Podcasts about torsades
Type of abnormal heart rhythm
- 42PODCASTS
- 79EPISODES
- 18mAVG DURATION
- 1MONTHLY NEW EPISODE
- Feb 14, 2026LATEST
POPULARITY
Best podcasts about torsades
Latest news about torsades
- Swishahouse Founder Michael “5000” Watts Dead At 52 Stereogum - Jan 31, 2026
- ECG Pointers: Longer is Always Better… Wait, that’s not right. emDOCs.net – Emergency Medicine Education - Jan 14, 2026
- Detection of Clinically Significant Drug-Drug Interactions in Fatal Torsades de Pointes: Disproportionality Analysis of the Food and Drug Administration Adverse Event Reporting System Journal of Medical Internet Research - Mar 25, 2025
- Torsade in a patient with left bundle branch block: is there a long QT? (And: Left Bundle Pacing). Dr. Smith's ECG Blog - Jan 2, 2025
- REBEL Core Cast 88.0 – Hypocalcemia REBEL EM – Emergency Medicine Blog - Oct 19, 2022
Latest podcast episodes about torsades
In this episode, we review the high-yield topic of Torsades de Pointes from the Cardiovascular section.Follow Medbullets on social media:Facebook: www.facebook.com/medbulletsInstagram: www.instagram.com/medbulletsofficialTwitter: www.twitter.com/medbullets
QT Prolongation and Psychiatric Medication: A Cardiac Safety Update
In this episode, we explore a new study examining whether antidepressants and antipsychotics truly increase the risk of torsades de pointes, a potentially fatal cardiac arrhythmia. What does the evidence say about using multiple psychiatric medications together, and when should we actually be concerned? Faculty: Scott Beach, M.D. Host: Richard Seeber, M.D. Learn more about our membership here Earn 0.75 CMEs: Quick Take Vol. 75 Torsades de Pointes: Impact of Antidepressants and Antipsychotics
Tareq Taylor, Linnea ”köttstjälken” Wikblad och girandole torsades
David VS svenska jaktsamhället, Linnea är killsugen och välrdens ensammaste val Lyssna på alla avsnitt i Sveriges Radio Play. Hela veckans Morgonpasset i P3 hör du i Sveriges Radios app.Hur undviker man att bli skjuten? Fäbojäntan – men av en feministisk teatergrupp? Ja, tack! Tareq Taylor är här! Vi snackar Här är ditt kylskåp, dark Tareq och hur en levande orm egentligen smakar. Babs Drougge från P3 Nyheter om Louvrenkuppen var ett inside job och om det blir nyva? I hennes hål i dag: girandole torsades. Linnéa Wikblad berättar om sin barndomshobby – att lemlästa dockor och sminka sig något av det grövsta. Så säger killar ”jag älskar dig” till sina killkompisar, enligt Druid. En val som pratar på en frekvens ingen annan val hör har blivit viral – är det världens mest ensamma val? Vetenskapsjournalisten Izabella Rosengren är här och hjälper oss grotta i valens mysterium.Tidpunkter i avsnittet:11:56 Nyhetsfördjupning: Var Louvrenkuppen ett insiderjobb?17:34 Väldens ensammaste val44:47 Nyhetsfördjupning: Snack om nyval1:04:26 Babs privata hål: Ggirandole torsades1:16:30 Tareq TaylorKapitellänkarna ovan leder till avsnittet utan musik i Sveriges Radios app.Programledare: David Druid och Linnea Wikblad.
The indications and administration of ACLS antiarrhythmics magnesium & Procainamide for treating Torsades de Pointes and stable tachycardias.Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest.Procainamide use for stable patients with a monomorphic wide-complex tachycardia.Procainamide dosing and when to stop the infusion.Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.**American Cancer Society (ACS) Fundraiser This is the seventh year that I'm participating in Men Wear Pink to increase breast cancer awareness and raise money for the American Cancer Society's life-saving mission.I hope you'll consider contributing.Every donation makes a difference in the fight against breast cancer! Paul Taylor's ACS Fundraiser Page: http://main.acsevents.org/goto/paultaylorTHANK YOU for your support! Good luck with your ACLS class!Links: Buy Me a Coffee at https://buymeacoffee.com/paultaylor Free Prescription Discount Card - Get your free drug discount card to save money on prescription medications for you and your pets: https://safemeds.vip/savePass ACLS Web Site - Other ACLS-related resources: https://passacls.com@Pass-ACLS-Podcast on LinkedIn
Q-BANK: https://patreon.com/highyieldfamilymedicineIntro (0:35),Sinus tachycardia (1:52),Sinus bradycardia (2:53),Focal atrial tachycardia (4:08),Multifocal atrial tachycardia (5:00),Atrial fibrillation (5:56),Atrial flutter (12:16),Supraventricular tachycardia (13:27)Wolff-Parkinson-White (16:18),AV blocks (17:31),Right bundle branch block (21:16), Left bundle branch block (22:18),Premature ventricular complexes (24:12),Ventricular tachycardia (25:07),Torsades de Pointes (26:06),Ventricular Fibrillation (26:49),Electrical interventions overview (29:06),Practice questions (30:20)
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest.Procainamide use for stable patients with a monomorphic wide-complex tachycardia.Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Good luck with your ACLS class!Links: Buy Me a Coffee at https://buymeacoffee.com/paultaylor Practice ECG rhythms at Dialed Medics - https://dialedmedics.com/Free Prescription Discount Card - Download your free drug discount card to save money on prescription medications for you and your pets: https://safemeds.vipPass ACLS Web Site - Episode archives & other ACLS-related podcasts: https://passacls.com@Pass-ACLS-Podcast on LinkedIn
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest.Procainamide use for stable patients with a monomorphic wide-complex tachycardia.Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Good luck with your ACLS class!Links: Buy Me a Coffee at https://buymeacoffee.com/paultaylor Practice ECG rhythms at Dialed Medics - https://dialedmedics.com/Free Prescription Discount Card - Download your free drug discount card to save money on prescription medications for you and your pets: https://safemeds.vipPass ACLS Web Site - Episode archives & other ACLS-related podcasts: https://passacls.com@Pass-ACLS-Podcast on LinkedIn
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG. Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@Pass-ACLS-Podcast on LinkedInGive Back & Help Others: Your support helps cover the monthly cost of software and podcast & website hosting. Donations at Buy Me a Coffee at https://buymeacoffee.com/paultaylor are appreciated and will help ensure others can benefit from these tips as well.Good luck with your ACLS class!Helpful Listener Links:Practice ECG rhythms at Dialed Medics - https://dialedmedics.com/
1005: Does a pacemaker or implanted cardiac defibrillator suggest a higher or lower risk of medication-induced torsades?
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode1005. In this episode, I'll discuss whether a pacemaker or implanted cardiac defibrillator (ICD) protects from medication-induced torsades. The post 1005: Does a pacemaker or implanted cardiac defibrillator suggest a higher or lower risk of medication-induced torsades? appeared first on Pharmacy Joe.
In this episode, we review the high-yield topic Torsades de Pointes from the Cardiovascular section at Medbullets.com Follow Medbullets on social media: Facebook: www.facebook.com/medbullets Instagram: www.instagram.com/medbulletsofficial Twitter: www.twitter.com/medbullets Linkedin: https://www.linkedin.com/company/medbullets
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@Pass-ACLS-Podcast on LinkedInGive Back & Help Others: Your support helps cover the monthly cost of software and podcast & website hosting so that others can benefit from these ACLS tips as well. Donations via Buy Me a Coffee at https://buymeacoffee.com/paultaylor are appreciated.Good luck with your ACLS class!Listen to Pass ACLS tips and other medical podcasts at ConveyMed.io
We're seeing a lot of "bespoke" things lately... but there's only one true bespoke cure for Torsades. Let's cover this HARD board-style question. Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind at here. Cite this podcast as: Briggs, Blake; Husain, Iltifat. 239. Torsades & Charcuterie. November 18th, 2024. Accessed [date].
JACC: Advances - Repolarization Injury and Occurrence of Torsades de Pointes During Acute Takotsubo Syndrome
Darshan H. Brahmbhatt, Podcast Editor of JACC: Advances, discusses a recently published original research paper on repolarization injury and occurrence of Torsades de Pointes during acute Takotsubo syndrome.
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG. Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@Pass-ACLS-Podcast on LinkedInGive Back & Help Others: Your support helps cover the monthly cost of software and podcast & website hosting so that others can benefit from these ACLS tips as well. Donations made via Buy Me a Coffee at https://buymeacoffee.com/paultaylor are appreciated.Make a difference in the fight against breast cancer by donating to my Men Wear Pink fundraiser for the American Cancer Society (ACS) at http://main.acsevents.org/goto/paultaylor Every dollar helps in the battle with breast cancer.Good luck with your ACLS class!
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia.Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@PassACLS on X (formally known as Twitter)@Pass-ACLS-Podcast on LinkedInGive back & help others. Your support will help cover the monthly cost of software and podcast & website hosting. Donations made via Buy Me a Coffee at https://buymeacoffee.com/paultaylor are appreciated.Good luck with your ACLS class!
929: What is the incidence of torsades from low-dose ondansetron in peri-operative patients?
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode929. In this episode, I'll discuss the incidence of torsades from low-dose ondansetron in peri-operative patients. The post 929: What is the incidence of torsades from low-dose ondansetron in peri-operative patients? appeared first on Pharmacy Joe.
Treating Traumatic Brain Injury with Ibogaine | Dr. Nolan Williams ~ ATTMind 188
Nolan Williams, MD joins to talk about brain injury, ibogaine, and the incredible results of his study (conducted at Ambio Life Sciences Center) on ibogaine for treatment of traumatic brain injury, "concussions" in particular. We also talk about ibogaine as an oneirogen; the cardiac risks of ibogaine; how ibogaine compares to other treatments methods for brain injury, including other psychedelics; microdosing ibogaine for traumatic brain injury; and that ibogaine can seemingly “de-age” the brain. Additionally, we talk about context vs pharmacology in the healing benefits of psychedelics; separating high-technology from time; and how and why using the vehicle of capitalism to fund psychedelic research may be a good thing. Enjoy ... For links to Dr. Williams' work, full show notes, and a link to watch this episode in video, head to bit.ly/ATTMind188 *** FULL TOPICS BREAKDOWN BELOW** SUPPORT THE PODCAST Become a member of my Patreon: https://patreon.com/jameswjesso Toss me a tip on PayPal: https://www.paypal.com/biz/fund?id=383635S3BKJVS Toss my a Tip on Ko-Fi: https://ko-fi.com/jameswjesso Buy some merchandise: https://www.jameswjesso.com/shop/ More Options: https://www.jameswjesso.com/support Newsletter: https://www.jameswjesso.com/newsletter Telegram Channel: https://t.me/jameswjesso *** Huge thanks to my patrons on Patreon! In particular, my $23+ patrons; Andreas D, Ian C, Alex F, Eliz C, Joe A; Episode Breakdown (00:00:00) Opening (00:01:04) Dr. Williams' Bio (00:04:15) Patreon Thanks (00:05:51) Interview begins (00:07:56) An explanation of traumatic brain injury (TBI) and their different severity—mild, moderate, severe (00:13:49) The impact of TBI on the person and society (00:16:33) Restoring brain function through psychedelics (00:20:03) TBI is an “invisible injury” that can express a huge range of symptoms (00:23:30) The substantial (but presently unknown) prevalence of TBI in society (00:28:05) The Western history of medical ibogaine (00:30:11) The pharmacological and psychological effects of ibogaine (00:31:50) Is ibogaine an oneirogen? (splitters vs lumpers) (00:34:10) Reducing stigma against Ibogaine by avoiding the term “psychedelic” (00:37:32) It's difficult to get approval for ibogaine research due to mortality risks (00:39:03) The cardiac risks of ibogaine; how and why ibogaine can stop your heart—Torsades (00:43:13) What inspired Dr. Williams to investigate ibogaine (00:46:11) The details of the treating traumatic brain injury with ibogaine study (00:50:55) The details of the treating traumatic brain injury with ibogaine study (00:52:54) Why their study focused on Veterans (00:56:50) Concussions are “mild TBI”; ibogaine treatment study was with people who had mTBI (01:00:13) The incredible results of this study: a significant reversal of their disability status (01:03:27) Context vs pharmacology in the healing benefits of psychedelics (01:14:19) The ibogaine life review seems to happened regardless of context (01:17:26) How ibogaine compares to other TBI treatments methods (01:20:34) Ibogaine vs other psychedelics in the treatment of traumatic brain injury (01:22:11) Are ibogaine's effects a “random” result of evolution? (01:24:57) What it is about ibogaine pharmacologically that makes it so effective for brain injury (01:26:11) The key metaphor of ibogaine (01:27:48) Ibogaine can “de-age” the brain (01:32:51) Separating high-technology from time (01:33:53) Using the vehicle of capitalism to fund psychedelic research is a good thing (?) (01:38:19) Mircodosing ibogaine for traumatic brain injury (01:43:01) What's Next for Dr. Williams (01:44:16) Follow-up links and Socials for Dr. Williams
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@PassACLS on X (formally known as Twitter)@Pass-ACLS-Podcast on LinkedInGive back - buy Paul a bubble tea hereGood luck with your ACLS class!
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of torsades on the ECG. Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@PassACLS on X (formally known as Twitter)@Pass-ACLS-Podcast on LinkedInGive back via PayPal Good luck with your ACLS class!
343. Cardio-Oncology: Arrhythmias in CardioOncology with Dr. Michael Fradley
CardioNerds (Dr. Daniel Ambinder, Dr. Giselle Suero Abreu, Dr. Kahtan Fadah, and Dr. Colin Blumenthal) discuss arrhythmias in CardioOncology with Dr. Michael Fradley. In this episode, Dr. Michael Fradley joins us in the CardioNerds CardioOncology clinic where he uses his unique dual training in cardio-oncology and electrophysiology to walk us through the complex interplay and management of these disorders. We discuss the incidence and pathophysiology of these arrhythmias, including the link with various cancer treatments, screening and detection, and complex management including rate vs rhythm control in atrial fibrillation, need for anticoagulation, effects on the QTc and so much more. Given the unique challenges with this population we also delve into how this affects their oncology care and how to approach changes to their cancer treatment. Show notes were drafted by Dr. Kahtan Fadah and episode audio was edited by student Dr. Tina Reddy. This episode is supported by a grant from Pfizer Inc. This CardioNerds Cardio-Oncology series is a multi-institutional collaboration made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Giselle Suero Abreu, Dr. Dinu Balanescu, and Dr. Teodora Donisan. CardioNerds Cardio-Oncology PageCardioNerds Episode PageCardioNerds AcademyCardionerds Healy Honor Roll CardioNerds Journal ClubSubscribe to The Heartbeat Newsletter!Check out CardioNerds SWAG!Become a CardioNerds Patron! Pearls and Quotes - Arrhythmias in CardioOncology Arrhythmias are common in cancer patients due to shared risk factors and bi-directional risk between cardiac and oncologic disorders. Many cancer therapeutics can be directly arrhythmogenic or lead to cardiotoxicities that pre-dispose to arrhythmias. Though incidence of arrhythmia can be significant increased with some cancer therapeutics (e.g. ibrutinib), there is not specific data to support proactive ambulatory monitoring for arrhythmia without evidence of clear symptoms. Atrial fibrillation is the most common arrhythmia in cancer patients and management of atrial fibrillation, as well as other tachyarrhythmias, is unchanged from management in non-cancer patients. General principles of when to start anticoagulation or rate vs rhythm control are not significantly different (e.g. still use CHA2DS2-VAsC, monitor for symptoms etc), but providers should be more mindful of drug-drug interactions with cancer therapeutics. Cancer therapeutics as well as common medications used to treat side effects or complications (e.g. antiemetics, antibiotics, etc) can prolong the QT interval and increase risk of Torsades de pointes (TdP). The QTc should be monitored with an ECG for patients on these medications. If a patient does develop a serious arrhythmia like TdP, management is similar to that in non-cancer patients. The goal of arrhythmia management in cardio-oncology is to prevent cardiovascular disease from becoming a barrier to appropriate cancer therapy. Though cancer therapeutics should be temporarily or permanently discontinued in potentially fatal events (e.g TdP from QTc prolonging meds), the overall goal is to manage the arrhythmias appropriately to allow cancer therapeutics to be continued or restarted. Show notes - Arrhythmias in CardioOncology What is the prevalence of arrhythmias in patients with cancer? Arrhythmias are common in patients with cancer due to a multitude of factors. Atrial fibrillation is the most common arrhythmia in this population and occurs in approximately 5% of patients with cancer. The driving forces are multifactorial and include the direct arrhythmogenic effects of cancer therapeutics and cardiotoxicities of cancer therapeutics that make arrhythmogenesis more likely. Additionally, there is a bi-directional link between cancer and cardiac disorders. For example, not only is atrial fibrillation more common in patien...
