future of ILD personalised care 13:40: Are we close to the reversal of fibrosis? 15:52: A message for clinicians
Unpacking Rare Lung Diseases: Interstitial Lung Disease: Detection & Diagnosis
In this episode, host Saranya Ravindran is joined by Toby Maher to explore the often-overlooked world of interstitial lung diseases. From clarifying common misconceptions to highlighting AI innovations and personalised treatments, the series dives deep into what clinicians need to know about these serious lung conditions. Whether you're new to interstitial lung diseases or experienced in respiratory care, this series offers timely insights and expert takeaways. Timestamps: 00:00: Introduction 00:41: Challenges in early diagnosis 03:22: ILD biomarkers 05:49: The overlap with autoimmune diseases 09:16: AI in ILD detection
Pulmonary Fibrosis Podcast - Ep 46 - Community Outreach for Palliative Care in ILD
Why is palliative care so important in ILD, especially in early diagnosis? How would you define palliative care, especially in the context of ILD? Dr. Gillian Love of the Division of Palliative Care with Jefferson Health joins Crockett to discuss these questions and more in the 'Pulmonary Fibrosis' podcast! Brought to you by the Wescoe Foundation for Pulmonary Fibrosis -- and the PAIPF Support Network -- visit PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Unpacking Rare Lung Diseases: Understanding Interstitial Lung Disease
In this episode, host Saranya Ravindran is joined by Toby Maher to explore the often-overlooked world of interstitial lung diseases. From clarifying common misconceptions to highlighting AI innovations and personalised treatments, the series dives deep into what clinicians need to know about these serious lung conditions. Whether you're new to interstitial lung diseases or experienced in respiratory care, this series offers timely insights and expert takeaways. Timestamps: 00:00: Introduction 02:00: ILD landscape: UK versus USA 04:33: What falls under the ILD umbrella? 06:38: Idiopathic pulmonary fibrosis 07:58: Understanding different patient profiles 09:28: Early clinical signs of ILD
Quickfire: Unpacking Rare Lung Diseases: Interstitial Lung Disease
In this episode, host Saranya Ravindran is joined by Toby Maher to explore the often-overlooked world of interstitial lung diseases. From clarifying common misconceptions to highlighting AI innovations and personalised treatments, the series dives deep into what clinicians need to know about these serious lung conditions. Whether you're new to interstitial lung diseases or experienced in respiratory care, this series offers timely insights and expert takeaways.
#106 Confronting Life-Altering Illness & Learning to Live | Meg Lewis
Today I'm joined by Meg Lewis – a passionate advocate and activist in the health space, making a profound impact in respiratory care and palliative health.Meg shares her deeply challenging and complex journey with Hypersensitivity Pneumonitis, a rare form of Pulmonary Fibrosis that can cause irreversible lung damage. The condition is life-altering, with no cure, limited management options, and a severe lack of research, awareness, and available resources. It's a reality that many struggle to even imagine, yet Meg offers an unfiltered, human perspective — shining a light on the physical, emotional, and social challenges that come with living with such an under-recognised illness.She also speaks openly about the ripple effects of her diagnosis, including medically induced disordered eating. From the intense fear of food and choking brought on by her condition, to the emotional toll of weight gain from steroid treatment, Meg vulnerably explores the complex intersection between physical health, body image, and mental well-being.And yet, at the heart of her story is a powerful message about what it means to truly live — even in the face of uncertainty. Meg reminds us of the importance of filling life with the things you love, embracing the “everyday magic” of small joys, and finding moments of laughter and connection despite hardship.https://www.instagram.com/thelungnrestless/https://thelungnrestless.substack.comTikTok: The Lung N Restless
Episode 8: Exploring the Connection Between Pulmonary Fibrosis and Rheumatoid Arthritis
Living with rheumatoid arthritis can pose additional challenges, including interstitial lung disease (ILD), a condition that can significantly impact lung function and quality of life. In this episode of Spotlight on Pulmonary Fibrosis, we welcome Professor Tomcik, a leading rheumatologist from the Institute of Rheumatology in Prague, and Ms Cechova, a patient advocate from the Revma Liga organization. Listen as they discuss key symptoms to look out for, tips to prepare for medical consultations, and the crucial role of support systems in managing this complex condition.
Episode 9: Living with Pulmonary Fibrosis and Rheumatoid Arthritis
Rheumatoid arthritis often brings unexpected complications, including interstitial lung disease (ILD), which can impact both lung function and overall health. In this episode of Spotlight on Pulmonary Fibrosis, Professor Tomcik, a leading rheumatologist from the Institute of Rheumatology in Prague, explores the vital link between rheumatoid arthritis and ILD. He discusses the key symptoms to monitor, risk factors, and what to consider before visiting a doctor. He also covers the screening process for ILD in rheumatoid arthritis and the multidisciplinary approach needed.