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of torsades on the ECG. Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.**American Cancer Society (ACS) Fundraiser This is the fifth year that I'm participating in Men Wear Pink to increase breast cancer awareness and raise money for the American Cancer Society's life-saving mission.I hope you'll consider contributing.Every donation makes a difference in the fight against breast cancer! Paul Taylor's ACS FundraiserTHANK YOU! Connect with me:Website: https://passacls.com@PassACLS on Twitter@Pass-ACLS-Podcast on LinkedInGive back & support the show:via PayPal Good luck with your ACLS class!
Les pharmaciens sont fréquemment confrontés à des interactions qui peuvent faire allonger l'intervalle QT et augmenter le risque de torsades de pointe. Quelle conduite privilégier pour prévenir les torsades de pointe d'origine médicamenteuse? Qui sont les patients les plus susceptibles de développer ce type d'arythmie et quels outils sont disponibles pour évaluer le risque? Quand faut-il intervenir? Pour nous guider à travers ces questions, Trait pharmacien reçoit Geneviève Cyr, pharmacienne à l'Institut de cardiologie de Montréal. NOUVEAUTÉ! Les membres de l'A.P.E.S. peuvent réclamer des UFC en réussissant un questionnaire d'évaluation des apprentissages! https://bit.ly/3PaDAuJ Références : Site Web de CredibleMeds : https://crediblemeds.org/ Vandael E et coll. Development of a risk score for QTc-prolongation: the RISQ-PATH study. Int J Clin Pharm 2017;39(2):424-32. Vandael E et coll. A smart algorithm for the prevention and risk management of QTc prolongation based on the optimized RISQ-PATH model. Br J Clin Pharmacol 2018;84(12):2824-35. Tisdale JE et coll. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes 2013;6(4):479-87. Haugaa KH et coll. Institution-wide QT alert system identifies patients with a high risk of mortality. Mayo Clin Proc 2013;88(4):315-25.
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach. Connect with me:Website: https://passacls.com@PassACLS on Twitter@Pass-ACLS-Podcast on LinkedInGive back & support the show:via PayPal Good luck with your ACLS class!
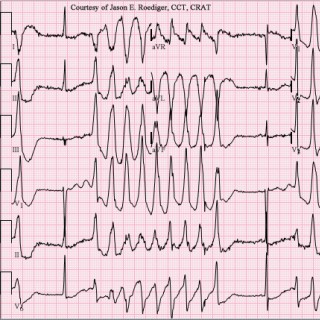
Contributor: Travis Barlock MD Educational Pearls The QT interval represents phases 2 and 3 of ventricular plateau and repolarization, respectively. As the QT interval lengthens, more sodium and calcium channels are available and susceptible to action potentials. Prolonged QT interval is more concerning in the setting of bradycardia. This scenario increases the likelihood of R on T phenomenon. R on T phenomenon occurs due to an early afterdepolarization event in which a premature ventricular contraction (PVC) occurs during the repolarization period (superimposed on the T wave), leading to an aberrant re-entry circuit. The re-entry circuit leads to Torsades de Pointes (polymorphic ventricular tachycardia with prolonged QT) and subsequent ventricular fibrillation. Treatment for Torsades de Pointes is 2g MgSO4. The preferred antiarrhythmic for VTach is IV lidocaine 1.5 mg/kg over 2 minutes. Avoid amiodarone due to risk of further QT prolongation. A heart rate under 80 does not need QT correction Corrected QT interval is used in the setting of tachycardia due to an abnormally small T wave Correction for the QT interval in tachycardia: 472 ms for males vs. 482 ms for females References 1. Banai S, Schuger C, Benhorin J, Tzivoni D. Treatment of torsade de pointes with intravenous magnesium. Am J Cardiol. 1989;63(20):1539-1540. doi:10.1016/0002-9149(89)90033-7 2. Gorgels APM, Van Den Dool A, Hofs A, et al. Comparison of procainamide and lidocaine in terminating sustained monomorphic ventricular tachycardia. Am J Cardiol. 1996;78(1):43-46. doi:10.1016/S0002-9149(96)00224-X 3. Liu MB, Vandersickel N, Panfilov A V., Qu Z. R-From-T as a Common Mechanism of Arrhythmia Initiation in Long QT Syndromes. Circ Arrhythmia Electrophysiol. 2019;12(12):1-15. doi:10.1161/CIRCEP.119.007571 4. Sagie A, Larson MG, Goldberg RJ, Bengtson JR, Levy D. An improved method for adjusting the QT interval for heart rate (the Framingham Heart Study). Am J Cardiol. 1992;70(7):797-801. doi:10.1016/0002-9149(92)90562-D 5. Vandenberk B, Vandael E, Robyns T, et al. Which QT correction formulae to use for QT monitoring? J Am Heart Assoc. 2016;5(6). doi:10.1161/JAHA.116.003264 6. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death - Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines. Vol 114.; 2006. doi:10.1161/CIRCULATIONAHA.106.178104 Summarized by Jorge Chalit, OMSII | Edited by Meg Joyce & Jorge Chalit, OMSII
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@PassACLS on Twitter@Pass-ACLS-Podcast on LinkedInGive back & support the show:via PayPal Good luck with your ACLS class!
807: Does a pacemaker or implanted cardiac defibrillator protect from medication-induced torsades?
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode807. In this episode, I'll discuss whether a pacemaker or implanted cardiac defibrillator (ICD) protects from medication-induced torsades. The post 807: Does a pacemaker or implanted cardiac defibrillator protect from medication-induced torsades? appeared first on Pharmacy Joe.
807: Does a pacemaker or implanted cardiac defibrillator protect from medication-induced torsades?
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode807. In this episode, I ll discuss whether a pacemaker or implanted cardiac defibrillator (ICD) protects from medication-induced torsades. The post 807: Does a pacemaker or implanted cardiac defibrillator protect from medication-induced torsades? appeared first on Pharmacy Joe.
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes.Identification of torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia.Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@PassACLS on Twitter@Pass-ACLS-Podcast on LinkedInGive back & support the show:via PayPal Good luck with your ACLS class!
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes. Identification of Torsades on the ECG.Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest.Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach.Connect with me:Website: https://passacls.com@PassACLS on Twitter@Pass-ACLS-Podcast on LinkedInGive back & support the show:via PayPal Good luck with your ACLS class!
1.28 Torsades de Pointes Cardiovascular system review for the USMLE Step 1 exam.
Antiarrhythmics Review: Magnesium and Procainamide
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes. Identification of torsades on the ECG. Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach. For more information on antiarrhythmics, check out the Pod Resource Page at passacls.com. The podcast episodes from Ninja Nerd and Coffee Break HEMS are great. Connect with me: Website: https://passacls.com (https://passacls.com) https://twitter.com/PassACLS (@PassACLS) on Twitter https://www.linkedin.com/company/pass-acls-podcast/ (@Pass-ACLS-Podcast) on LinkedIn Good luck with your ACLS class!
Take Home Points Severe hypocalcemia can cause hypotension and QTc prolongation leading to Torsades de Pointes. Treat moderate to severe symptoms and any EKG changes with IV calcium salts Always search for and treat the underlying cause of hypocalcemia REBEL Core Cast 88.0 – Hypocalcemia Click here for Direct Download of the Podcast Definition: A ... Read more The post REBEL Core Cast 88.0 – Hypocalcemia appeared first on REBEL EM - Emergency Medicine Blog.
In this episode, we review the high-yield topic of Torsades de Pointes from the Cardiovascular section. Follow Medbullets on social media: Facebook: www.facebook.com/medbullets Instagram: www.instagram.com/medbulletsofficial Twitter: www.twitter.com/medbulletsIn --- Send in a voice message: https://anchor.fm/medbulletsstep1/message
Antiarrhythmics Review: Magnesium and Procainamide
Although magnesium can be used in the treatment of other medical conditions such as eclampsia, asthma, & digitalis toxicity; for ACLS, magnesium is primarily used to treat Torsades de Pointes. Identification of torsades on the ECG. Administration of a magnesium infusion for stable patients vs slow IV push for patients in cardiac arrest. Procainamide use for stable patients with a monomorphic wide-complex tachycardia. Procainamide dosing and when to stop the infusion. Tip for determining whether magnesium or Procainamide should be used when treating stable patients with V-Tach. Connect with me: Website: https://passacls.com (https://passacls.com) https://twitter.com/PassACLS (@PassACLS) on Twitter https://www.linkedin.com/company/pass-acls-podcast/ (@Pass-ACLS-Podcast) on LinkedIn Good luck with your ACLS class!
229. CardioNerds Rounds: Challenging Cases – Atrial Fibrillation with Dr. Hugh Calkins
It's another session of CardioNerds Rounds! In these rounds, Dr. Stephanie Fuentes (EP FIT at Houston Methodist) joins Dr. Hugh Calkins (Professor of Medicine and Director of the Electrophysiology Laboratory and Arrhythmia Service at Johns Hopkins Hospital) to discuss the nuances of atrial fibrillation (AF) management through challenging cases. As an author of several guideline and expert consensus statements in the management of AF and renowned clinician, educator, and researcher, Dr. Calkins gives us many pearls on the management of AF, so don't miss these #CardsRounds! This episode is supported with unrestricted funding from Zoll LifeVest. A special thank you to Mitzy Applegate and Ivan Chevere for their production skills that help make CardioNerds Rounds such an amazing success. All CardioNerds content is planned, produced, and reviewed solely by CardioNerds. Case details are altered to protect patient health information. CardioNerds Rounds is co-chaired by Dr. Karan Desai and Dr. Natalie Stokes. Speaker disclosures: None Challenging Cases - Atrial Fibrillation with Dr. Hugh Calkins CardioNerds Rounds PageCardioNerds Episode PageCardioNerds AcademyCardionerds Healy Honor Roll CardioNerds Journal ClubSubscribe to The Heartbeat Newsletter!Check out CardioNerds SWAG!Become a CardioNerds Patron! Show notes - Challenging Cases - Atrial Fibrillation with Dr. Hugh Calkins Case #1 Synopsis: A woman in her mid-60s presents with symptomatic paroxysmal atrial fibrillation (AF). An echocardiogram has demonstrated that she has a structurally normal heart. Her primary care doctor had started Metoprolol 50 mg twice a day but she has remained symptomatic. In office, an EKG confirms AF, but she converts to sinus while there. She is seeking advice to prevent further episodes and in general wants to avoid additional medications Case #2 Takeaways We discussed several potential options for treatment. Amongst the first things we discussed was amiodarone. In a patient of this nature without structural heart disease and under the age of 70, Dr. Calkins discussed that he would probably consider amiodarone as a 2nd line option. While amiodarone may be effective in maintaining sinus rhythm in comparison to other antiarrhythmic medications like sotalol, flecainide, and propafenone, it does have significant toxicity.If antiarrhythmic drugs (AAD) were to be considered, we also discussed the options of dofetilide versus sotalol. Dofetilide typically requires inpatient initiation due to the risk of QT prolongation and Torsades. Since women tend to have longer corrected QT (QTc) intervals, high dose dofetilide may be more proarrhythmogenic in women. Though, Dr. Calkins noted that many patients don't tolerate sotalol due to fatigue and generally dofetilide is well tolerated.When it comes to the “pill in the pocket” approach, Dr. Calkins noted that its utility is more so in patients with persistent AF that is known to not stop on its own. For instance, an individual who has AF a few times a year that is persistent may benefit from flecainide or propafenone (“in the pocket”) instead of being brought in for an electrical cardioversion. In this scenario, the first time one of these agents is used, the patient ought to be closely monitored. For our patient, her episodes were too frequent and self-terminating for a “pill in the pocket” approach to be effective.Current guideline recommendations for catheter ablation include a Class IA recommendation for patients with paroxysmal AF refractory to AADs, and a Class IIA recommendation as first-line therapy for patients with paroxysmal AF.In the 2020 ESC Atrial Fibrillation Guidelines, catheter ablation is given a Class IA recommendation to improve symptoms of AF recurrences in patients who have failed or are intolerant of one Class I or III AADs. For patients who have failed or have been intolerant of beta blocker alone for rhythm control,
Approach to the Toddler with Somnolence and Difficulty Breathing
Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists. I'm Pradip Kamat coming to you from Children's Healthcare of Atlanta/Emory University School of Medicine. I'm Rahul Damania from Cleveland Clinic Children's Hospital and we are two Pediatric ICU physicians passionate about all things MED-ED in the PICU. PICU Doc on Call focuses on interesting PICU cases & management in the acute care pediatric setting so let's get into our episode: Here's the case presented by Rahul: A 21-month-old girl was brought to an OSH ED for somnolence and difficulty breathing, which developed after she accidentally ingested an unknown amount of liquid medicine that was used by her grandfather. Per the mother, the patient's grandfather was given the liquid medication for the treatment of his opioid addiction. The patient took some unknown amount from the open bottle that was left on the counter by the grandfather. Immediately after ingestion of the medicine, the patient initially became irritable and had some generalized pruritus. The patient subsequently became sleepy followed by difficulty breathing and her lips turned grey. The patient was rushed to an outside hospital ED for evaluation. OSH ED: The patient arrived unresponsive and blue, she was noted to be sleepy and difficult to arouse on arrival, with pinpoint pupils and hypoxic to 88%. , but After receiving Naloxone, however, she became awake and interactive. Her glucose on presentation was 58 mg/dL and Her initial VBG resulted 7.3/49.6/+2. She continued to have intermittent episodes of somnolence without apnea. Poison control called and recommend starting a naloxone infusion; she was also given dextrose bolus. The patient was admitted to the PICU. To summarize key elements from this case, this patient has: Accidental ingestion of an unknown medication Altered mental status Difficulty breathing—with grey lips suggestive of hypoventilation/hypoxia All of which brings up a concern for a toxidrome which is our topic of discussion for today The typical symptoms seen in our patient of pinpoint pupils, respiratory depression, and a decreased level of consciousness is known as the “opioid overdose triad” Given the history of opioid addiction in the grandfather, the liquid medicine given to him is most likely methadone.In fact, in this case, the mother brought the bottle of medicine, which was subsequently confirmed to be prescription methadone given to prevent opioid withdrawal in the grandfather. To dive deeper into this episode, let's start with a multiple choice question: Which of the following opioids carries the greatest risk of QTc prolongation? A. Methadone B. Morphine C. Fentanyl D. Dilaudid The correct answer is methadone. Methadone prolongs QT interval due to its interactions with the cardiac potassium channel (KCNH2) and increases the risk for Torsades in a dose-dependent manner. Besides the effect on cardiac repolarization, methadone is also associated with the development of bradycardia mediated via its anticholinesterase properties and through its action as a calcium channel antagonist. Hypokalemia, hypocalcemia, hypomagnesemia, and concomitant use of other drugs belonging to the family of CYP3A4 system inhibitors such as erythromycin can prolong Qtc. Even in absence of these risk factors, methadone alone can prolong QTc. Thanks for that, I think it is very important to involve your Pediatric Pharmacy team to also help with management as children may be concurrent qt prolonging meds. Rahul, what are some of the pharmacological and clinical features of methadone poisoning? Methadone is a synthetic opioid analgesic made of a racemic mixture of two enantiomers d-methadone and l-methadone. besides its action on mu and kappa receptors, it is also an NMDA receptor antagonist. Due to its long action, methadone is useful as an analgesic and to suppress opioid withdrawal symptoms (hence used for opioid...
Haiki is a multimedia artist, model, pianist, singer and CEO of an NFT discord community- We Are The Foos (@wearethefoos) ‼️
Trade – Magnesium SulfateClass – Electrolyte, Tocolytic, MineralAction – Controls seizures by blocking peripheral neuromuscular transmission. Magnesium is also a peripheral vasodilator, and an inhibitor of platelet function. Indication – Torsades de Pointes, cardiac arrhythmias associated with hypomagnesemia, eclampsia and seizure prophylaxis in preeclampsia, status asthmaticus. Contraindications – AV Block, GI obstruction, use caution in renal impairment. Side effects – Mag ToxicitySigns of Mag Toxicity would include flushing, diaphoresis, hypotension, muscle paralysis, weakness, hypothermia, and cardiac, CNS, or respiratory depressionDosagesPulseless V-fib/ V-tach with Torsades de Pointes or Hypomagnesemia Adult:1 – 2 G in 10ml D5W IV,IO, over 15 mins or faster if cardiac arrestPediatric: 25 – 50mg/kg IV/IO over 10 – 20 mins or faster for Torsades- max single dose: 2GEclampsia and Seizure Prophylaxis in preeclampsia Adult:4-6G IV/O over 20-30 mins followed by 1-2G/Hr Status Asthmaticus Adult: 1.2-2G IV/IO over 20 minsPediatric:25/50mg/kg slow IV/IO over 10-20 mins
In this episode, we review the high-yield topic of Torsades de Pointes from the Cardiovascular section. Follow Medbullets on social media: Facebook: www.facebook.com/medbullets Instagram: www.instagram.com/medbulletsofficial Twitter: www.twitter.com/medbullets
690: What is the incidence of torsades from low-dose ondansetron in peri-operative patients?
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode690. In this episode, I’ll discuss the incidence of torsades from low-dose ondansetron in peri-operative patients. The post 690: What is the incidence of torsades from low-dose ondansetron in peri-operative patients? appeared first on Pharmacy Joe.
690: What is the incidence of torsades from low-dose ondansetron in peri-operative patients?
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode690. In this episode, I’ll discuss the incidence of torsades from low-dose ondansetron in peri-operative patients. The post 690: What is the incidence of torsades from low-dose ondansetron in peri-operative patients? appeared first on Pharmacy Joe.
Episode 11: Arrhythmias Part One (Tachyarrhythmias)
Welcome to our first episode of a 2-part series on arrhythmias! Here we discuss the highest-yield points on tachyarrhythmias, which include: A fib, AVRT, AVNRT, V tach, Torsades, and V fib. Hope you enjoy this HIGH-YIELD episode!
084 – Prolonged QT syndrome and Torsade de pointes with Graeme.
You are called to review a 35yr old woman at 36 weeks in labour ward who has had a couple of "funny turns" in the last 15 minutes where she became unresponsive and then seemed confused for a few minutes after. When you get there they tell you she is being induced with cervidil for premature rupture of membranes but she is not in active labour. Because of the PROM she has been started on erythromycin. She has also been unwell with hyperemesis most of the pregnancy but has been vomiting a lot over the last 2 days and has received a lot of medications to try and get on top of it including, ondansetron, droperidol, famotidine and maxalon - with only limited effect. She looks pretty thin and she says she has had a lot of trouble with her weight / nutrition because of her chronic nausea. The team have done some observations on her - she has a heart rate of 57/min, BP 100/55, she is afebrile and not tachypneic. At this stage the team thinks maybe she is fainting because she is a bit dehydrated but decide to send off some bloods and to do an ECG "to make sure there is nothing else going on". Her bloods come back and her potassium is only 2.2 and she is anaemic Hb 95. The ECG shows the following - what's wrong? (Image borrowed from LITFL - Hypokalaemia ECG changes • LITFL • ECG Library) Suddenly she passes out again whilst the ECG is attached, what are you going to do? Image borrowed from LITFL - Polymorphic VT and Torsades de Pointes (TdP) • LITFL Join Graeme and I as we discuss another fascinating topic after having a couple of patients recently with this challenging but fascinating syndrome.....
133. Case Report: Ventricular Arrhythmias & Heart Failure – A Shocking Diagnosis – University of Chicago
CardioNerds (Amit Goyal and Daniel Ambinder), join cardiology fellows from the University of Chicago, (Dr. Mark Belkin, Dr. Ian Hackett, and Dr. Shirlene Obuobi) for an important discussion about case of a woman presenting with implantable cardioverter-defibrillator (ICD) discharges found to be in ventricular tachycardia (VT) storm and work through the differential of ventricular arrhythmias, etiologies of heart failure, and indications for permanent pacemaker and ICD placement. Advanced imaging modalities that aid in the diagnosis of cardiac sarcoidosis, manifestations and management of cardiac sarcoidosis are also discussed. Dr. Nitasha Sarswat and Dr. Amit Patel provide the E-CPR for this episode. Audio editing by CardioNerds Academy Intern, Leticia Helms. Claim free CME just for enjoying this episode! Disclosures: Dr. Amit Patel disclosed ownership of small stocks in GE Healthcare Bio-Sciences. Jump to: Case media - Case schematic & teaching - References CardioNerds Case Reports PageCardioNerds Episode PageCardioNerds AcademyCardionerds Healy Honor Roll CardioNerds Journal ClubSubscribe to The Heartbeat Newsletter!Check out CardioNerds SWAG!Become a CardioNerds Patron! Case Media Click to Enlarge Episode Teaching Pearls The etiology of wide-complex tachycardias (WCT) of ventricular origin can be broken down by structurally normal versus structurally abnormal hearts. WCT in structurally normal hearts can be further broken down into idiopathic or primary arrhythmia syndromes. WCT in structurally abnormal hearts can be broken down into ischemic and non-ischemic etiologies.In patients with an unexplained non-ischemic cardiomyopathy, conduction abnormalities and/or ventricular arrhythmias should raise suspicion for cardiac sarcoidosis. Additional manifestations include atrial arrhythmias and pulmonary hypertension.Accurate diagnosis and treatment of cardiac sarcoidosis often requires multimodality cardiovascular imaging. Check out these terrific videos from Cardiac Imaging Agora: 1) PET for inflammation/sarcoidosis and 2) Echo and CMR for sarcoidosis.While a pathological tissue diagnosis is the gold-standard, endomyocardial biopsy has a low sensitivity, weven when paired with image guidance. Remember to consider extra-cardiac sites for biopsy.Decisions regarding ablation of ventricular arrhythmia or ICD placement should be done individually with careful assessment of active inflammation secondary to cardiac sarcoidosis and possible response to immunosuppressive medications.Management of cardiac sarcoidosis has two basic principles: 1) Treat the underlying process with immunosuppression and 2) Treat the cardiac sequelae: heart failure, conduction abnormalities, ventricular arrhythmias, atrial arrhythmias, and pulmonary hypertension. Notes 1. The patient in this case was found to be in VT storm. Taking a step back, when we suspect a wide complex tachycardia (WCT) is VT, what are some etiologies we should keep in mind? Differentiating between a supraventricular vs. ventricular origin of a WCT will be a topic for a future episode! But after you have determined that the origin of WCT is ventricular, considerations for the underlying etiology should include ischemia-related, non-ischemic cardiomyopathy-associated, primary arrhythmia syndromes and idiopathic (in addition to common considerations such as medications and electrolyte abnormalities)Chronic ischemia-related WCT is typically scar-mediated, a result of re-entrant mechanism and more commonly presenting as monomorphic VT. WCT in the setting of acute ischemia is likely a result of combination increased automaticity and re-entry, typically manifesting as polymorphic VT. In fact, acute ischemia is the most common cause of polymorphic VT, not Torsades de Pointes, and should be our first consideration. Torsades de Pointes specifically occurs due to an early afterdepolarization in a patient with an acqui...
Torsades de Pointes (TdP) A type of polymorphic ventricular tachycardia that is inherently unstable and often quickly degrades into ventricular fibrillation. It usually occurs in the setting of a prolonged QT interval, which can either be genetic or acquired. Treatment Defibrillation – per ACLS, ventricular tachycardia with a pulse should receive synchronized cardioversion. But in […]
Torsades de Pointes (TdP) A type of polymorphic ventricular tachycardia that is inherently unstable and often quickly degrades into ventricular fibrillation. It usually occurs in the setting of a prolonged QT interval, which can either be genetic or acquired. Treatment Defibrillation – per ACLS, ventricular tachycardia with a pulse should receive synchronized cardioversion. But in […]
Ep 154: 4-Step Approach to Bradycardia and Bradydysrhythmias
How do we figure out when bradycardia is due to a medical illness and when it is a primary cardiac problem? What are the 4 immediate life threatening diagnosis that we have to entertain and address in the first few minutes of the sick bradycardic patients? What are some key ECG patterns that are sometimes missed by ED docs that can have devastating consequences? How can we better understand Torsades de Pointes by understanding AV blocks? How can we better understand Mobitz l and ll using 'The Dorian' approach? What is BRASH syndrome and how can we recognize it? In this main episode podcast 4-step Approach to Bradycardia and Bradydysrhythmias with electrophysiologist, educator and researcher Dr. Paul Dorian and Chair of Education for the ED at Cook County Hospital Dr. Tarlan Hedayati, we dig deep into bradycardia... The post Ep 154: 4-Step Approach to Bradycardia and Bradydysrhythmias appeared first on Emergency Medicine Cases.
December 4, 2001. A bad day, indeed. That's the day the FDA issued a black box warning for droperidol, citing evidence of QT prolongation, Torsades de Pointes, and death. This was a surprise warning because droperidol had been extensively used by emergency medicine and anesthesiology for decades without apparent problems. Since this bad day, we've essentially been without droperidol. Fortunately, it's back! Before we start using it again, we should take a look at what got this drug on the FDA's radar. Dr. Jarvis reviews the literature about the “evidence” behind the warning and describes how his systems will be bringing droperidol back into practice.
Pediheart Podcast #150: Exercise Training Effects On Repolarization Abnormalities Mimicking LQTS
This week in a co-branded episode with the SADS Foundation (SADS.ORG), we speak with Professor Peter Schwartz of University of Pavia about a recent work he authored on the topic of changes in repolarization amongst well trained athletes. Can athletic training masquerade as LQTS causing prolongation and/or abnormalities in the QT interval? How can these patients be properly identified and not 'lumped' into the LQTS 'pile'? This is a very important work by one of the foremost authorities on the planet on LQTS and Professor Schwartz also shares with us how he became interested in this topic 50+ years ago as well as some pearls for clinical investigators at the start of their careers. One of the best and most inspirational interviews of the entire 150 episode series! doi: 10.1161/CIRCULATIONAHA.120.048916
This episode covers torsades de pointes!
Circulation: Arrhythmia and Electrophysiology June 2020 Issue
Paul J. Wang: Welcome to the monthly podcast, On the Beat for Circulation: Arrhythmia and Electrophysiology. I'm Dr. Paul Wang, editor in chief, with some of the key highlights from this month's issue. In our first paper, Vivek Reddy and associates studied a novel, 7.5, French lattice tip catheter with the compressible 9 mm nitinol tip that is able to deliver either focal radio frequency ablation [RFA] or pulsed field ablation [PFA], 2 to 5 second lesions. In a 3 center, single-arm, first in human trial, the catheter was used with a custom mapping system to treat paroxysmal or persistent atrial fibrillation. Toggling between energy sources, point by point, pulmonary vein [PV] encirclement was performed using biphasic pulsed field ablation, posteriorly, and either temperature controlled irrigated RFA or pulse field ablation, anteriorly (RF/PF or PF/PF) respectively. Linear lesions were created with either PFA or RFA. The 76 patient cohort included 55 paroxysmal and 21 persistent atrial fibrillation [AF] patients undergoing either RF/PF [pulse field ablation] 40 patients or PF/PF ablation in 36 patients, pulmonary vein isolation therapy duration was 22.6 minutes per patient with a mean of 50.1 RF/PF ablation lesions per patient. Linear lesions included 14 mitral, 34 left atrial roof and 44 cavo-tricuspid isthmus lines with therapy duration times of 5.1, 1.8 and 2.4 min/patient respectively. All lesion sets were acutely successful using 4.7 minutes of fluoroscopy. There were no device-related complications, including no strokes. Post-procedure esophagogastroduodenoscopy revealed minor mucosal thermal injury in two of the 36 RF/PF and zero of the 24 PF/PF patients. Post-procedure brain MRI revealed DWI positive flair, negative and DWI positive flare positive asymptomatic lesions in 5 and 3 of the 51 patients respectively. In our next paper, Moussa Saleh and associates examined whether chloroquine, hydroxychloroquine plus or minus azithromycin lead to a prolongation of the QT interval, possibly increasing the risk of torsades de pointes and sudden death in a hospitalized population of patients with COVID-19. 201 patients were treated for COVID-19 with chloroquine/hydroxychloroquine. 10 patients or 5% received chloroquine, and 191 or 95% received hydroxychloroquine and 119 or 59% also received azithromycin. The primary outcome of Torsades de pointes was not observed in the entire population. Baseline QTC interval did not differ between patients treated with chloroquine or hydroxychloroquine monotherapy versus those treated with combination group chloroquine/hydroxychloroquine and azithromycin (440 ms versus 439.9 ms). The maximum QT during treatment was significantly longer in the combination versus the monotherapy group, 470 ms versus 453 ms (P = 0.004). Seven patients (3.5%) required discontinuation of these medications due to QTC prolongation. No arrhythmic deaths were reported. In our next paper, Mikko Tulppo and associates examine whether the association between leisure time physical activity and the risk of sudden death and non-sudden cardiac death in coronary artery disease patients. 1,946 patients with angiographically verified coronary artery disease were classified into four groups: inactive, irregularly active, active exercise regularly two to three times per week, and highly active, exercise four times or more weekly. During follow-up, median 6.3 years, 52 sudden cardiac death and 49 non-sudden cardiac deaths occurred. Inactive patients had increased risk for sudden cardiac death compared to active patients, hazard ratio 2.45. Leisure time was not associated with sudden cardiac death in patients with Canadian cardiovascular class one, 18 events in 1,107 patients. Among patients with Canadian cardiovascular society, class two or higher, 34 events in 839 patients. An increased risk for sudden cardiac death encountered in highly active patients, hazard ratio 7.46 (P < 0.001). In inactive patients hazard ratio 3.64 as compared to active patients. A linear association was observed between leisure time, physical activity and non-sudden cardiac death. Those with high leisure time physical activity had the lowest risk for non sudden cardiac death. In our next paper, Jacob Koruth and associates examined the preclinical feasibility and safety of a 9mm lattice tip catheter with focal biphasic pulse field [PF] based thoracic vein isolation and linear ablation combined focal biphasic pulse field and radio-frequency [RF] focal ablation and vocal biphasic pulse field delivered directly on top of the esophagus. They treated two cohorts of six swine with pulse fields at low dose and high dose followed for four weeks and two weeks, respectively to isolate 25 thoracic veins and to create five right atrial low dose PF, six mitral high dose PF, and six roof lines with combined RF and high dose PF. Baseline and follow-up voltage mapping, venus potentials, ostial diameters and phrenic nerve viability were assessed. High dose PF in RF lesions were delivered in 4 and 1 swine from the inferior vena cava onto a forcefully deviate esophagus. 