Insider Look at Rabacfosadine (Tanovea) from Shelved Human Drug to Dog Lymphoma Treatment | Dr. Doug Thamm #284
Dr. Doug Thamm discusses the development and use of Tanovea, a drug for treating lymphoma in dogs. He explains the drug's origins, initially researched as a human cancer therapeutic in collaboration with Gilead Sciences, and its transition to veterinary use. Dr. Thamm provides insights into Tanovea's application, dosage, and effectiveness compared to the CHOP protocol, as well as its potential side effects and other possible uses in different cancer types like multiple myeloma. The episode also delves into related immunotherapy research and personal reflections from Dr. Thamm, a double cancer survivor, on his career choice in veterinary oncology. Your Voice Matters! If you have a question for our team, or if you want to share your own hopeful dog cancer story, we want to hear from you! Go to https://www.dogcancer.com/ask to submit your question or story, or call our Listener Line at +1 808-868-3200 to leave a question. Related Videos: https://www.youtube.com/watch?v=G0iRyKshzq8 Related Links: Our article on lymphoma: https://www.dogcancer.com/articles/types-of-dog-cancer/lymphoma-in-dogs/ Our article on Tanovea: https://www.dogcancer.com/articles/drugs/tanovea-rabacfosadine-chemotherapy/ Get the facts on dog cancer remission: https://www.dogcancer.com/articles/stats-and-facts/dog-cancer-remission/ Chapters: 00:00 Introduction 00:13 Interview with Dr. Doug Thamm 00:26 The Early Involvement with Tanovea 00:41 Challenges and Discoveries in Drug Development 02:16 Transition from Human to Veterinary Use 02:48 Clinical Trials and Dosage Experiments 06:45 FDA Approval and Practical Use 08:05 Comparing Tanovea and CHOP Protocol 15:23 Exploring Alternative Treatments: Laverdia 18:43 Off-Label Uses and Future Research 23:46 Exploring Tanovea's Effectiveness in Blood Cancers 25:14 Cost Comparison: Tanovea vs. CHOP 26:15 Side Effects of Tanovea 28:47 Pulmonary Fibrosis and Breed-Specific Risks 32:52 Personal Cancer Journeys: Dr. Doug and His Wife 38:23 Debunking Myths About Dog Cancer Treatment 42:24 The Future of Cancer Treatment: Immunotherapy 45:23 Conclusion and Resources Get to know Dr. Doug Thamm: https://www.dogcancer.com/people/doug-Thammm-v-m-d-diplomate-acvim-oncology/ For more details, articles, podcast episodes, and quality education, go to the episode page: https://www.dogcancer.com/podcast/ Learn more about your ad choices. Visit megaphone.fm/adchoices
Navigating Treatment-Resistant Depression, with Ron Jones
Summary: *Ron Jones discusses treatment resistant depression (TRD), which occurs when multiple classes of antidepressant medications fail to provide relief. *TRD is described as a subcategory of major depressive disorder, unrelated to therapy but linked to the ineffectiveness of psychotropic medications. *Ron shares his personal experience with TRD, highlighting the frustration and discouragement of ineffective treatments and the lengthy process of testing medications. *He suggests that emotional and mental needs, when unmet, can lead to chemical imbalances, and treating only the symptoms without addressing underlying issues is insufficient. *Jones emphasizes the importance of understanding one's identity in relation to God, suggesting that misalignment can contribute to mental health issues. *He recounts a pivotal moment in a church service where he felt the Holy Spirit's guidance, leading to a significant change in his depression. *Jones discusses the role of community, vulnerability, and addressing lies or misconceptions about oneself as crucial steps in the healing process. *He advocates for the recognition of negative emotions as truthful indicators and encourages seeking the Holy Spirit's guidance for healing. *Jones stresses the importance of relational accountability and having supportive people in one's life to provide honest feedback. *He concludes by affirming the possibility of finding hope and new life even after experiencing deep depression, through a relationship with Christ and understanding one's true identity. PODCAST INTRO: My guest today, Ron Jones, is a pastoral counselor and mental health advocate and he stopped by to share his first-hand experiences and insights into his victory over treatment-resistant depression (TRD). This discussion touches on the complexities of living with TRD, the challenges of traditional treatment methods, and the importance of having a strong identity in Christ and growing in faith throughout the healing process. What is Treatment-Resistant Depression? Treatment-resistant depression is a severe form of major depressive disorder. Ron explained that clinically, it is defined as depression that does not respond to at least three different classes of antidepressant medications. Ron also shared that this condition is not merely about resistance to therapy but is specifically linked to the ineffectiveness of psychotropic medicines. The Struggle with Traditional Treatments Ron describes the frustration of navigating the medical system, which often prioritizes treating symptoms over addressing root causes. He likens the process to taking aspirin for a headache without investigating the underlying cause. He even pointed out that this approach can be disheartening, especially when medications take weeks to show results, if at all. A Journey of Identity and Faith Throughout his journey, Ron emphasizes the importance of understanding one's true identity. He believes that much of mental illness stems from a misalignment between who we are and who we perceive ourselves to be. For Ron, this journey of self-discovery was deeply intertwined with his faith, which provided a foundation and a source of hope. This foundation withstood 13 years of struggling AND also provided room for growth and intimacy with Christ as he searched how to get out from under his depression. As shared in then opening clip….Ron was desperately clinging to hope God and yet had no hope. Steps Toward Healing Ron offered practical steps for those struggling with depression: Evaluate Your "Have To's": Examine the non-negotiables in your life that might be contributing to your stress and consider whether they are truly necessary. Identify Primary Lies: Reflect on the negative emotions you feel most often and ask the Holy Spirit to reveal the first time you felt this way. Listen for the Holy Spirit: Spend time in silence, asking the Holy Spirit, "What's We most important thing I could hear right now?" and be open to whatever answer comes without editing it. Something I added, only because I have to do this: when I'm seeking God for an answer I have learned that I need to write it down. It is very commen for me to forget the details of what He spoke into my spirit. If you want to add a #4: Write down what you hear the Holy Spirit speak into your spirit and refer to it as often as you need to. Conclusion Ron's story gives us a deeper revelation about Treatment Resistant Depression because it's from his personal experience; his 13 year battle to find relief. His faith, community, and self-reflection was instrumental in overcoming his TRD. While traditional treatments may fall short mainly