100% of thoracic veins, 25 out of 25, were successfully isolated with 12.4 applications per vein with a mean pulse field times of less than 90 seconds per vein. Durable isolation improved from 61.5% in the low dose pulse field to 100% with a high dose pulse field (P = 0.04). And all linear lesions were successfully completed without incurring venous stenosis or phrenic injury. High dose pulse field sections had higher trans mortality rates than low dose pulse field (98.3% versus 88.1%, P = 0.03). Despite greater thickness, 2.5 versus 1.3 mm, pulse field lesions demonstrated homogeneous fibrosis without epicardial fat, nerve or vessel involvement. In comparison, combined RF plus high dose PF sections revealed similar transmurality, but expectedly more necrosis, inflammation and epicardial fat, nerve and vessel involvement. Significant ablation related esophageal and necrosis inflammation and fibrosis were seen in all RF sections as compared to no PF sections. In our next paper, Hagai Yavin and associates investigated the effects of a novel, lattice tip catheter designed for focal radiofrequency ablation [RFA] or pulse field ablation in 25 swine. In 14 animals, they examined in step one (n = 14) the feasibility to create atrial line of block and described as acute effects on the phrenic nerve and esophagus. In step two (n = 7), they examined the subacute effects of pulse field ablation on block durability, phrenic nerve, and esophagus 2 or more weeks. In 4 animals in step three, they compare the effects of pulse field ablation and RFA on the esophagus using a mechanical deviation model, approximating the esophagus through the right atrium in 4 and direct ablation honest lumen in 4. The effects of endocardial PFA and RFA on the phrenic nerve were also compared (n = 10). Histological analysis were performed. Pulse field ablation produced acute block in 100% of lines achieved with 2.1 applications per centimeter line. Histological analysis following a mean of 35 days showed 100% transmurality (thickness range 0.4 to 3.4 mm) with a lesion width of 19.4 mm. Pulse field ablation selectively affected cardiomyocytes, but spared blood vessels and nervous tissue. Pulse field ablation applied from the posterior atrium to the approximated esophagus produced transmural lesions without esophageal injury. Pulse field ablation applied within the esophageal lumen produced mild edema compared to radiofrequency ablation (13 applications) which produced epithelial ulcerations. Pulse field ablation resulted in no or transient stunning of the phrenic nerve, less than 5 minutes without histological changes while radiofrequency ablation produced paralysis. In our next paper, Elad Anter and associates investigated the optimal methods to identify arrhythmogenic substrate of scar related VT. They examine how often sites of activation slowing during sinus rhythm co localize with ventricular tachycardia VT circuit. In a multicenter study in patients with infarct-related VT, the left ventricle was mapped during activation from three directions, sinus rhythm, or atrial pacing, right ventricular and left ventricular LV pacing at 600 ms. Ablation was applied selectively to the cumulative area of slow activation defined as a sum of all regions with activation time of 40 ms or greater per 10 mm. Hemodynamically tolerated ventricular tachycardias or VT were mapped with activation or entrainment. The primary outcome was a composite of appropriate ICD therapies and cardiovascular death. In 85 patients, the left ventricle was mapped during activation from 2.4 directions. The direction of LV activation influenced the location and magnitude of activation slowing. The spacial overlap of activation slowing between sinus rhythm and right ventricular RV pacing was 84.2%, between sinus rhythm and LV pacing was 61.4%, and between right ventricular and left ventricular pacing, 71.3% (P < 0.05) between all comparisons. Mapping during sinus rhythm identified only 66.2% of the entire area of activation slowing and 58% of critical isthmus sites. Activation from other directions, right ventricular or left ventricular stimulation unmasked an additional 33% of slowly conducting zones and 25% critical isthmus sites. The area of maximal activation slowing often corresponded to the site where the wavefront first interacted with the infarct. During a follow-up period of 3.6 years, the primary end point incurred in 14 out of 85 or 16.5% of patients. The authors concluded that the spatial distribution of activation slowing is dependent on the direction of LV activation with the area of maximal slowing corresponding to the site where the wavefront first interacts with the infarct. In our next paper, Georg Gussak and associates identified a novel form of abnormal calcium wave activity in normal and failing dog atrial myocytes, which occurs during the action potential and is absent during diastole. The goal of this study was to determine if triggered calcium waves affect cellular electrophysiological properties. The authors use simultaneous recordings of intracellular calcium, and action potentials for the measurement of maximum diastolic potential and action potential duration during triggered calcium waves in isolated dog atrial myocytes. Computer simulations then explored electrophysiological behavior arising from triggered calcium waves at the tissue scale. At 3.3 to five Hertz, triggered calcium waves occurred during the action potential and outlasted several action potential cycles. Maximum diastolic potential was reduced and actual potential duration was significant prolonged during trigger calcium waves. All electrophysiological responses that triggered calcium waves were abolished by using SCA 0400 and ORM 10103, indicating that sodium calcium exchange current caused depolarization. The time constant recovery from inactivation of calcium current was 40 to 70 ms in atrial myocytes, depending on the holding potential. This current could be responsible for action potential (AP) activation during repolarization induced by triggered waves. Modeling studies demonstrate the characteristic properties of triggered calcium waves are potentially arrhythmogenic by promoting both conduction block and reentry arising from the repolarization induced by triggered calcium waves. The authors concluded that triggered calcium waves activate inward sodium calcium exchange and dramatically reduce atrial maximum diastolic potential and prolonged action potential duration establishing the substrate for reentry that could contribute to initiation and maintenance of atrial arrhythmias. In our next paper Faisal Merchant and Omid Sayadi and associates evaluate the ability of a real-time, closed loop system to record and analyze repolarization alternans from multiple intracardiac leads and deliver dynamically R-wave triggered pacing stimuli during the absolute refractory period. They examined the ability of this system to control repolarization alternans and reduce arrhythmia susceptibility, in vivo. R-wave trigger pacing can induce repolarization alternans, the magnitude of which can be modulated by varying the amplitude, pulse width, or size of the pacing vector. Using a swine model (n = 9), the authors demonstrated that to induce 1 microvolt change in the alternans voltage on the body surface, coronary sinus or left ventricle, requires a delivery charge of 0.04, 0.05 and 0.06 microcoulombs, respectively, while to induce one unit change of the case score requires a delivery charge of 0.93, 0.32 and 0.33 microcoulombs, respectively. For all body surface and intracardiac leads a Delta alternans voltage and Delta K score between baseline and R-wave triggered pace peaks increases consistently with an increase in the pacing pulse amplitude, pulse width and vector spacing. Additionally, the author showed that the proposed method can be used to suppress spontaneously occurring alternans (n = 7), in the presence of myocardial ischemia. Suppression of repolarization alternans by pacing during the absolute refractory period results in a significant reduction in arrhythmia susceptibility, evidenced by lower S rank score during program ventricular stimulation compared to baseline prior to ischemia. In a perspective outlining the cardiovascular effects of chloroquine and hydroxychloroquine, Ohad Oren and associates describe their belief that the use of chloroquine and hydroxychloroquine in COVID-19 should be limited to randomized, controlled trials. For critically ill patients, unable to enroll in a trial, selective in-hospital use could be considered with careful clinical monitoring in keeping with the FDA's emergency use authorization. The authors suggested that studies evaluating chloroquine and hydroxychloroquine should systematically collect baseline demographic data, results from electrocardiographic and echocardiographic monitoring prior to and during treatment and rates of adverse cardiovascular events in both the near and long-term. In a research letter, Federico Migliore and Alessandro Zorzi and associates found a 28% decrease in the number of urgent pacemaker implantations during the six weeks after the first COVID-19 case, from 122 to 88 (P = 0.02), compared to the six weeks before the first COVID-19 case. The proportion of female patients requiring urgent pacemaker implantation after the COVID-19 outbreak decreased from six out of 122 (49%) to 30 out of 88 (34%) (P = 0.03). In a special report Stephanie Kochav and associates described 4 cases of cardiac arrhythmias in COVID-19, including AV block, atrial fibrillation, polymorphic ventricular tachycardia, and pulseless electrical activity arrest. In a year in review, Suraj Kapa and associates discuss a number of the many advances in our understanding of arrhythmia mechanisms, diagnosis, and new therapies in the past year. Data suggests that secretoneurin may be a marker for patients at risk of ventricular arrhythmias, while natriuretic peptide receptor C may have a role in atrial fibrosis. In atrial specific 2-pore potassium channel TASK-1 may be a therapeutic target for atrial fibrillation. Sensory neurons may play a key role in sleep apnea related to atrial fibrillation. Bariatric surgery is associated with improved atrial fibrillation outcome. Artificial intelligence applied to electrocardiography has yielded estimates of age, gender, and overall health. We've seen new tools for collection of patient centered outcomes following catheter ablation. There's been significant advances in the ability to identify ventricular tachycardia termination sites through high density mapping of deceleration zones. We've learned that right ventricular dysfunction may be a predictor of survival benefit after ICD implantation in non ischemic cardiomyopathy patients. We've seen further insights in the role of his bundle pacing on improving outcomes. As our understanding of cardiac laminopathies advance, we have new tools to predict arrhythmic event rates in gene carriers. And finally, we've seen numerous advances in the treatment of arrhythmias in patients with congenital heart disease. That's it for this month. We hope that you'll find the journal to be the go-to place for everyone interested in the field. See you next time. This program is copyright American Heart Association 2020.
Circulation: Arrhythmia and Electrophysiology August 2020 Issue
Paul J. Wang: Welcome to the monthly podcast! On the Beat for Circulation: Arrhythmia and Electrophysiology. I'm Dr. Paul Wang, Editor-in-Chief. With some of the key highlights from this month's issue. Paul J. Wang: In our first paper, Demilade Adedinsewo and associates assess the accuracy of an artificial intelligence-enabled electrocardiogram [AI-ECG] to identify patients presenting with dyspnea who have left ventricular LV systolic function (defined as LV ejection fraction ≤35%) in the emergency department [ED]. Patients were included if they had at least one standard 12-lead electrocardiogram [ECG] acquired on the date of the ED visit and an echocardiogram performed within 30 days of presentation. Patients with prior LV systolic dysfunction were excluded. A total of 1,606 patients were included. Meantime from ECG echocardiogram was one day. The AI-ECG algorithm identified LV systolic dysfunction with an area under the curve [AUC] of 0.89 and accuracy of 85.9%. Sensitivity was 74%, specificity 87%, negative predictive value 97%, and positive predictive value 40%. To identify an ejection fraction less than 50%, the AUC was 0.85, sensitivity 86%, sensitivity 63%, and specificity 91%. NT-proBNP alone with a cutoff greater than 800 identified LV systolic function with an AUC of 0.80 by comparison. Paul J. Wang: In our next paper, Mahmood Alhusseini and associates hypothesize that convolutional neural networks [CNN] may enable objective analysis of intracardiac activation in atrial fibrillation [AF]. They perform panoramic recording of bi-atrial electrical signals in AF and use the Hilbert-transform to produce 175,000 image grids in 35 patients labeled for a rotational activation by experts who showed consistency, but with variability (kappa [κ]=0.79). In each patient, ablation terminated atrial fibrillation. A CNN was developed and trained on 100,000 AF image grids validated on 25,000 grids, and then tested on a separate 50,000 grids. They found in a separate test cohort of 50,000 grids, CNN reproducibly classified AF image grids into those with or without rotational sites with 95.0% accuracy. This accuracy exceeded that of support vector machines, traditional linear discriminant, and k-nearest neighbor statistical analyses. To probe the CNN, they applied gradient weighted class activation mapping, which revealed that the decision logic closely mimicked rules used by experts (C statistic 0.96). The authors concluded that convolutional neural networks improve the classification of intercardiac AF maps compared to other analyses and agreed with expert evaluation. Paul J. Wang: In our next paper, Kenji Okubo and associates examined whether late potential LP, abolition and ventricular tachycardia [VT] non-inclusive ability predicted long-term outcomes in patients with non-ischemic cardiomyopathy [NICM] undergoing VT ablation. The total 403 patients with NICM (523 procedures) who underwent VT ablation from 2010 to 2016 were included. The underlying structural disease consists of dilated cardiomyopathy (DCM, 49%), arrhythmogenic right ventricular cardiomyopathy (ARVD 17%), postmyocarditis (14%), valvular heart disease (8%), congenital heart disease (2%), hypertrophic cardiomyopathy (2%), and others (5%). Epicardial access was performed in 57% of patients. At baseline, the LPs were present in 60% of patients, and a VT was either inducible or sustained/incessant in 85% of the cases. At the end of the procedure LP abolition was achieved in 79% of cases in VT noninducability in 80%. After a multivariate analysis, the combination of LP abolition and VT noninducibility was independently associated with free survival from VT (hazard ratio, 0.45, p = 0.0002) and cardiac death (hazard ratio 0.38, P = 0.005). The benefit of LP abolition of preventing the VT recurrence in ARVD and postmyocarditis appeared superior to that observed for DCM. Paul J. Wang: In our next paper, Domenico Corradi, Jeffrey Saffitz and associates hypothesize that structural molecular changes in atrial myocardium that correlate with myocardial injury and precede and predict postoperative atrial fibrillation [POAF] may identify new molecular pathways and targets for prevention of this common morbid complication. Right atrial appendage [RAA] samples were prospectively collected during cardiac surgery from 239 patients enrolled in the OPERA trial. 35.2% of patients experienced POAF compared to the non-POAF group. They were significantly older and more likely to have chronic obstructive pulmonary disease or heart failure. They had a higher Euro score and more often underwent valve surgery. No differences in atrial size were observed between POAF and non-POAF patients. The extent of atrial interstitial fibrosis, cardiomyocyte myocytolysis, cardiomyocyte diameter, glycogen storage, or connection 43 distribution at the time of surgery, was not significantly associated with the incidents of POAF. None of these histopathological abnormalities were correlated with level of NT pro-BNP, hs-cTnT, CRP, or oxidative stress biomarkers. The authors concluded that in sinus rhythm patients undergoing cardiac surgery, histopathological changes in RAA do not predict POAF. They did not also correlate with biomarkers of cardiac function, inflammation, and oxidative stress. Paul J. Wang: In our next paper, Mark McCauley, Liang Hong, Arvind Sridhar, and associates hypothesize that obesity decreases sodium channel NAF 1.5 expression via enhanced oxidative stress, thus reducing the sodium current and enhancing susceptibility to atrial fibrillation [AF]. They studied a diet induced obese [DIO] mouse model. Pacing induced AF in 100% of DIO mice versus 25% in controls (P 20 ms shorter than the other sites, and/or induction of AF/atrial tachycardia during measurements. LVA ablation was performed in the LA-LVA patients during the follow-up period of a mean of 62 weeks, the EP test-guided group had a significantly lower recurrence rate (19%,11/57 versus 41%, 22/54, P=0.012) and a higher Kaplan-Meier AF/AT-free survival curve compared with controls (P=0.01). No significant differences in the recurrence, and AF/AT-free survival curves between PWI (positive EP test) and non-PWI (negative EP test) subgroups were observed. Therefore, PWI for positive EP tests reduced the AF/AT recurrence in the EP test-guided group. A stepwise Cox proportional hazard analysis identified EP test-guided ablation as a factor, reducing recurrence rates. The recurrence rates in LA-LVA ablation group and EP test-guided group were similar. Paul J. Wang: In our next study, Jinxuan Lin and associates assess whether simultaneous pacing of the left and right bundle branch areas may achieve more synchronous ventricular activation than just bundle pacing alone. In symptomatic bradycardia patients, the distal electrode of the bipolar pacing lead was placed at the left bundle branch area via a transventricular-septal approach. This was used to pace the left bundle branch area, while the ring electrode was used to pace the right bundle branch area. Bilateral bundle branch area pacing [BBBP] was achieved by stimulating the cathode and anode in various configurations. BBBP was successfully performed in 22 out of 36 patients. Compared with LBBP, BBBP resulted in greater shortening of QRS duration (109.3 vs 118.4 ms, P < 0.001). LBBP resulted in paced RBBB configuration with a DRVAT of 115 ms and interventricular conduction delay of 34.0 ms. BBBP fully resolved the RBBB morphology in 18 patients. In the remaining 4 patients, RBBP pacing partially corrected the right bundle branch block. Paul J. Wang: In our next paper, Ramanathan Parameswaran, Jonathan Kalman, Geoffrey Lee and associates recorded 2-minute long segments of simultaneous inter-operative mapping of endo- and epicardial lateral right atrial [RA] wall in patients with persistent atrial fibrillation [AF] using 2 high-density grid catheters (16 electrodes, 3 mm spacing). Filtered unipolar and bipolar electrograms [EGMS] of continuous 2-minute AF recordings and electrodes locations were exported for phase analysis. They defined endocardial-epicardial dissociation [EED] as phase differences of ≥20 ms between paired endo- and epi electrodes. Wavefronts [WF] were classified as single rotations, that is single wavefront, focal waves, or disorganized activity as per standard criteria. Endo-Epi wave fronts were simultaneously compared on dynamic phase maps. Complex fractionated electrograms were defined as bipolar electrograms with directional changes occupying at least 70% of the sample area. 14 patients with persistent AF underwent cardiac surgery are included. EED was seen in 50.3% of phase maps with significant temporal heterogeneity. Disorganized activity (endo 41.3%, epi 46.8%, P = 0.0194) and single wave (endo 31.3 versus epi 28.1, P = 0.129) were the dominant patterns. Transient rotations (endo 22%, epi 19.2%, P = 0.169, mean duration 590 ms) and non-sustained focal waves (endo 1.2% and epi 1.6%, P = 0.669) were also observed. Apparent transmural migration of rotational activations (n=6) from the epi- to the endocardium was seen in 2 patients. EGM fractionation was significantly higher in the epicardium than endocardium (61.2% versus 51.6%, P < 0.0001). The authors concluded that simultaneous endo-epi phase mapping of prolonged human persistent AF recordings showed significant EED marked temporal heterogeneity, discordant and transitioning wavefronts patterns and complex fractionations. No sustained focal activity was observed. Such complex 3-dimensional interactions provide insights into why endocardial mapping alone may not fully characterize the AF mechanism and why endocardial ablation may not be sufficient. Paul J. Wang: In our next paper, Andrew Beaser and associates hypothesize that intravascular ultrasound [IVUS] could accurately visualize and quantify intravascular lead adherence and degree of intravascular lead adherence correlates with transvenous lead extraction difficulty. Serial imaging of leads occurred prior to transvenous lead extraction using IVUS. Intravascular lead adherence areas were classified as high or low grade. Degree of extraction difficulty was assessed using 2 metrics and correlated with intravascular lead adherence grade. Lead extraction difficulty was calculated for each patient and compared to IVUS findings. 