because they're go to is to fix things with medicine vs looking at a more holistic approach that would include a deep dive into one's identity. So Ron's journey offers hope and encouragement to those facing similar struggles, reminding us that there is always a path to discovering the benefits of knowing the truth and having a stronger identity. Live Loved and Thrive! @alifeofthrive.com Sherrie Pilk With regard to the acronyms you'll hear Ron use, here is what they stand for (this info is more current than the audio intro to this podcast episode): SSRIs - (Selective Serotonin Reuptake Inhibitors) are a class of antidepressants that help treat depression Sozo is a practice/method used by some Christian ministries to describe their approach to inner healing, which focuses on restoring broken relationships with God and healing past trauma (for more info check out sozo.org) SNRIs - Serotonin-Norepinephrine Reuptake Inhibitors PCP - Primary Care Physician BPD - Borderline Personality Disorder Resources along the same topic: Unrelenting Pain Known as The Suicide Disease (CRPS), with Darci Steiner - https://alifeofthrive.com/wp-admin/post.php?post=9563&action=edit Autoimmune Disease, Pulmonary Fibrosis and Faith, with Sara Salazar - https://alifeofthrive.com/2021/09/01/autoimmune-disease/ Hope in the Midst of Chronic Illness, with Sara Willoughby - https://alifeofthrive.com/2025/01/01/hope-in-the-midst-of-chronic-illness-with-sara-willoughby/ Connect with Ron: Ron's podcast w/his friend (Nick): https://podcasts.apple.com/us/podcast/ron-and-nicks-best-friend-podcast/id1599899345 Amazon link to Ron's most recent book - The Little Book of Forgiveness - The Pathway to Freedom: https://www.amazon.com/Little-Book-Forgiveness-pathway-freedom/dp/B0DYNXWKBW/ref=tmm_pap_swatch_0?_encoding=UTF8&dib_tag=se&dib=eyJ2IjoiMSJ9.oljVyfzmkcvd-tRRqhc8qzcDCCeB-vKQpdasKmcPpGyLFkFehAMYradfiTGZARL3MVN6ar_YRewiXpEMrwt-ig.0u01g9j57uS-UD4NfXgrNw4IxQKkAQYxAoW0rJG8AV0&qid=1743803194&sr=8-1 Ron's Bio: R. Kenward Jones is a disruptive teacher, writer, podcaster (who isn't these days?), counselor, husband, father and grandfather. He holds a bachelor's degree in mechanical engineering and master's degrees in biblical studies and counseling. His debut novel, Buried at Sea, was published by Penmore Press in 2022. Daily, he writes proverbs, parables and prayers and shares them on his Facebook page and website to inspire and encourage. R. Kenward Jones is a US Navy veteran and served as both an enlisted man and officer for 12 years before he left the military to become a pastor. After a 13-year long bout with treatment resistant depression he left the ministry to reset his life. He knows the Valley of the Shadow of Death and the power of personal Creativity as the way through it and out of it. Currently he works as a counselor and teaches the 515A “zero excuses” bootcamp at the local YMCA. He and Tina, his high school sweetheart, have been married for 40 years, have two children and one grandchild, and live in Southeastern Virginia although they still consider the Shenandoah Valley to be their “home.” R. Kenward Jones enjoys life and joy tempered by suffering and more than anything wants to help other sufferers experience the same.
Pulmonary Fibrosis Podcast - Ep 45 - Dr. Rachel Kriner Discusses Women and ILD
How does ILD typically present in women vs. men? Any noticeable difference in symptoms? Are there types of ILD that are more common in women than in men? These are the questions we discuss in this episode of the 'Pulmonary Fibrosis' podcast! Jen Wescoe and Dr. Rachel Kriner of Temple Lung Center discuss women and ILD, the mental health of women battling ILD, and great resources you can use to join clinical trials to help beat this disease! The 'Pulmonary Fibrosis' podcast is brought to you by the Wescoe Foundation for Pulmonary Fibrosis -- and the PAIPF Support Network -- visit PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Summary/Outline: *Introduction and Context: The focus is on Denise Clanin's personal experience with the loss of her brother, Garrett, who was diagnosed with a rare disorder called NF2 *Personal Recollections: Denise shares fond memories of her brother, highlighting his love for music and his contagious sense of humor. She also discusses his academic skills and intelligence. *Brother's Diagnosis and Impact: Garrett was diagnosed with NF2 at 11, which led to the loss of certain abilities over time. Denise reflects on how this condition affected her family dynamics and her own feelings of being secondary in focus. *Coping with Challenges: Denise talks about the gradual changes in family dynamics and her personal journey through grief. She discusses the importance of giving oneself grace and the role of faith in navigating these challenges. *Faith and Identity: The conversation touches on the role of faith in dealing with suffering and the challenges of maintaining one's identity amidst family and personal upheaval. Denise emphasizes the importance of keeping one's identity rooted in God. *Writing as a Path to Healing: Denise shares how writing her book, "Among the Stars," helped her process grief and pay homage to her brother. The book serves as a medium to explore themes of hope and personal growth. *Family and Community Support: The importance of community support and family connections is highlighted, especially through shared experiences like charity events. *Future Aspirations: Denise discusses her plans for future writing projects and how she wants to continue exploring themes of identity and personal growth. *Overall Message: The conversation ends with a message of hope. Denise encourages finding hope and blessings even in difficult times and emphasizes the significance of prayer and faith in providing strength and direction. Podcast Intro: My guest is Denise Clanin, a wife, mom and author. She and I connected because of her willingness to share her personal story about losing her brother, Garrett to a rare mutation known as NF2. This disorder caused tumors to grow throughout his body, and that resulted in degrees of loosing his quality of life such as his ability to speak and hear; two of the major ways we communicate! I can't even fathom that slow separation from your loved ones. At the time of the diagnosis Denise was 9 and Garrett 11. At the time of Garrett's passing he was 29. My conversation with Denise weaved together loss, resilience, and faith and the fact that grief can be very transformative in powerful ways. Faith was the cornerstone for Denise as she navigated what it meant to have a sibling who was experiencing a gradual decline in health and in quality of life. We talked about how she felt as her parents naturally gravitated to Garrett's ever increasing dependency. I was curious about that because at 9 years old she's in elementary school, and then through middle and high school and into college; crucial years for a young girl, a young woman. As we talked, I felt I heard in her voice (and the way she shared about this part of the journey) healing and acceptance saturated with grace. With the ever morphing process of the family dynamic we talked about identity and how that is impacted, and how everything about our life is based on identity and so what do we do when things are shifted and we lose titles, responsibilities, relationships? Denise talked about God's ability to use the tragedy of life for transformation in us and how He moves us into a greater purpose using the pain of life. We talked about the book she authored, Among the Stars and how she blended parts of her life to create a family friendly read that has an uplifting message for the heart and the mind. We folded into the conversation, how therapeutic writing/journaling can be in the grief process. And she's started on her next book that will develop one of the characters found in the first book. I love a series where you can engage in more than one book. Listen in and I hope you'll be encouraged by Denise's desire to share her experience into the complexities of grief, the importance of community, and the enduring power of hope, faith, and love. Live Loved and Thrive! @alifeofthrive.com Sherrie Pilk Related topics (podcast and/or blog): Sara Salazar - Autoimmune Disease, Pulmonary Fibrosis and Faith: https://alifeofthrive.com/2021/09/01/autoimmune-disease/ Sherrie Pilkington - Here's How Psalm 23 Showed Me God's Faithfulness: https://alifeofthrive.com/2022/08/17/heres-how-psalm-23-showed-me-gods-faithfulness/ Genetic Testing and Prophylactic Mastectomy, with Erin Simon: https://alifeofthrive.com/2023/02/01/genetic-testing-and-prophylactic-mastectomy-with-erin-simeone/ Connect with Denise: FB: https://www.facebook.com/profile.php?id=100092102171844 Bio: Denise had always dreamed of writing her book. As a child, she loved to write stories with memorable characters and positive themes. She carried this passion for writing into her adolescence and early adulthood, hoping to publish one of her stories someday. However, as with any story plot, there were obstacles to reaching this goal. At Pepperdine University, she began to study accounting, a degree that required intense concentration and countless hours of studying and memorization. In addition, it was around that time when her older brother's chronic medical condition took a turn for the worse – leaving him in almost constant pain and removing his ability to hear, speak, and see well. His parents transitioned into full-time caregivers who sacrificed their time and energy so that their son could live another day. For Denise, this devastating life change meant taking a step back from her hobbies, instead focusing on her family and establishing herself in her career. Sadly, her brother succumbed to the complications of his condition five years after her college graduation. She appreciated the precious time she had with him and the positive impact he left behind. Although she continued her accounting profession after his passing, she knew the corporate world wasn't where she wanted to remain. A few years later, Denise and her husband moved from sunny San Diego to the forested terrain of Post Falls, Idaho, to plant their roots – buying their first home and expanding their family. That was when she finally found the inspiration to pen her first book, “Among the Stars” – originally an idea she wrote for her creative writing class in college. From there, she continued to push forward despite a decade-long writing hiatus and several bouts of writer's block. She is thankful that God has provided her with the words to share with others through her book, touching on the themes of forgiveness, redemption, and hope – while also paying homage to the notable people in her life, including those who have passed. She hopes this tale of first love, friendship, and family connection will bring joy and encouragement to those who need it.
ERJ Podcast March 2025: Generalisability of pharmaceutical randomised controlled trial eligibility criteria for progressive pulmonary fibrosis
As part of the March issue, the European Respiratory Journal presents the latest in its series of podcasts. Deputy Chief Editor Don Sin interviews Associate Editor Yet Khor about the generalisability of pharmaceutical randomised controlled trial eligibility criteria for progressive pulmonary fibrosis.
Pulmpnary Fibrosis Ep 44 - A Lung Transplant Journey
The timeline of diagnosis, to possible transplant recipient -- to post-transplant can feel like a whirlwind for patients and caregivers. Marion Marin, a lung transplant recipient, joins the show to discuss how that process went for her! She discusses advocating for yourself, waiting for 'the call' -- and the importance of the community around you when physically and emotionally dealing with a diagnosis! It's the 'Pulmonary Fibrosis' podcast! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Find this podcast wherever you get your podcasts! Are you interested in helping advance PF research? If so, consider joining a workgroup! Visit wescoe.org or pfpatientengagement.org for more details!See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis. A debilitating disease that restricts a person's lung capacity, controllable with drug therapies, but it's only “cure” is a double lung transplant. Researchers at TGen have released the results of a study that investigated the disease on a cellular level. Using advanced spatial transcriptomics, they identified hidden disease markers in seemingly healthy lung tissue—offering hope for earlier, more personalized treatments. Targeting these early disruptions could improve lung function and outcomes. With current PF treatments only slowing decline, this discovery, published in Nature Genetics, marks a step toward preventing irreversible damage. In this episode of TGen Talks, Nicholas Banovich, Ph.D., discusses the Nature Genetics finding and the new spatial map of gene expression in lung cells. Instead of blending tissue together and analyzing it, scientists can now examine individual cells and pinpoint where molecular changes happen. We'll break down what this means, how it's done, and why it could change the way we study lung disease.
Detection, assessment and management of pulmonary fibrosis
In this Healthed lecture, Associate Professor Nicole Goh outlines the key features of pulmonary fibrosis from presenting and distinguishing signs, testing, and diagnosis to the latest evidence-based treatments. She will also provide an update on the current prognosis and natural history of pulmonary fibrosis as well as the GP's role in managing patients with this not uncommon condition.See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis Ep 43 - Advancing Palliative Care to Better Care for Patients with Serious Illness
What is the difference between Palliative Care & Hospice, and why important to discern the difference?! Dr. Kathleen Lindell of the Medical University of South Carolina joins the show to discuss why Palliative Care can be such an important piece of both the patient and caregivers role in the ILD journey. It's the 'Pulmonary Fibrosis' podcast! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Find this podcast wherever you get your podcasts! Are you interested in helping advance PF research? If so, consider joining a workgroup! Visit wescoe.org or pfpatientengagement.org for more details!See omnystudio.com/listener for privacy information.