158 vascular segments in 60 patients were analyzed: 141 (89%) low grade versus 17 (11%) high grade. Median extraction time (low = 0 versus high grade 97 seconds, P < 0.001) and median laser pulsations delivered (low = zero versus high grade 5,852, P < 0.001) were significantly higher in the high-grade segments. Most patients with low lead extraction difficulty score had low intravascular lead adherence grades. 86% of patients with high lead extraction difficulty score had low IVUS grade, and the degree of transvenous lead extraction difficulty was similar to patients with low IVUS grades and lead extraction difficulty scores. Paul J. Wang: In our next paper, András Bratincsák, and associates sought to create the foundation of normative ECG standards in the young using Z-scores. 102 ECG variables were collected from a retrospective cohort of 27,085 study subjects with no known heart conditions, age zero to 39 years. The cohort was divided into 16 age groups by gender. Median interquartile range and range were calculated for each variable adjusted to body surface area. Normative standards were developed for all 102 ECG variables, including heart rate; P, R, and T axis; R-T axis deviation; PR interval, QS duration, QT, and QTc interval; P, Q, R, S, and T amplitudes in 12 leads; as well as QRS and T wave integrals. Incremental Z-score values between negative 2.5 and 2.5 were calculated to establish the upper and lower limits of normal. Historical ECG interpretive concepts were reassessed and new concepts observed. The author summarized that electronically acquired ECG values based on the largest pediatric and young adult cohort ever compiled provide the first detailed, standardized, quantitative foundation of traditional and novel ECG variables. Paul J. Wang: In our next paper, Jungmin Hwang and associates hypothesize that suppressing the late sodium current may counterbalance the reduced repolarization reserve in long QT syndrome [LQTS] and prevent early depolarization [EAD] and polymorphic ventricular tachycardia [PVT]. They tested the effects of selective late sodium channel blocker GS967 on polymorphic ventricular tachycardia [PVT] induction in a transgenic rabbit model of type two using intact heart optical mapping, cellular electrophysiology, and confocal calcium imaging and computer modeling. They found that GS967 reduced ventricular fibrillation [VF] induction under a rapid pacing protocol (7 out of 14 hearts in control versus 1 out of 14 at 100 nanomolar) without altering action potential duration [APD] or restitution and dispersion. GS967 suppressed PVT incidents by reducing calcium mediated EADs and focal activity during isoproterenol perfusion (at 30 nanomolar, 7 out of 12 and a 100 nanomolar, 8 out of 12 without EADs and PVTs). Confocal calcium imaging of LQT myocytes revealed GS967 shortened calcium transient duration by accelerating sodium calcium exchanger mediated calcium efflux from cytosol, thereby reducing EADs. Computer modeling revealed the inward late sodium current potentiates EADs in the LQT setting through providing additional depolarizing currents through action potential plateau phase, and increasing intracellular sodium that decreases the depolarizing sodium calcium exchanger, thereby suppressing the action potential plateau and delaying the activation of slowly activating delayed rectifier current, IKS. Suggesting important roles in the late sodium current in regulating intracellular sodium. Thus, the authors concluded that selective late sodium channel blockade by GS967 prevents EADs and abolishes PVT in LQT rabbits by counterbalancing the reduced repolarization reserve and normalizing intracellular sodium. Paul J. Wang: In our next paper, Pietro Lazzerini, Mohamed Boutjdir and associates, hypothesize that systemic inflammation per se can significantly prolong QTc during infection via cytokine-mediated changes in potassium channel expression. They found in patients with acute infections, regardless of concomitant QT-prolonging anti-microbial therapy, QTc was significantly prolonged but rapidly normalized in parallel to C-reactive protein [CRP] and cytokine level reduction. Consistently, in Torsades de Pointes cohort, concomitant acute infections were prevalent 30% despite only a minority (25%) of these cases were treated with QT-prolonging anti-microbials. KCN J2, potassium channel expression in peripheral blood mononuclear cells was strongly correlated to that in ventricles, inversely associated to CRP and interleukin one changes in acute infection patients. The authors concluded that acute infection, systemic inflammation rapidly induces cytokine-mediated ventricular electrical remodeling and significant QTc prolongation, regardless of concomitant antimicrobial therapy. Paul J. Wang: In a research letter, Christophe Beyls and associates examined the risk of bradycardia and critically ill COVID-19 patients treated with Lopinavir [LPV], a protease inhibitor of HIV-1, and Ritonavir [RTV], another protease inhibitor that strongly inhibits hepatic cytochrome P 450 [CYP3A4] activity in order to increase the Lopinavir plasma concentration. During the first month of the outbreak, patients admitted to the ICU with positive PCR for COVID-19 received LPV (200 mg)/RVT (50 mg) twice daily for 10 days. Bradycardia was defined as heart rate below 60 for a period of more than 24 hours. All patients were monitored 24 hours a day for all hemodynamic parameters, including heart rate with a five-lead ECG. Monitors were linked to a computerized system allowing to extract hemodynamic data. LPV/RTV plasma concentration was monitored using analytic method, combining high propensity performance, liquid chromatography and tandem mass spectrometry at 72 hours and every 72 hours. They prospectively included 41 COVID-19 patients who received LPV/RTV treatment. Nine or 22% patients experienced bradycardia. No patients had a pre-existing nodal pathology on the ECG on admission. Among the 9 patients with bradycardia, 8 or 88% were sinus bradycardia and one (12%) third-degree AV block. Causality may be considered as bradycardia occurred at least 48 hours after LPV/RTV initiation, bradycardia resolved after discontinuation or dose reduction and no alternative cause was found. Patients who presented with bradycardia were older, had a higher RTV plasma concentration and a lower lymphocyte count. In our study, no correlation was found between RTV plasma concentration, LPV plasma concentration, and mean heart rate at day three. No patient had bradycardia in the first 48 hours after LPV/RTV administration. For patients with LPV RTV plasma level overdose, the dose of LPV RTV was divided by two until the next dose. For the patient with third degree AV block LPV/RTV was stopped. None of the patients had any known cytochrome CYP3A4-inhibiting drugs. The authors concluded that the results suggest that RTV plasma overdose in elderly critical ill patients may increase the risk of bradycardia. Paul J. Wang: In a research letter, Emily Zeitler and associates surveyed cardiac implantable device [CID] patients. A total of 109 patients were approached to participate, nine declined. Most respondents were white (79%), male (60%) with a mean age of 73 years. The median number of correct responses to the 11 factual questions was six. Respondents held some common misconceptions. For example, 25% of respondents believe that FDA determines the cost of the device. Trust in the FDA was high; 67% of respondents agreed "I trust the FDA". Respondents mostly agreed "the FDA would not approve my device unless it was a hundred percent safe". Only 6% of respondents agreed, "we would be better off if there was no FDA," and a similarly small fraction disagreed with "when it comes to medical devices, the U.S. does the best job in the world at keeping people safe". Most respondents, 69% demonstrated fear of device recalls by agreeing with "if there was a recall of all are part of my device, I think I would be worried or scared." On average, respondents were comfortable sacrificing some privacy for device surveillance, 75% agreed with "once the device has been approved, the FDA should continue to monitor for signs that there are problems with the device even if it means that private health information about me is collected". Respondents seemed to believe that the FDA was risk averse; 56% believed that the FDA does not approve devices unless they're a hundred percent safe. This is in contrast to trends shifting the demonstration of safety to post-approval settings and expanding acceptable forms of data for regulatory approval. Paul J. Wang: In a research letter, Laura Rottner, Christoph Sinning and associates examined novel high resolution imaging system based on a wide band dielectric technology, and reports the first clinical experience of feasibility and reliability of cryoballoon [CB] occlusion tool as compared to fluoroscopic and 3D transesophogeal [TEE] assessment during pulmonary vein isolation [PVI]. In consecutive patients with symptomatic atrial fibrillation [AF], cryoballoon-based ablation was performed with a novel 3D wide-band dielectric imaging system. Pulmonary vein [PV] occlusion was assessed with fluoroscopy in 3D-TEE and concomitantly correlated with the novel CB occlusion tool. The endpoint was defined as persistent PV isolation verified by spiral mapping catheter recordings 30 minutes after the last CB application. A total of 36 (90%) of PVs in 10 patients with paroxysmal (40%) and persistent (60%) were analyzed. In all patients, a normal PV anatomy with four separate PVs was documented. Visualization via 3D-TEE was feasible in 80% septal PVs and 100% of lateral PVs. In 67% of PVs, total PV occlusion was confirmed by all 3 imaging modalities. In 17% of PVs, incomplete PV occlusion was initially demonstrated by TEE and 3D dielectric imaging, whereas fluoroscopy suggested complete occlusion in initial analysis. After repositioning of the CB at 3 PVs, complete PV occlusion was verified by all three modalities. In 3 out of 36 (8%), no occlusion was initially seen by any imaging modality, for which the CB was repositioned resulting in total PV occlusion as confirmed by all three modalities. Two out of 36 PVs (6%) were confirmed to be occluded via fluoroscopy in 3D-TEE, but not by the CB occlusion tool. There was only one out of 36 PVs (3%), which were confirmed to be included by the CB tool and 3D-TEE, but not by fluoroscopy. A negative and positive predictive value of 1.0 and 0.6 was seen when comparing PV occlusion by the novel occlusion tool compared to PV collusion, verified by fluoroscopy and 3D-TEE. Paul J. Wang: In a special report, Jun Hirokami, and associates aim to clarify the spatial correlations between fractionated potential detected by Lumipoint with non-PV trigger. They enrolled 30 symptomatic atrial fibrillation [AF] patients who underwent non pulmonary vein [PV] foci ablation. 4 patients underwent the first procedure, 17 underwent second procedure and eight underwent third procedure, and one underwent a fourth procedure. They highlighted the fractionated signal area in atrial muscle [FAAM] during sinus rhythm and atrial pacing, thereby producing a digital FAAM map. They retrospectively applied Lumipoint to 30 patients in order to clarify the relationship between FAAM and non-pulmonary vein [PV] foci. Non-PV foci were successfully identified in all patients. They identified four patients with multiple non-PV foci. Of these four patients, one had non-PV foci at the superior vena cava and left arterial anterior wall. One had non-PV foci at the SVC and LA bottom wall. And two had non-PV foci at the SVC and interatrial septum. They only analyze 30 non-PV foci unrelated to SVC because the SVC isolation was routinely performed for non-PVC foci at the SVC. In order to analyze the correlation between FAAM and location of non-PV triggers, they determined the cutoff points of peaks slider, which non-PV triggers were completely located within the FAAM in. The accuracy of predicting location of the non-PV triggers was summarized using area under the receiver operating curve, a UROC curve. The optimal cutoff point of peak sliders to predict the location of non-PV was determined by the Youden Index. The Youden Index established the optimal cutoff point of the maximum peaks slider was 7; sensitivity was 0.906 and specificity 0.770. The peaks slider 7 was the most accurate predictor fractionated signals location area to the location of non-PV triggers. (area under the curve 0.902). The mean area of peaks slider 7 was six centimeters squared or 4.3% of the atrium. The authors concluded that the proof-of-concept observational study demonstrated that novel visualization tool of FAAM map successfully identified non-PV triggers that did not induce atrial fibrillation and/or non-PV foci, which potentially serve as substrates for AF maintenance. Paul J. Wang: In a special report, Leslie Saxon and associates update their prior publication providing further detail on mitigation adoption rates for the entirety of the U.S. patient population with implanted cardiac rhythm management devices falling under FDA cyber security advisories from any device manufacturer. They also provided limited data on known cybersecurity mitigation adoption outside the U.S. They report a unique complication resulting for introducing firmware to already implanted devices. Discuss how evolving FDA policies towards firmware mitigation adoption may increasingly determine how and when updates occur. They found that patients under 50 years of age and those over 80 years were less likely to receive the software upgrades, and male versus females had greater rates of upgrades. The upgrade rates varied according to U.S. Region and date of implant. Resynchronization devices were less likely to receive the upgrade, as were pacemaker dependent patient. Those ICD patients initially falling under the battery advisers were upgraded more frequently. The number of advisory patients followed in clinic was a significant predictor for firmware upgrade adoption, particularly for pacemakers that were often upgraded in smaller size clinics. Overall, only 24% of devices for all groups, and 22% of devices not impacted by the battery advisory were upgraded. For Abbott devices, the home communicator cyber security vulnerabilities were mitigated with an automatic software patch that was updated using the Merlin network, and adoption rates were nearly a hundred percent. For the entire patient cohort with impacted pacemaker and ICDs, U.S. and global adoption rates remain low at 24 to 35% with a low rate of complications. Most reported complications for pacemakers and ICD were symptoms (transient palpitations, dizziness, or syncope) that resulted from the temporary change in mode to VVI or transient loss of programmer telemetry while performing the upgrade (pacemaker 0.05%; ICD 0.01%). Globally, a total of 9 pacemakers and 8 ICDs required replacement, as a result of performing the firmware upgrade due to irreversible reversion to a backup pacing mode and loss of defibrillation therapy (ICDs). Analysis of the returned ICD pulse generaotrs found at 7 cases, the cause related to a capacitor bond failure that was exposed only when extended telemetry as required by the upgrade. The failure mechanism was an isolated component failure in the remaining ICD. The programmer based test has recently been FDA approved and can be performed prior to firmware upgrade to identify ICD patients at risk for capacitor bond failure. A total of 256 ICDs were susceptible to loss of RF telemetry after receiving a firmware update, and this has since been mitigated with a software patch. For Medtronic programmers, the initial mitigation responses of cybersecurity advisory was to take the programmers off the network. The network connection was enhanced with one or more security protections provided to the programmers using a flash drive, so the programmers can now be secured from potential cyber intrusion when connected to the network. Medtronic ICDs are currently being upgraded. The upgrade is being provided to impacted patients automatically when the device is interrogated with the programmer during follow-up. Metronic is introducing upgrades in phased approach with all expected to be completed by the beginning of 2021. There are 9% or 55,000 ICDs under this advisory that cannot receive the update due to design or safety constraints. Since the 2017 Abbott advisories identify cybersecurity vulnerabilities in pacemakers and ICDs with the potential for exploits have been increased, including 2 additional FDA advisories issued for another manufacturer. Medtronic's connected communication product and implantable defibrillators in the past 12 months. The authors comment that a recent report and a smaller number of Abbott impacted pacemaker and ICD patients from Canada reported marked differences in mitigation adoption rates between pacemakers and ICDs. This was due to an increase incremental clinical familiarity and comfort with performing the updates as experience and education surrounding these issues evolve. The authors indicate that automating cybersecurity updates without process in place for determining safety, for alerting patients or clinicians that have been delivered, may also be associated with yet unknown risks. Newer generation devices and communication protocols may render cyber security, advisories less frequent as cybersecurity integration is considered an essential aspect of device design. Paul J. Wang: In a review article, Albert Feeny and associates discuss the use of artificial intelligence [AI] and machine learning [ML] in medicine, which are currently areas of intense exploration showing potential to automate human tasks or even perform tasks beyond human capabilities. The first objective of this review is to provide the novice reader with a literacy of AI/ML methods, and to provide a foundation of how one may conduct an ML study. The review provides a technical overview of some of the most commonly used terms, challenges in AI/ML studies with reference to recent studies in cardiac electrophysiology to illustrate key points. The second objective of this review is to use examples from the recent literature to discuss how AI and ML are changing clinical practice and research in cardiac electrophysiology with emphasis on disease detection and diagnosis, prediction, and patient outcomes and novel characterization of disease. The final objective is to highlight important considerations and challenges for appropriate variation, adoption, and deployment of AI technologies and practice. Paul J. Wang: That's it for this month! We hope that you will find the journal to be the go-to place for everyone interested in the field! See you next time! This program is copyright American Heart Association 2020. Thank you.
durée : 00:00:43 - Good morning à teurtous
Episode 30- How fast can we give IV magnesium?