Progressive Early Interstitial Lung Abnormalities in Persons At-Risk for Familial Pulmonary Fibrosis: A Prospective Cohort Study and Big Things Have Small Beginnings: Clinical Implications of Early Interstitial Lung Disease
Dr. Mohleen Kang chats with Dr. Margaret Salisbury and Dr. Anna Podolanczuk about their articles, "Progressive Early Interstitial Lung Abnormalities in Persons at Risk for Familial Pulmonary Fibrosis: A Prospective Cohort Study" and "Big Things Have Small Beginnings: Clinical Implications of Early Interstitial Lung Disease."
Let's Talk Death with Susan McCue, LCSW
In this episode, Susan shares her story of dying now that she has entered hospice for comfort care related to a progressive disease with no cure. She hopes to die peacefully at home surrounded by her loved ones while sharing tall tales and laughter.Susan McCue is a licensed clinical social worker who has worked in the field of death, dying, and bereavement since 2005. Her career began first as a hospice social worker, then as a hospice bereavement counselor. After obtaining her LCSW, Susan opened a private therapy practice specializing in grief and loss, mainly focusing on bereavement needs following the immediate death of a loved one.During this time, Susan also provided grief and loss presentations at the community, state, national, and international levels on topics including the difference between the natural process of grief and more complicated grief responses.Susan's personal background includes multiple deaths in her immediate family, which led to Susan's interest and passion for the field of death, dying, and bereavement. She is one of nine children born in an Irish-American family. Her father died at age 64, her mother at age 69, and six of their nine children (Susan's siblings) died in their 50s and 60s.Susan finds her personal and professional life coming full circle now that she has entered hospice for comfort care related to her diagnosis of Pulmonary Fibrosis, a progressive disease with no cure. Susan's brother and sister also died of this disease. Susan volunteers as a Pulmonary Fibrosis Foundation Ambassador to participate in PF research and to share her story with other PF patients, families, and loved ones affected by the disease. She hopes to die peacefully at home surrounded by her loved ones while sharing tall tales and laughter.Support the show
Self-described pulmonary fibrosis warrior and former journalist, Teresa Barnes, joins host and former CNN news anchor Patti Tripathi for the premiere episode of ATS Breathe Easy, the Latest. Ms. Barnes is chief executive of Pulmonary Fibrosis Warriors and former chair of the ATS Public Advisory Roundtable. PAR is comprised of 12-15 executives of respiratory-related patient interest organizations like the Pulmonary Fibrosis Warriors.
Pulmonary Fibrosis Ep 42 - Convene PF and Patient Engaged Research
Everyone can have a role in the Pulmonary Fibrosis community! Whether that's as a patient, a caregiver and beyond -- information is key to helping tackle all things PF. This episode, we're joined by John Marshall and Dr. Ilene Hollin of Temple University Lung Center to discuss the importance of patient engaged research, and how you can be involved in the research as well!! We'll learn more about PCORI and Convene-PF, and how you can participate in the studies! It's the 'Pulmonary Fibrosis' podcast! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Are you interested in helping advance PF research? If so, consider joining a workgroup! Visit wescoe.org or pfpatientengagement.org for more details!See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis Ep 41 - Looking Into the New Year
2024 was an AMAZING year for the 'Pulmonary Fibrosis' podcast! We have been downloaded in 74 countries around the world, and can't wait to continue to explore all avenues that connect the ILD community! Jen Wescoe of the Wescoe Foundation for Pulmonary Fibrosis joins Crockett to discuss some of the tremendous moments of 2024, and what's in store for 2025! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
How is the Veteran community impacted by Interstitial Lung Disease? What are some helpful resources to help Veterans navigate ILD? Dr. Dean (Trey) Kellogg of UT Health San Antonio joins the show to discuss Veterans and ILD! It's the 'Pulmonary Fibrosis' podcast! Hosted by Kevin Crockett. Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis Ep 39 - Role of a Research Coordinator in Clinical Trials
What is the role of a Research Coordinator in clinical trials? Why are clinical trials so important -- especially when discussing Interstitial Lung Disease? Rachel Nwafo of Temple Lung Center tells us about her role, and the path she took to get there! It's the 'Pulmonary Fibrosis' podcast! Hosted by Kevin Crockett. Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis Ep 38 - Spirituality and ILD
How can spirituality, in all denominations and perspectives, be beneficial for one managing Interstitial Lung Disease? How does the family dynamic help in managing this part of one diagnosis? Dr. Patricia Fogelman, and Author/Pastor/Double Lung Transplant recipient Tim Cox join the show to discuss the role spirituality can play when battling disease in the 'Pulmonary Fibrosis' podcast! Hosted by Kevin Crockett. Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis Ep 37 - Pulmonary Rehab With David Junga, RRT, PAS
What is Pulmonary rehab? How has rehab changed thanks to the virtual world? This episode, we're joined by David Junga, RRT, PAS with Pulmonary Rehabilitation Associates, LLC to discuss the great benefits of virtual rehab! It's the 'Pulmonary Fibrosis' podcast! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Pulmonary Fibrosis Ep 36 - Rural Healthcare and ILD
What defines a "rural" area? What step has to been taken to assess rural healthcare & ILD needs? Find out in a new episode of the 'Pulmonary Fibrosis' podcast! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! This episode, we're joined by Dr. Teja Kulkarni of UAB and Dr. Jessica Shore of the Pulmonary Fibrosis Foundation to discuss the impact on patients living in rural areas! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Specialist Spotlight: Racial Disparities in Pulmonary Fibrosis (Part 3)
Drs. Vela and Adegunsoye explore the intersections of patient education, community engagement, and healthcare policies, particularly in addressing the needs of underrepresented racial groups. Monica emphasizes the value of long-term patient-physician relationships in primary care, the necessity of interrupting physician biases, and the importance of systemic changes to facilitate more comprehensive patient interactions. Deji highlights the need for community-based outreach and clinical trial participation to address health disparities, particularly in Black communities. Both underscore the importance of innovative communication strategies to build trust and educate communities about diseases affecting them disproportionately. Their conversation envisions a brighter future with more effective and inclusive healthcare practices.