The rate of IV magnesium administration depends on the particular indication, dose, and patient-specific factors. Tune in for more details.References:Kaye P, O'Sullivan I. The role of magnesium in the emergency department. Emerg Med J. 2002; 19: 288-291Grissinger M. Avoiding patient harm from a magnesium bolus dose. P & T. 2014; 39(2): 81-82Preventing magnesium toxicity in obstetrics. ISMP. Updated October 5, 2005. Accessed November 2 2020. https://www.ismp.org/resources/preventing-magnesium-toxicity-obstetrics
The Curious Clinicians are back at it, exploring why magnesium so effectively treats the arrythmia torsades de pointes. Hint: it's the same mechanism as magnesium's effects on bronchospasm in severe asthma and seizures in eclampsia! As always, you can get CE/MOC credits just for listening! To learn more, check out the show notes for this episode on our website. You can also read Avi's original tweetorial on torsades and magnesium here.
Elektrolit Bozuklukları Elektrolit anormallikleri kardiyak arreste neden olabilir veya katkıda bulunabilir, resüsitatif çabaları engelleyebilir ve kardiyak arrest sonrası hemodinamik iyileşmeyi etkileyebilir. Standart İKYD'ye ek olarak, spesifik müdahaleler hiperkalemi ve hipermagnezemi vakaları için hayat kurtarıcı olabilir. Hiperkalemiye genellikle böbrek yetmezliği neden olur ve kardiyak aritmileri ve kardiyak arresti presipite edebilir. Şiddetli hipokalemi daha az yaygındır, ancak gastrointestinal veya renal kayıplar durumunda ortaya çıkabilir ve yaşamı tehdit eden ventriküler aritmilere yol açabilir. Şiddetli hipermagnezemi, en çok preeklampsi veya eklampsi için IV magnezyum tedavisi alan obstetrik hastalarda meydana gelir. Çok yüksek seviyelerde hipermagnezemi, bilinçte değişikliklere, bradikardiye veya ventriküler aritmilere ve kalp durmasına neden olabilir. Hipomagnezemi, diğer nedenlerin yanı sıra gastrointestinal hastalık veya yetersiz beslenme durumunda ortaya çıkabilir ve ciddi olduğunda hem atriyal hem de ventriküler aritmilere yol açabilir. Bu konu en son 2010'da resmi kanıt değerlendirmesi almıştır. Öneriler Bilinen veya şüphelenilen hiperkalemili kardiyak arrest için standart İKYD bakımına ek olarak IV kalsiyum uygulanmalıdır (c1 KD C-LD).Standart İKYD'ye ek olarak, yaşamı tehdit eden hiperkalemiyi tedavi etmek için uzun süredir birkaç tedavi önerilmektedir. Bunlar; IV kalsiyum ve/veya bikarbonat, glikoz artı insülin ve/veya inhale albuterol uygulamasını içerir. Parenteral kalsiyum, miyokardiyal hücre zarını stabilize edebilir ve bu nedenle, kardiyak arrest sırasında en faydalı olanıdır ve IV veya IO yoluyla verilebilir. Tipik doz, IV veya IO yol aracılığıyla 2 ila 5 dakikada uygulanan 5 ila 10 mL %10 kalsiyum klorür solüsyonu veya 15 ila 30 mL %10 kalsiyum glukonat solüsyonudur. Sodyum polistirenin (Kayexalate) standart kullanımı artık zayıf etkinlik ve bağırsak komplikasyonları riski nedeniyle önerilmemektedir. Hastane ortamında; acil hemodiyaliz, yaşamı tehdit eden hiperkalemi için kesin tedavi olmaya devam etmektedir.Şiddetli hipomagnezemiden kaynaklanan kardiyotoksisite ve kardiyak arrest için standart İKYD bakımına ek olarak IV magnezyum önerilir (c1 KD C-LD).Uzamış QT yokluğunda IV magnezyum uygulaması VF/VT için faydalı bulunmamasına rağmen, uzamış QT'si olan hastalarda kardiyak arest için kullanılması tavsiye edilir. Hipomagnezemi, uzamış QT'ye neden olabilir veya bunu şiddetlendirebilir. çoklu aritmiler ile ilişkilidir ve kardiyak arresti presipite edebilir. Bu yüzden, standart İKYD tedavinin temel taşı olmaya devam etmesine rağmen, normal seviyelerin sağlanması anlamlıdır. Torsades de Pointes tedavisi için öneriler Geniş Kompleks Taşikardi bölümünde verilmektedir.Bilinen veya şüphelenilen hipermagnezemili kalp durması için, standart İKYD bakımına ek olarak, ampirik IV kalsiyum uygulanması makul olabilir (c2b KD C-EO).Hiperkalemi için önerilen dozlarda IV veya IO kalsiyum uygulaması, şiddetli magnezyum toksisitesinde hemodinamiyi iyileştirebilir ve doğrudan kanıt olmamasına rağmen kardiyak arestte kullanımı desteklenebilir.Şüpheli hipokalemik kardiyak arrest vakalarında IV bolus potasyum uygulaması önerilmez (c3: Zarar KD C-LD).Şiddetli hipokalemiye bağlı ventriküler aritmiler için kontrollü IV potasyum uygulaması yararlı olabilir, ancak vaka raporları genellikle potasyum infüzyonunu içermiş ve bolus uygulamayı içermemiştir. Kardiyak cerrahinin en az bir küçük vaka serisinde, bir anestezi uzmanı tarafından yüksek donanımlı ortamda kardiyak yan etkiler olmaksızın bolus doz uygulaması bildirilmiştir. Ancak bu uygulamanın kardiyak arrest için etkinliği bilinmemektedir ve güvenlik endişeleri devam etmektedir. Opioid Doz Aşımı Opioide bağlı hastane dışı kardiyak arrest sıklığı giderek artmaktadır. Özellikle 25-65 yaş aralığında opioid kaynaklı ölümler sık görülmektedir. İzole opioid toksisitesi MSS ve solunum sisteminde depresyona yol açar. Bu durum solunum arrestine,
Elektrolit Bozuklukları Elektrolit anormallikleri kardiyak arreste neden olabilir veya katkıda bulunabilir, resüsitatif çabaları engelleyebilir ve kardiyak arrest sonrası hemodinamik iyileşmeyi etkileyebilir. Standart İKYD'ye ek olarak, spesifik müdahaleler hiperkalemi ve hipermagnezemi vakaları için hayat kurtarıcı olabilir. Hiperkalemiye genellikle böbrek yetmezliği neden olur ve kardiyak aritmileri ve kardiyak arresti presipite edebilir. Şiddetli hipokalemi daha az yaygındır, ancak gastrointestinal veya renal kayıplar durumunda ortaya çıkabilir ve yaşamı tehdit eden ventriküler aritmilere yol açabilir. Şiddetli hipermagnezemi, en çok preeklampsi veya eklampsi için IV magnezyum tedavisi alan obstetrik hastalarda meydana gelir. Çok yüksek seviyelerde hipermagnezemi, bilinçte değişikliklere, bradikardiye veya ventriküler aritmilere ve kalp durmasına neden olabilir. Hipomagnezemi, diğer nedenlerin yanı sıra gastrointestinal hastalık veya yetersiz beslenme durumunda ortaya çıkabilir ve ciddi olduğunda hem atriyal hem de ventriküler aritmilere yol açabilir. Bu konu en son 2010'da resmi kanıt değerlendirmesi almıştır. Öneriler Bilinen veya şüphelenilen hiperkalemili kardiyak arrest için standart İKYD bakımına ek olarak IV kalsiyum uygulanmalıdır (c1 KD C-LD).Standart İKYD'ye ek olarak, yaşamı tehdit eden hiperkalemiyi tedavi etmek için uzun süredir birkaç tedavi önerilmektedir. Bunlar; IV kalsiyum ve/veya bikarbonat, glikoz artı insülin ve/veya inhale albuterol uygulamasını içerir. Parenteral kalsiyum, miyokardiyal hücre zarını stabilize edebilir ve bu nedenle, kardiyak arrest sırasında en faydalı olanıdır ve IV veya IO yoluyla verilebilir. Tipik doz, IV veya IO yol aracılığıyla 2 ila 5 dakikada uygulanan 5 ila 10 mL %10 kalsiyum klorür solüsyonu veya 15 ila 30 mL %10 kalsiyum glukonat solüsyonudur. Sodyum polistirenin (Kayexalate) standart kullanımı artık zayıf etkinlik ve bağırsak komplikasyonları riski nedeniyle önerilmemektedir. Hastane ortamında; acil hemodiyaliz, yaşamı tehdit eden hiperkalemi için kesin tedavi olmaya devam etmektedir.Şiddetli hipomagnezemiden kaynaklanan kardiyotoksisite ve kardiyak arrest için standart İKYD bakımına ek olarak IV magnezyum önerilir (c1 KD C-LD).Uzamış QT yokluğunda IV magnezyum uygulaması VF/VT için faydalı bulunmamasına rağmen, uzamış QT'si olan hastalarda kardiyak arest için kullanılması tavsiye edilir. Hipomagnezemi, uzamış QT'ye neden olabilir veya bunu şiddetlendirebilir. çoklu aritmiler ile ilişkilidir ve kardiyak arresti presipite edebilir. Bu yüzden, standart İKYD tedavinin temel taşı olmaya devam etmesine rağmen, normal seviyelerin sağlanması anlamlıdır. Torsades de Pointes tedavisi için öneriler Geniş Kompleks Taşikardi bölümünde verilmektedir.Bilinen veya şüphelenilen hipermagnezemili kalp durması için, standart İKYD bakımına ek olarak, ampirik IV kalsiyum uygulanması makul olabilir (c2b KD C-EO).Hiperkalemi için önerilen dozlarda IV veya IO kalsiyum uygulaması, şiddetli magnezyum toksisitesinde hemodinamiyi iyileştirebilir ve doğrudan kanıt olmamasına rağmen kardiyak arestte kullanımı desteklenebilir.Şüpheli hipokalemik kardiyak arrest vakalarında IV bolus potasyum uygulaması önerilmez (c3: Zarar KD C-LD).Şiddetli hipokalemiye bağlı ventriküler aritmiler için kontrollü IV potasyum uygulaması yararlı olabilir, ancak vaka raporları genellikle potasyum infüzyonunu içermiş ve bolus uygulamayı içermemiştir. Kardiyak cerrahinin en az bir küçük vaka serisinde, bir anestezi uzmanı tarafından yüksek donanımlı ortamda kardiyak yan etkiler olmaksızın bolus doz uygulaması bildirilmiştir. Ancak bu uygulamanın kardiyak arrest için etkinliği bilinmemektedir ve güvenlik endişeleri devam etmektedir. Opioid Doz Aşımı Opioide bağlı hastane dışı kardiyak arrest sıklığı giderek artmaktadır. Özellikle 25-65 yaş aralığında opioid kaynaklı ölümler sık görülmektedir. İzole opioid toksisitesi MSS ve solunum sisteminde depresyona yol açar. Bu durum solunum arrestine,
Geniş Kompleks Taşikardi Geniş kompleks taşikardi, QRS süresi 0.12 saniye veya daha fazla olan hızlı bir ritim (genellikle bir aritmiye atfedilebildiğinde 150 atım / dakika veya daha fazla) olarak tanımlanır. Aberran iletili supraventriküler taşikardi, atriyoventriküler reentry'nin neden olduğu paroksismal SVT, aberran iletili atriyal fibrilasyon, atriyal flutter veya ektopik atriyal taşikardi dahil olmak üzere anormal şekilde geçirilen herhangi bir supraventriküler taşikardiyi temsil edebilir. Geniş kompleks taşikardinin ilk tedavisi, hastanın hemodinamik stabilitesinin hızlı bir şekilde değerlendirilmesini gerektirir. Stabil olmayan hastalar acil elektriksel kardiyoversiyon gerektirir. Hemodinamik stabil olan hastalara ise taşikardi özelliklerini değerlendirmek için 12 derivasyonlu bir EKG çekilmelidir. Hemodinamik olarak stabil ritimler değerlendirme ve farmakolojik tedavi için bir fırsat sağlarken, unstabil hastalarda ise acil kardiyoversiyon uygulanmalıdır. Düzenli geniş kompleks taşikardinin paroksismal SVT olduğundan şüpheleniliyorsa, farmakolojik tedavilere başlamadan önce vagal manevralar düşünülebilir. Geniş kompleks taşikardisi olan stabil hastalarda, özellikle VT olduğundan şüpheleniliyorsa veya adenozin başarısızlığı varsa IV antiaritmik ilaçlar düşünülebilir. Daha uzun etki süreleri nedeniyle, antiaritmik ajanlar, geniş kompleks taşikardinin nüksetmesini önlemek için de yararlı olabilir. Lidokain, farklılaşmamış geniş kompleks taşikardi için bir tedavi seçeneği olarak dahil edilmemiştir çünkü SVT için etkisiz olan nispeten dar spektrumlu bir ilaçtır. Amiodaron, prokainamid ve sotalol, lidokaine göre "daha geniş spektrumlu" antiaritmiklerdir ve hem SVT'yi hem de VT'yi tedavi edebilir, ancak hipotansiyona neden olabilirler. Verapamil, aupraventriküler kökenli olduğu ve aksesuar yol iletimini içermediği bilinen geniş kompleks bir taşikardinin tedavisinde etkili olsa da negatif inotropik ve hipotansif etkileri VT'yi dengesizleştirebilir ve önceden uyarılmış atriyal fibrilasyonu ve flutter'ı hızlandırabilir. Hemodinamik Olarak Stabil Geniş Kompleks Taşikardide Elektrikli Tedavi Yönetimi ÖnerisiHemodinamik olarak stabil geniş kompleks taşikardinin tedavisinde farmakolojik tedavi başarısız olursa, kardiyoversiyon veya acil uzman konsültasyonu istemek mantıklıdır (2a) Torsades de Pointes Polimorfik VT, QRS kompleksinin atımdan atıma farklı konfigürasyonları ile geniş kompleksli ventriküler kaynaklı taşikardiyi ifade eder Polimorfik VT'nin Elektriksel Tedavi ÖnerisiSürekli, hemodinamik olarak kararsız polimorfik VT için acil defibrilasyon önerilir (1) Altta yatan QT aralığı ne olursa olsun, tüm polimorfik VT formları hemodinamik ve elektriksel olarak unstabil olma eğilimindedir. Tekrarlayabilir, kendiliğinden hafifleyebilir, sürekli hale gelebilir veya elektriksel şok gerekebilecek VF'ye dönüşebilirler. Polimorfik VT, her QRS kompleksinin farklı özellikleri nedeniyle güvenilir bir şekilde senkronize edilemez ve yüksek enerjili senkronize edilmemiş defibrilasyon gerektirir. Uzun QT Aralığı (Torsades De Pointes) ile İlişkili Polimorfik VT'nin Farmakolojik Tedavisi ÖnerisiUzun bir QT aralığı (torsades de pointes) ile ilişkili polimorfik VT'nin tedavisi için magnezyum düşünülebilir (2b) Torsades, QT aralığını uzatabilen ve aritmiyi artırabilen antiaritmik ilaçlarla tedavi edilemez. Magnezyumun, torsades'te görülen VT salvolarını tetikleyebilen miyokardiyal aksiyon potansiyelindeki dalgalanmalar olan erken depolarizasyonları baskıladığına inanılıyor. Bunun yanında herhangi bir elektrolit anormalliğinin, özellikle hipokaleminin düzeltilmesi de tavsiye edilir. Uzun QT Aralığı ile İlişkili Olmayan Polimorfik VT'nin Farmakolojik Tedavisi İçin ÖnerilerIV lidokain, amiodaron ve miyokardiyal iskemiyi tedavi etmeye yönelik önlemler, uzun QT aralığı yokluğunda polimorfik VT'yi tedavi etmek için düşünülebilir (2b)Normal bir QT aralığı ile polimorfik VT tedavisinde rutin magnezyum ...
Contributor: Sam Killian, MD Educational Pearls: Droperidol (Inapsine) is an antipsychotic drug with efficacy for nausea, vomiting, headaches, and treating agitation In the early 2000’s, Droperidol received a black box warning for QT prolongation This caused a precipitous drop of in administration and ultimately led to a stop in production More careful analysis since has called into question the true incidence of QT prolongation in typical dosing Retrospective review published this year looked at 15,374 non-critical and 1,172 critical patients who received droperidol with only a single episode of Torsades des pointes (which was attributed to multiple other risk factors) Of the 2,431 non-critical patients, and 396 critical patients, who received an ECG before and after administration, there were no changes to the mean QTc Droperidol is being manufactured again and the prior black box warning being called into question, so it will likely begin to become more widely available for use References Cole JB, Lee SC, Martel ML, Smith SW, Biros MH, Miner JR. The Incidence of QT Prolongation and Torsades des Pointes in Patients Receiving Droperidol in an Urban Emergency Department. West J Emerg Med. 2020 Jul 2;21(4):728-736. doi: 10.5811/westjem.2020.4.47036. PMID: 32726229; PMCID: PMC7390553. Perkins J, Ho JD, Vilke GM, DeMers G. American Academy of Emergency Medicine Position Statement: Safety of Droperidol Use in the Emergency Department. J Emerg Med. 2015 Jul;49(1):91-7. doi: 10.1016/j.jemermed.2014.12.024. Epub 2015 Mar 30. PMID: 25837231. Summarized by Jackson Roos, MS4 | Edited by Erik Verzemnieks, MD
Mini episode 3- Early After Depolarizations and Experimental Mechanisms of Torsades
Great review of potential torsades mechanisms based off experimental data- https://www.sciencedirect.com/science/article/pii/S1880427611800050
Ventricular ArrhythmiasSpecial Guest: Matthew Wanat, PharmD, BCPS, BCCCP, FCCM Show Notes: https://pharmacytodose.files.wordpress.com/2020/07/ventricular-arrhythmias-show-notes.pdf Reference List: https://pharmacytodose.files.wordpress.com/2020/07/ventricular-arrhythmias-references.pdf 04:00 – What are arrhythmias?; 05:30 – Why are arrhythmias harmful/dangerous?; 06:58 – Risk factors; 09:12 – Common atrial arrhythmias; 10:19 – General arrhythmia treatment principles; 12:45 – When to use rhythm control for AF; 14:37 – Adenosine; 22:04 – Non-sustained VT/PVCs; 27:00 – Monomorphic v. Polymorphic VT; 30:53 – Torsades de Pointes; 34:16 – QTc prolongation; 42:18 – VF v. VT; 43:29 – Pulseless VT/VF; 49:30 – Amiodarone; 54:55 – Lidocaine/Mextiletine; 64:10 – Sotalol; 67:40 – Sodium channel blockers; 70:25 – Isoproterenol; 73:43 – BB/CCB; 78:29 – Long-term management; 80:34 – Stroke risk with ventricular arrhythmias; 82:20 – Prevention; 83:40 – EKG Interpretation; 86:48 – Step-wise approach; 88:13 – Take-home points; 90:00 – Small talk PharmacyToDose.Com@PharmacyToDose on Twitter/InstagramPharmacyToDose@Gmail.com
Cuisses de lapin à la bière brune et ses torsades à la farine d’épeautre
durée : 00:33:30 - On cuisine ensemble la marmite picarde FB Picardie - Le lapin une viande peu calorique qui se cuisine à toutes les sauces.
Torsades de Pointes
488: Evaluating the unknown QTc/torsades risk of hydroxychloroquine and azithromycin
The Elective Rotation: A Critical Care Hospital Pharmacy Podcast
Show notes at pharmacyjoe.com/episode488. In this episode, I ll discuss evaluating the unknown QTc/torsades risk of hydroxychloroquine and azithromycin. The post 488: Evaluating the unknown QTc/torsades risk of hydroxychloroquine and azithromycin appeared first on Pharmacy Joe.
On this episode Dave talks about how the QT interval is a big deal and how we should be looking at it each time we perform an ECG. QT Interval - The time from the beginning of the Q wave to the end of the T wave. Also In This Episode Please start looking at the QTc as part of your regular ECG interpretation Torsades de Pointes is a specific form of 'Polymorphic Ventricular Tachycardia' caused by a 'Long QT'. Watch out and prepare! QT little 'c' which stands for (corrected). What it is correcting for? It's correcting for 'RATE' and averaging everything to 60 beats per minute. QTc > 0.50 sec = a clinically significant prolonged QT interval and you need to tell somebody about it!! Patients at higher risk - Methadone and medications of the Mycin family are notorious for prolonging the QT interval to name just a very few. Brush up on all the other medications that prolong the QT. Take a closer look at the QTc in patients who are elderly and perhaps suffer from chronic renal insufficiency...they are higher risk patients for a prolonged QT. And don't forget...If you encounter a patient in Torsades. Once you fix the rhythm, immediately as yourself...Hmm why did this patient have a prolonged QT interval??? So it doesn't happen again. Subscribe to the video version of this podcast to have access to the visuals that accompany the audio as well as additional tools and resources to help improve your understanding. Subscribe now at CurrentECG.com And Stay Current!
Dr Carolyn Lam: Welcome to Circulation on the Run, your weekly podcast summary and backstage pass to the journal and its editors. I'm Dr Carolyn Lam, Associate Editor from the National Heart Center and Duke National University of Singapore. Dr Greg Hundley: And I'm Greg Hundley, Associate Editor of Circulation from the Pauley Heart Center at VCU Health in Richmond, Virginia. Dr Carolyn Lam: Are NOACs, or non-vitamin K antagonist oral anticoagulants, safe and efficacious in patients with extremely high or very low body weight? Very interesting paper and discussion coming right up. Greg, I hear that you've got a couple of papers you'd like to highlight first. Dr Greg Hundley: You bet, Carolyn. My two papers today both focus on ventricular dysrhythmia. The first one, from Yuki Komatsu from Tsukuba, Japan, researches the efficacy of catheter ablation of refractory ventricular fibrillation storm after myocardial infarction. VF storm attributed to focally triggered VF after MI is recognized as a distinctive, lethal, arrhythmogenic syndrome that differs from scar mediated monomorphic VT. This study investigated the acute and long-term outcomes of catheter ablation for the treatment of last resort in a large series of consecutive patients with post-MI VF storm refractory to medical therapies. In the study, investigators enrolled 110 patients averaging about sixty-five years in age. Ninety-two were men, and their average ejection fraction was approximately 31%. VF storm occurred in the acute phase of MI, about four and a half days after MI-onset, during the index hospitalization in about 39% of the patients. It was sub-acute (that is greater than 1 week later) in 44% of patients. It was remote (greater than 6 months later) in 17% of patients. And the focal triggers were found to originate from the scar border zone in 80% of the individuals. Dr Carolyn Lam: And what did the study show? Dr Greg Hundley: So Carolyn, during in hospital stay after ablation, VF storm subsided in 84% of patients and overall, 27% of in-hospital deaths occurred. The duration from the VF occurrence to the ablation procedure was associated with in-hospital mortality, with a P-value of 0.008. During follow-up after discharge from the hospital, only one patient developed recurrent VF storm. Of note though, 36% of the patients died, with a median survival of 2.2 years. And the long-term mortality was associated with a low EF (less than 30%), New York Heart Association class greater than 3 Heart Failure, a history of atrial fibrillation or chronic kidney disease. So in summary Carolyn, the results of this study show that in patients with MI presenting with focally-triggered VF storm, catheter ablation of the culprit triggers is life-saving and appears to be associated with short and long-term freedom from recurrent VF storm. The overall mortality for these patients is associated with the severity of their underlying cardiovascular disease, and those associated co-morbidities. Now my next paper is from one of our associate editors, Sami Viskin from Tel Aviv University. He's looking at a new form of polymorphic VT. Now as we think about polymorphic VT, I always think about the long QT interval syndromes associated with Torsades de Pointes. We have specific management strategies for those long QT syndromes, but Carolyn, there's a second category of polymorphic VT that's not related to QT prolongation. This second category involves patients without structural heart disease, who have genetic disorders like Brugada or patients that may have experienced hypothermia. There is also a third category of individuals with structural heart disease, during acute ST elevation MI. What Sami has discovered is there's now a fourth category of non-QT prolongation, which includes those with coronary artery disease but without evidence of ischemia. Dr Carolyn Lam: So how did they show or find this fourth category? Dr Greg Hundley: Well, this is a longitudinal cohort that he identified, and they basically followed forty-three individuals who developed polymorphic VT within days of an otherwise uncomplicated MI or coronary revascularization procedure. The in-hospital mortality was 17% with these patients with arrhythmic storm and the patients were treated with quinidine invariably survived to hospital discharge, just like the other categories of non-QT prolongation polymorphic VT. During long term follow-up of five and a half years, 16% of patients discharged without quinidine developed recurrent polymorphic VT and there were no recurrent arrhythmias in those individuals that were receiving quinidine therapy long term. So Carolyn, although quinidine therapy is usually considered contraindicated in patients with organic heart disease who develop ventricular arrhythmias, this therapy may be life-saving for patients with coronary disease developed arrhythmic storms due to polymorphic VT. Polymorphic VT storms may be a transient phenomenon. It's unclear for how long quinidine should be continued in these responsive patients. Dr Carolyn Lam: Wow, neat! Well, for my two papers I'm going to start off with a basic paper and, in fact, a quiz for you this time, Greg! So, what do cilia have to do with the heart? All right, you get to ask me, do you remember what cilia are? Dr Greg Hundley: Aren't cilia on prokaryotes? I mean, I think of bacteria. Dr Carolyn Lam: All right, let me set us straight. The primary cilium is a cellular organelle and it's formed by a protrusion of the plasma membrane that functions as a signaling platform in eukaryotic cells and is found in many cells including neurons, pre-adipocytes and kidney tubular cells, where they have been reported to be involved in a variety of cellular functions such as proliferation, differentiation, cell cycle regulation as well as mechano-chemical sensing of diverse stimuli. Now, the importance of these cilia is highlighted by the role in several diseases, known as ciliopathies. Polycystic kidney disease is one such disorder with, by the way, numerous cardiovascular manifestations. Whereas ciliated cells have been described in the developing heart, a role for primary cilia in the adult heart has not been reported. It was therefore the aim of these authors and those co-corresponding authors Dr Hill from UT Southwestern and Dr Lavandero from University of Chile, who aimed to identify cells in the adult heart harboring a primary cilium and to determine whether these primary cilia play a role in disease-related remodeling. Dr Greg Hundley: Carolyn, this is so interesting. I had no idea about these cilia. So what did they find? Dr Carolyn Lam: So, in a series of elegant experiments, these authors identified for the first-time primary cilia in mouse, rats, and human hearts, specifically and exclusively in cardiac fibroblasts. Now these ciliated fibroblasts were enriched in areas of myocardial injury. Transforming Growth Factor beta-1 signaling and SMAD3 activation were impaired in fibroblasts that were depleted of the primary cilium. Extra cellular matrix protein levels and contractile function were also impaired. And in vivo depletion of PC1 inactivated fibroblasts after myocardial infarction impaired the remodeling response. Dr Greg Hundley: So how do we use this clinically, and what does it mean for us? Dr Carolyn Lam: These findings point to a pivotal role of cilia and PC1 in disease related pathological cardiac remodeling and suggest that some cardiovascular manifestations of autosomal dominant polycystic kidney disease, for example, derive directly from myocardium autonomous abnormalities. The findings also uncover novel fibrosis regulators and raise the prospect that this pathway may emerge as a target with therapeutic relevance. Dr Greg Hundley: Wow, very interesting! Dr Carolyn Lam: Thanks! And the next paper is also very interesting, in dilated cardiomyopathy and providing insights in how specific viral function may be involved in the development of dilated cardiomyopathy. Looking at the Group B enteroviruses, which are a common cause of acute myocarditis and can be a precursor of chronic myocarditis and therefore dilated cardiomyopathy leading to heart transplantation. In fact, enterovirus-induced dilated cardiomyopathy represents a third of idiopathic dilated cardiomyopathy cases. So these authors, led by corresponding author Dr Andreoletti from University of Reims, Champagne-Ardenne and Dr Semler from University of California, performed deep sequencing of viral RNA from cardiac tissue from patients with enterovirus related end stage dilated cardiomyopathy and then trans-factored viral RNA clones, mimicking the viral genomes found in patient tissues into primary human cardiac cells to assess their replication activities and impact on cardiomyocyte function. They found that the major persistent viral forms are composed of B-type enteroviruses harboring 5' terminal deletion in their genomic RNAs. These viruses alone, or associated with full length populations of helper RNAs, could impair cardiomyocyte function by viral enterovirus proteinase 2A activities in these enterovirus-related dilated cardiomyopathy cases. Dr Greg Hundley: Very interesting, Carolyn. So what are the clinical implications of this viral infection of the heart? Dr Carolyn Lam: Well, the findings seem to imply that it would be important for us to develop specific inhibitors of enterovirus proteinase 2A activity that might prevent viral replication and inhibit the shut-off of host cell translation as well as the disruption of dystrophin. Furthermore, in early diagnosed enterovirus induced dilated cardiomyopathy, the use of such protease inhibitors could potentially decrease and stop the chronic pathological process of dilated cardiomyopathy and therefore reduce the need for heart transplantation in this end-stage. Very interesting, but requires more work. So, that wraps up our summaries Greg. Shall we move to our feature discussion? Dr Greg Hundley: Absolutely. Dr Greg Hundley: Today we have Renato Lopes from Duke University in Durham, North Carolina and Brian Olshansky, Professor Emeritus from Iowa now in clinical practice in Waterloo and Mason City, Iowa. We're going to talk about our non-vitamin K oral antagonists, or NOACs, safe and efficacious in patients in extremely high (greater than 120 kg) or extremely low (less than 60kg) of body weight. Renato, welcome to our podcast in Circulation on the Run. Can you give us a little overview of your study, why you performed it and what results did you experience? Dr Renato Lopes: The idea behind this study was to provide more data into the use of NOACs in these extreme body weight patients, where we don't have a lot of information. Some guidelines actually caution against the use of NOACs in patients with extreme body weight because of the lack of data. We had the opportunity to look at the Aristotle database, which was a large, randomized trial comparing apixaban versus warfarin for patients with atrial fibrillation, over 18 000 patients. We took advantage of this database to try to look at the extreme body weight and how those patients at weight more than 120 kg, more than 140 kg and less than 60 kg, performed in terms of the treatment effect of apixaban versus warfarin. This was the rational, to try to provide more data so people could gain additional confidence in using apixaban in clinical practice in those extreme body weight patients. What we showed was, in general the treatment effect of apixaban versus warfarin for the efficacy outcomes CHOKE, systemic embolism and all cause death and myocardial infarction was very consistent across the weight spectrum and preserved. Apixaban was superior to warfarin and this was consistent regardless of the weight category. For the low body weight patients less than 60 kg, we also found that apixaban results in terms if efficacy was preserved. So, going out to the bleeding and safety endpoints, apixaban was safer than warfarin across different spectrums of weight. Surprisingly, in patients less than 60 kg we saw an even greater relative risk reduction in bleeding, in patients treated with apixaban compared to warfarin. The main message was for efficacy, apixaban was better than warfarin - the same results as the Aristotle main trial. For bleeding and safety endpoints, we also saw the same results and consistent results with apixaban- in particular with patients below 60 kg, which is always a concern that people might have in clinical practice. It seems that apixaban was even safer with an even greater treatment effect. Dr Greg Hundley: Very nice. Can you tell us a little bit about some of the sites where you enrolled patients and did you identify any variation in age, sex or region specific factors? Were there any differences in your findings related to race? Dr Renato Lopes: That is a very interesting question because we know that these variables play an important role in body weight. We enrolled patients from thirty-nine