Specialist Spotlight: Racial Disparities in Pulmonary Fibrosis (Part 2)
Drs. Vela and Adegunsoye delve into the racial disparities in the diagnosis and progression of pulmonary fibrosis, particularly within the black population. They discuss the role of environmental and occupational exposures, and the impact of cultural and autoimmune factors on the disease's prevalence in black communities. Dr. Adegunsoye emphasizes that black individuals are at a higher risk for autoimmune disorders, which can lead to pulmonary fibrosis. Moreover, he highlights the flaws in lung function tests that use race adjustments, often masking the real health conditions in black patients. The discussion also addresses the critical issue of delayed diagnosis, which adversely affects the prognosis of pulmonary fibrosis. Both presenters stress the importance of early screening, equitable access to care, and policy changes to improve outcomes for marginalized populations. They conclude by noting the need for action plans to address these disparities, pointing out that black individuals often get diagnosed and die from pulmonary fibrosis at an earlier age compared to other racial groups.
Specialist Spotlight: Racial Disparities in Pulmonary Fibrosis (Part 2)
Drs. Vela and Adegunsoye delve into the racial disparities in the diagnosis and progression of pulmonary fibrosis, particularly within the black population. They discuss the role of environmental and occupational exposures, and the impact of cultural and autoimmune factors on the disease's prevalence in black communities. Dr. Adegunsoye emphasizes that black individuals are at a higher risk for autoimmune disorders, which can lead to pulmonary fibrosis. Moreover, he highlights the flaws in lung function tests that use race adjustments, often masking the real health conditions in black patients. The discussion also addresses the critical issue of delayed diagnosis, which adversely affects the prognosis of pulmonary fibrosis. Both presenters stress the importance of early screening, equitable access to care, and policy changes to improve outcomes for marginalized populations. They conclude by noting the need for action plans to address these disparities, pointing out that black individuals often get diagnosed and die from pulmonary fibrosis at an earlier age compared to other racial groups.
Specialist Spotlight: Racial Disparities in Pulmonary Fibrosis (Part 1)
Drs. Vela and Adegunsoye share their insights into racial disparities in pulmonary fibrosis, including the impact of characterizing groups based on skin color or race, the concept of cultural humility, and best practices for diagnosing ILD while taking into account these disparities.
Pulmonary Fibrosis Ep 35 - Marie Conley of PARDAC - Pennsylvania Rare Disease Advisory Council
What is the Pennsylvania Rare Disease Advisory Council (PARDAC)? What are some of the important findings in their Patient Needs Assessment Survey? Marie Conley, the Co-chair of PARDAC discusses some of the important and impactful information they've gathered in this episode of the 'Pulmonary Fibrosis' podcast! Brought to you the Wescoe Foundation for Pulmonary Fibrosis and the Pennsylvania IPF Support Network! Learn more at PAIPFsupportnetwork.org!See omnystudio.com/listener for privacy information.
Ep 436 - Pulmonary Fibrosis—An Aberrant Matrix: “I Have a Client Who . . .” Pathology Conversations with Ruth Werner
The ABMP Podcast | Speaking With the Massage & Bodywork Profession
A person with rheumatoid arthritis and lupus develops new back pain in her mid-upper left side. It feels like “it's coming from under my ribs,” she says. First, it's diagnosed as arthritis, but interventions don't seem to make a difference. Finally, a year into this unremitting pain, a rheumatologist asks about her breathing and discovers she has developed a complication called pulmonary thrombosis, probably related to her autoimmune diseases. They start treatment and voilà, her back pain is gone. This is a good example of a case in which massage therapy was definitely NOT the best choice. Resources: Dsouza, K.G. et al. (2023) ‘Management of interstitial lung disease in patients with autoimmune disease-related interstitial lung disease', Multidisciplinary Respiratory Medicine, 18(1), p. 890. Available at: https://doi.org/10.4081/mrm.2023.890. Fibrosis as an autoimmune disease (no date) CPC - M. Available at: https://www.cpc-munich.de/en/research-projects/fibrosis-as-an-autoimmune-disease/index.html, https://www.cpc-munich.de/en/research-projects/fibrosis-as-an-autoimmune-disease/index.html (Accessed: 3 May 2024). 3. Gole, S. and Bankole, A. (2024) ‘Nintedanib', in StatPearls. Treasure Island (FL): StatPearls Publishing. Available at: http://www.ncbi.nlm.nih.gov/books/NBK585049/ (Accessed: 8 May 2024). Interstitial Lung Diseases - What Are Interstitial Lung Diseases? | NHLBI, NIH (2022). Available at: https://www.nhlbi.nih.gov/health/interstitial-lung-diseases (Accessed: 8 May 2024). 5. Kašiković Lečić, S. et al. (2022) ‘Management of musculoskeletal pain in patients with idiopathic pulmonary fibrosis: a review', Upsala Journal of Medical Sciences, 127, p. 10.48101/ujms.v127.8739. Available at: https://doi.org/10.48101/ujms.v127.8739. 6. Massage & Bodywork - MAY | JUNE 2021 (no date). Available at: https://www.massageandbodyworkdigital.com/i/1358392-may-june- Host: Ruth Werner is a former massage therapist, a writer, and an NCBTMB-approved continuing education provider. She wrote A Massage Therapist's Guide to Pathology, now in its seventh edition, which is used in massage schools worldwide. Werner is also a long-time Massage & Bodywork columnist, most notably of the Pathology Perspectives column. Werner is also ABMP's partner on Pocket Pathology, a web-based app and quick reference program that puts key information for nearly 200 common pathologies at your fingertips. Werner's books are available at www.booksofdiscovery.com. And more information about her is available at www.ruthwerner.com. Sponsors: Anatomy Trains: www.anatomytrains.com Elements Massage: www.elementsmassage.com/abmp Earthlite: www.earthlite.com
PREMIERE: Joseph S Joyce - Once Upon An Icelandic Highway [Default Position]
‘'Once upon an Icelandic Highway, my father and I embarked on an unforgettable journey. With a camera securely mounted to our jeep, we ventured out into the vast untouched wilderness to capture Iceland's other-worldly landscapes on film. The rhythmic hum of the tires against the road became our soundtrack as the terrain unfolded. Each twist and turn of the highway revealed breathtaking panoramas - from rugged mountains and cascading waterfalls to frozen glaciers and majestic fjords. On our return, I got to work editing a selection of the best footage. Later, I created a soundtrack that encapsulated the lunar-like surface of this incredible place and the repetitive rhythm of the car cruising along the road. In dedicating this release to my father, I pay homage to a man whose passion for the natural world was unparalleled. In loving memory of Brendan Joyce OBE.'' - Joseph S Joyce All proceeds from this release will be donated to Action for Pulmonary Fibrosis. https://soundcloud.com/josephjoyce https://soundcloud.com/default-position Follow us on social media: https://soundcloud.com/itsdelayed https://linktr.ee/delayed https://www.itsdelayed.com https://www.facebook.com/itsdelayed https://www.instagram.com/_____delayed https://www.youtube.com/@_____delayed
Your health journey is all your own. I'm Annette Leonard of https://www.annetteleonard.com find me on Instagram https://www.instagram.com/theannetteleonard Several things made me think about this topic. I recently was talking about my friend Amy. She died almost exactly a year before I got my diagnosis of Pulmonary Fibrosis. She was waiting for her lung transplant and when she passed she was a frail shadow of herself. Also, my mom died with complications of several of the autoimmune diseases that I have. It's so easy -- especially when we have a difficult or unfamiliar diagnosis, to lean on Dr Google, or other peoples' experiences and let those things coopt our imagination about our illness and I think that can have some disastrous and unintended consequences. The Google will tell you that my life expectancy is 3 - 5 years. Well, here I am 9 years later. While many things COULD have led to my demise -- but tuning that out and walking my own path has been crucial. As a reforming people pleaser, as someone who values information, it's easy to be captivated by the stories people share about anyone they know who may have had something similar to what I have, how that's gone, what's worked, what remedies they've tried. Sometimes, hearing those stories can contribute to the sense that I'm doing it wrong, or add to the sense that "this is going poorly and I've already made the wrong decisions." Having done this for a while and having learned how to BE EMBODIED in this experienced: doing body scans, checking in with my thoughts and feelings, knowing when something's changed. I'm the best person to asses what's going well and when it's time to make a change. No, it isn't fun, it takes a lot of effort to tune in like that, to advocate for myself, to coordinate with my docs and insurance companies, but it's the only way to take control of my health. When I start thinking "well, she said that by this time next year things got really bad..." then I'm initiating a slew of chemicals that will lead to anxiety, fear, pain, or being addicted to my own catastrophes. Perhaps those things will happen, but perhaps they won't. But, the only guarantee is that I've robbed myself of this present moment. The idea of suffering is terrifying. I'm not trying to pretend it isn't. There is fear and anguish. But there are tools. Whether it starts with a contemplative practice, journaling, or noticing what's happening to find a skilled therapist. There are ways to keep my fear of the future from enjoying the present. This journey is YOURS ALONE, from the small to the large. But no amount of today is improved by me fixating on how bad it's going to get. Notice when you get hooked, when you start to borrow trouble. If you don't have tools, skills, or support about making change in that area, it might be time to get some. Let us know how you're making your journey your own. This is the Chronic Wellness Podcast. I'm Annette Leonard, speaker, coach, and sick person who believes that my illnesses do not define me. If health is the absence of disease and wellness is the presence of wholeness, then no matter what your disease status, we can work toward your wellness, your wholeness. Whether or not you are ever "healthy" on paper, you can be well. Join me and others on the path back to wholeness at AnnetteLeonard.com. Whether you are a person experiencing chronic illness or are someone who loves or serves people with chronic illness I have great resources here on this channel or on my website for you.
Best of DvC: ‘Is There Bacon in Heaven' / Pulmonary Fibrosis
For the next few weeks, the guys will be re-airing some of their favourite episodes from our archives. Today on a special episode, we will be hearing a preview of Ali's new book ‘Is There Bacon in Heaven', published by Simon and Shuster, coming out Sept 27. Before Ali gets started Asif discusses summer entertainment he has consumed including ‘Prey', ‘Archer', ‘She-Hulk', ‘Harley Quinn', ‘Rings of Power' and ‘House of the Dragon'. Ali then treats us to a funny and poignant chapter focussing on his father's life and death. During the excerpt, they guys take a brief digression to discuss pulmonary fibrosis, a disease which Ali's father suffered from. Asif talks about what it is, how it is diagnosed and the risk factors for developing it. He then discusses the prognosis and the limited treatments for the condition. The opinions expressed are those of the hosts, and do not reflect those of any other organizations. This podcast and website represents the opinions of the hosts. The content here should not be taken as medical advice. The content here is for entertainment and informational purposes only, and because each person is so unique, please consult your healthcare professional for any medical questions. Music courtesy of Wataboi and 8er41 from Pixabay Contact us at doctorvcomedian@gmail.com Follow us on Social media: Twitter: @doctorvcomedian Instagram: doctorvcomedian Show Notes: Is There Bacon in Heaven: https://www.simonandschuster.ca/books/Is-There-Bacon-in-Heaven/Ali-Hassan/9781982149178 Idiopathic Pulmonary Fibrosis: https://emedicine.medscape.com/article/301226-overview
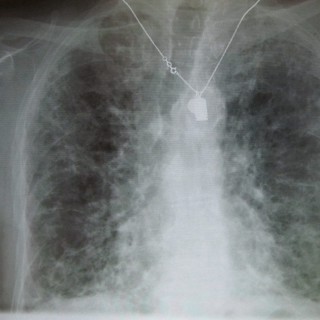
36. Pulmonary fibrosis with Miranda Siemienowicz and Jonathan Chung
Miranda and Jonathan chat chest radiology, mainly focusing on connective tissue disease related interstitial lung disease, but also touching on a whole bunch of other interesting topics. Frank hijacks the intro to chat about our December supporter drive. Find the lectures ► https://radiopaedia.org/courses/chest-lectures Radiopaedia 2024 Virtual Conference ► https://radiopaedia.org/courses/radiopaedia-2024-virtual-conference Become a supporter ► https://radiopaedia.org/supporters Get an All-Access Pass ► https://radiopaedia.org/courses/all-access-course-pass Andrew's Twitter ► https://twitter.com/drandrewdixon Frank's Twitter ► https://twitter.com/frankgaillard Ideas and Feedback ► podcast@radiopaedia.org The Reading Room is a radiology podcast intended primarily for radiologists, radiology registrars and residents.
In our final episode of 2023, the JHLT Digital Media Editors have two manuscripts from the December 2023 issue of The Journal of Heart and Lung Transplantation! Digital Media Editor Erika Lease, MD, transplant pulmonologist at the University of Washington in Seattle, hosts this episode. First, a free-ranging conversation with first author Mark E. Snyder, MD, and senior author John F. McDyer, MD, on their team's study “Impact of age and telomere length on circulating T cells and rejection risk after lung transplantation for idiopathic pulmonary fibrosis.” A subset of patients with idiopathic pulmonary fibrosis (IPF) have a heritable, age-adjusted short telomere length. Mutations in telomere length can manifest as T-cell dysfunction and immunodeficiency. As T-cells are involved in the development of acute cellular rejection (ACR), the authors hypothesized that the combination of age and telomere length would impact the degree of ACR burden in lung transplant recipients—and indeed, the authors found that lung transplant recipients with IPF and short telomere length had premature “aging” of their circulating T-Cells. There was a significant decline in early ACR burden with increasing age, found only in those with short telomere length. How might these findings impact immunosuppression regimens in clinical practice? What follow-up studies to they have planned? In the discussion, Drs. Snyder and McDyer, both of UPMC in Pittsburgh, discuss all these possibilities, as well as the the work of their collaborator, Jonathan K. Alder, PhD, as inspiration for the study. Next, the editors explored “Early optical coherence tomography evaluation of donor-transmitted atherosclerosis and cardiac allograft vasculopathy: insights from a prospective, single-center study,” in a discussion with senior author Snehal R. Patel, MD, of the Montefiore Medical Center in New York. Cardiac allograft vasculopathy (CAV) remains a major cause of death in heart transplant recipients, and donor-transmitted atherosclerosis (defined as a maximal intimal thickness of >/= 0.5mm on baseline intravascular ultrasound (IVUS) early after transplant) is believed to carry a greater risk for the development of CAV. Dr. Patel's team, however, hypothesized that optical coherence tomography (OCT) may have advantages over IVUS as an imaging modality due to its higher resolution. In this prospective, observational study, the authors assessed the prognostic role of OCT, and found that transplant recipients whose OCT imaging showed advanced plaque characteristics had a significantly higher event rate after a mean follow up of 3.3 years. OCT was also an independent predictor of clinic events, while maximal intimal thickness of >/= 0.5mm was not. In the episode, Dr. Patel shares the key features of OCT that may make it of clinical use, the three risk categories developed for the study, and what the follow-ups might be. Follow along at www.jhltonline.org/current, or, if you're an ISHLT member, log in at ishlt.org/journal-of-heart-lung-transplantation. Don't already get the Journal and want to read along? Join the International Society of Heart and Lung Transplantation at www.ishlt.org for a free subscription, or subscribe today at www.jhltonline.org.
EP 297: How To Overcome Anything... A Story Of Life And Breath with Lee Fogel
A retired global technology executive and former Ironman Triathlete at 62 years old, Lee Fogle contracted Covid in The first wave in January 2020. After the resulting two bouts of pneumonia he found himself unable to walk upstairs or do normal activities. He was diagnosed by CTSCAN with end-stage Pulmonary Fibrosis, less than 30% remaining lung function. He was given a life expectancy of 1-3 years unless he could get a lung transplant. As a lifelong biohacker, Lee refused to accept this reduced life expectancy, and although he was unable to walk more than 20 steps without assistance, and required 6 L of supplemental oxygen 24 hours a day he began the process of battling back against the disease. He did exhaustive research and began a gradual, but steadily increasing program of pulmonary rehabilitation and exercise, combined with meditation, nutrition, proper sleep, breath training, and natural supplements. Today he has resumed normal activities of swimming, biking, running, playing pickle, ball and golf, and he's living, a full and active life. He has written a book, A Matter of Life and Breath (available on Amazon) which chronicles, his dramatic health decline and ultimately recovery. He shares the 7 Steps to Recovery in his book. Today he serves as an ambassador to the Pulmonary Fibrosis Foundation, and volunteers his time in hospice and memory care facilities as a Reiki practitioner. Here's where you can contact Lee: Lee.Fogle@injuryclaimsexpress.com http://linkedin.com/in/leefogle https://www.facebook.com/lee.fogle.007?mibextid=LQQJ4d Here's the link to his book: A Matter of Life and Breath: My 7 Step Guide to Overcoming Near Death From Long CoVid and Pulmonary Fibrosis https://a.co/d/2RSUPR8 Exercise effect on pulmonary fibrosis study: https://apm.amegroups.com/article/view/74647/html


