countries in Aristotle, in over a thousand sites all over the world. Interestingly, I can tell you that the heaviest weight we had in our study was 205 kg, a patient from the United States. The lightest weight that we had was 39 kg, from the Philippines. You lose trading the variation that regions of the world can play out and how patients can perform. We haven't seen any major difference in these analogies. There were prior analogies that look at different BMIs, and we know that the treatment effect might be attenuated depending on race and sex. In this analogy, we did not find any significant difference according to race, region of the world or even sex. Dr Greg Hundley: Just getting back to your body weight measurement, you mentioned percentage of individuals were above 120 kg and briefly mentioned some were above 140 kg. What percentage of your study cohort was that extra-large size, above 140 kg? Do you think more work needs to be done in that area or do you think the results were sufficient for that very heavy body weight? Dr Renato Lopes: This is a very important question. If we look at the breakdown, we had about 11% of the entire trial in the low spectrum of weight, less than 60 kg in weight - almost 2000 patients. A good number of patients. In extreme weight more than 120, we have about 980 patients. That was 5.5% of the overall trial. When you look at greater than 140 kg, we had 258 patients, 1.4% of the overall trial population and about 25% of this category greater than 120. I think as we start getting greater than 140 kg, we had 258 patients. It is not a large number of patients. It is some information and it is good to have some data on these patients. Before that, we had no data on apixaban in this level of weight. What we are seeing is that above 140 kg, the death rate are very low. There is a trend to better bleeding endpoints and better bleeding profile with apixaban, similar to what we have seen in the entire spectrum of weight when we look at weight as a continuous variable. We also saw that trend in patients greater than 140 kg for bleeding. This is reassuring. I don't think we can say it is definitive, it is only 260 patients that we are talking about. It is reassuring that we now have data in patients more than 140 and up to 205 kg, and we didn't seem to see any major concern or any difference in the curves in terms of the direction of efficacy and safety of apixaban. For the majority of patients it is reassuring and gives us extra confidence that the dose we use in clinical practice five milligrams twice daily should also work in those heavy weight and the heaviest body weight patients. Dr Greg Hundley: Very good. Brian you've done an excellent editorial and I wonder if you could help us put this study in perspective with what we know about NOACs and managing patients with atrial fibrillation? Dr Brian Olshansky: It really is a fascinating study. Obesity is as growing problem for us here in the mid-west and probably throughout the world. It effects a variety of things including drug pharmakinetics, volume of distribution, drug clearance etc. So knowing how NOACs work at the extremes of body weight, either the massively obese or the vanishingly frail, it becomes important to understand the safety and efficacy of the use of NOACs in these individuals. There are guidelines that caution us against use of NOACs at extremes of body weight, particularly those patients who are over the 120 kg mark. The one point I would like to make is, at least here in the mid-west, 120 kg is becoming almost the norm. We are having people that are becomingly massively obese and this is really the question then in my mind, is what to do with those patients who are over 140 kg or even way more than that. This gets to points that I would like to make about some the issues we need to consider about this study and where we are with our understanding about the use of NOACs in the extremes of body weight. One thing to keep in mind is, in this analysis, this was a retrospective group analysis. That is one important point. We don't have prospective data that look at an entire large population, a very frail, a very low body weight population. Another issue is that weight is not a static measure. We only have assessment at the baseline. Variability in weight or body mass index may be important in terms of its relationship to the development of atrial fibrillation and sequelae. The other issue here to consider is that there are comorbidities that are associated with those who are at the extremes of body weight and there was a significant variation in this study in age composition, sex dominance, the region of enrollment, the presence of comorbidities between the different weight groups that could contribute to results we have seen. Those with low body weight had more comorbidities and a higher mean CHADSVASC score, and had the biggest difference between apixaban and warfarin. We have quite a bit to learn about how to understand these data, and when we consider the individuals who are over 140 kg, indeed there are concerns about the volume of distribution of a NOAC and its efficacy. We would like to rely on this data. The problem is that the number of individuals that are a part of this retrospective analysis at the very high body weight and very low body weights was a rather small number and so to project from that number, what we should do with all of our patients becomes somewhat of a concern. Although these are interesting and provocative data, what we really need is to have some well-designed large prospective randomized controlled trials that specifically address those individuals at the extremes of body weight because this is becoming more and more of a problem as time goes on. We are seeing more individuals that are at the extremes of body weight. While I have not specifically noticed a difference in my own clinical practice, what we need is a better understanding about the dosing of and potential risks and benefits of the NOACs for the extremes of body weight. Dr Greg Hundley: On behalf of Carolyn and myself, we really appreciate you listening. Have a great week. We look forward to seeing you next week. Dr Carolyn Lam This program is Copyright American Heart Association 2019.
Episode 9 - Torsades de SAAG
Explore low SAAG (not portal HTN) ascites with Alex, HIV asscociated cardiomyopathy with Rob, and Torsades with Chi!This podcast is powered by Pinecast.
IBCC Episode 12 - Torsades De Pointes
Do those squiggly lines on the ECG monitor have you patient down in the hypotensive dumps? Don't know what to do? Well we have you covered. Identification, common causes and treatment of TDP can all be found in this one podcast.
“Unstable” Arrhythmias Arrhythmias that cause Hypotension Pulmonary Edema Chest Pain Altered Mental Status Supraventricular Tachycardia (SVT) Stable Vagal maneuver Adenosine Beta blocker or calcium channel blocker Unstable SYNCHRONIZED cardioversion Monomorphic Ventricular Tachycardia (VT) Stable Amiodarone Procainamide Lidocaine Unstable SYNCHRONIZED cardioversion Pulseless Defibrillation Polymorphic Ventricular Tachycardia (aka Torsades de Pointes) Known complication of prolonged QTc Side […]
Dr. Dimitre is back with the 57th episode of the primary medicine podcast! Acquired long QTc syndrome is a disorder of the rhythm of the heart. It can lead to ventricular arrhythmias, such as Torsades de Pointe, and possibly ventricular fibrillation and death. It is caused by QTc prolonging medications which include antidepressants, antibiotics, antibiotics, […] The post Podcast 57: Acquired Long QTc Syndrome appeared first on Primary Medicine Podcast.
Circulation: Arrhythmia and Electrophysiology On the Beat August 2017
Dr. Wang: Welcome to the monthly podcast On The Beat for Circulation, Arrhythmia and Electrophysiology. I'm Dr. Paul Wang, editor-in-chief, with some of the key highlights from this month's issue. We'll also hear from Dr. Suraj Kapa, reporting on new research from the latest journal articles in the field. This month's issue of Circulation: Arrhythmia and Electrophysiology has a number of fascinating and important articles. Let's start with the first article by Philip Halbfass and Associates, which describes the use of esophageal endoscopy in patients undergoing atrial fibrillation ablation. Of 1,802 patients undergoing afib ablation, 832 underwent post-procedural esophageal endoscopy. All patients were ablated using a single tip re-circular ablation catheter. Category one lesions described as erythema erosion were seen in 98 out of these 295 patients, while in 52 out of the 295 patients, ulceration was seen. In three of the 832 patients, esophageal perforation occurred, and in two of the 832 patients, atrial-esophageal fistula occurred. Esophageal perforation only occurred in patients with category two lesions with an absolute risk of 9.6%. The authors concluded that post-ablation esophageal endoscopy is able to identify patients with high-risk lesions. One out of 10 patients with post-ablation esophageal ulcers progressed to perforation, while no patients without esophageal ulcers showed evidence of perforating complications. In the next article by Christian Sohns and Associates describes the relationship between atrial fibrosis identified with magnetic resonance imaging and atrial rotor activity identified by noninvasive electrophysiological mapping. Ten patients underwent pulmonary vein isolation for persistent atrial fibrillation. Late gadolinium enhancement using magnetic resonance imaging, which projected onto the anatomy used for noninvasive electrophysiologic mapping. The noninvasive electrophysiologic mapping identified 410 rotors evenly distributed between the left atrium and the right atrium. This study found that there was no statistically significant association between the presence of late gadolinium enhancement and the presence of rotors. In the next article written by Jereon Venlet examines the endocardial unipolar voltage that best identifies abnormal epicardial electrograms. Thirty-three patients underwent endocardial epicardial right ventricular electro-anatomical mapping in ablation of right ventricular scar-related ventricular tachycardia. Eighty-six percent of abnormal epicardial electrograms had corresponding endocardial sites with bipolar electrogram less than 1.5 millivolts. The remaining abnormal epicardial electrograms could be identified by endocardial unipolar voltages of less than 3.7 millivolts. The authors concluded that this use of endocardial unipolar voltage cut off at normal bipolar voltage sites improves the identification of all abnormal epicardial electrograms where there is less than 1 millimeter of fat. The next article by Alan Bulava and Associates examines the outcomes of hybrid epicardial and endocardial radial frequency ablation, a persistent atrial fibrillation. Seventy patients underwent the epicardial thoracoscopic procedure followed by endocardial mapping ablation two to three months later. At the time of catheter ablation, 76% of patients were in sinus rhythm. All four pulmonary veins were found to be isolated in 69% of the patients and the left atrial posterior wall was isolated in 23% of the patients. In the 12 months after the catheter ablation, 77% were arrhythmia-free, off antirrhythmic drugs. The majority of arrhythmia occurrences occur during the first 12 months following catheter ablation. Using previously ineffective antiarrythmics drugs and re-ablation procedures, arrhythmia-free survival increased to 97% during a mean followup of 936 days. Left atrial volume greater than 165 milliliters, the absence of sinus rhythm before catheter ablation and induce-ability of any sustained tachyarrhythmia at the end of catheter ablation predicted atrial fibrillation recurrence. The authors concluded that the majority of patients after epicardial ablation required endocardial catheter ablation to complete the linear ablation or pulmonary vein isolation lesion sets. In the next article, Jason Roberts and Associates studied the clinical phenotype of Type 6 Long QT Syndrome, stemming from mutations in the KCNE2 encoded voltage gated channel beta subunit. The authors examined individuals reported pathogenic KCNE2 mutations collected from inherited arrhythmia clinics in the Rochester LQTS registry as well as previously reported LQT6 cases identified through a med-line database search. Of 44 probands studied, 16 probands had resting QTC intervals and only developed QT prolongation and malignant arrhythmias following exposure to QT prolonging stressors. Ten had other Long QT pathogenic mutations and 10 did not have a Long QT phenotype, with the remaining eight subjects having a Long QT phenotype, but with evidence suggesting that the KCNE2 variant was not the underlying culprit. The authors noted that the collective frequency of KCNE2 variance implicated in Long QT6 syndrome in the exome aggregation consortium database was 1.4%, in comparison with the 0.0005% estimated clinical prevalence of LQT6 syndrome. Thus, the authors concluded that based on clinical phenotype, the high allelic frequencies of LQT6 mutations in the exome consortium database, in absence of prior documentation of genotype phenotype segregation, many KCNE2 variants, and perhaps all have been erroneously designated as long QT syndrome causative mutations. Instead, KCNE2 variants may confer pro-arrhythmic susceptibility when provoked by additional environmental acquired or genetic factors. In the next article, Alexander Quinn and Associates examine how mechanically-induced ectopy may cause ventricular fibrillation, the mechanism of commotio cordis. It is known that the block of stretched sensitive ATP inactivated potassium channels limits ventricular fibrillation occurrence in a porcine model of commotio cordis. In isolated rabbit heart preparations using optical voltage mapping combined with pharmacological block of potassium ATP or stretch activated cation nonselective channels, the authors showed that the mechanical stimulation reliably triggers premature ventricular excitation at the contact site with induce-ability predicted by local tissue indentation. Mechanically-induced premature ventricular excitation induction is decreased by stretch activated cation nonselective channel block. The authors also found that mechanically-induced premature ventricular excitation resulted in ventricular fibrillation only if the mechanical stimulation site overlaps the re-polarization wave edge in hearts where T-waves involve a well-defined re-polarization edge traversing the epicardium. This defines a narrow subject-specific vulnerable window for commotio cordis-induced ventricular fibrillation in both time and space. In the next article Matthias Seidl and Associates examine the gene expression required for development of atrial fibrillation in a transgenic mouse model. Recent studies showed that atrial fibrillation susceptibility is associated with down regularization of target genes of the CREB/CREM family of transcription factors. CREB/CREM refers to cyclic and P-response element binding protein modulator. Short CREM repressor isoforms like CREM-IbΔC-X bind to cyclical A&P responsive elements preventing transcriptional activation. Messenger RNA for CREM-IbΔC-X is up-regulated in atrial biopsies from patients with paroxysmal or chronic atrial fibrillation. The authors examined transgenic mice expressing CREM-IbΔC-X, which spontaneously developed atrial fibrillation proceeding to permanent fibrillation with age. The authors found that the most prominent alterations of the gene program linked to CREM-induced atria modeling were identified in expression of genes related to structure, metabolism, contractility and electrical activity regulation. In the next article by Takumi Yamada and Associates electrophysiologic characteristics of the idiopathic ventricular arrhythmias originating from the parietal band, one of the muscle bands of the right ventricle, were examined. Of 294 consecutive patients with right ventricular origins, 14 patients had ventricular arrhythmia origins in the parietal band. All patients have left bundle block pattern with 12 inferior and two superior axis. All patients had the notch in the middle of the curess in all cases. Seven patients had precordial transition before lead V3 and four patients had a slow curess onset. Far field ventricular electrogram with an early activation was always recorded in His bundle region regardless of the location of the ventricular arrhythmia origin. During the catheter ablation, a mean number of 10.4 radio frequency of applications with a mean duration of 1,099 seconds were delivered. Catheter ablation was successful in 10 patients and ventricular arrhythmias recurred in four with a mean followup of 41 months. In the Advances in Arrhythmia and Electrophysiology section, the Buza and Associates have reviewed cancer treatment-induced arrhythmias. The authors describe ECD advances in arrhythmias associated with individual cancer chemotherapeutic agents. Now here with a review of the highlights from the articles from journals throughout the world in the past month, is Dr. Suraj Kapa. Dr. Kapa: Hello. Today we're going to be going over several hard hitting articles we have identified that seem to stand out in the electrophysiological literature from the month of July 2017. The first area we will be delving into is that of atrial fibrillation. Specifically related to cardiac mapping and ablation. The first article in this area that we've chosen was published by Samuel et al. in the Journal of Cardiovascular Electrophysiology entitled Catheter Ablation for the Treatment of Atrial Fibrillation Is Associated with a Reduction in Healthcare Resource Utilization. Samuel et al. reviewed data from a large population base cohort in Quebec, Canada including over 1,500 patients undergoing cardiac ablation for atrial fibrillation. They demonstrated that healthcare resource utilization including hospitalizations, emergency room visits and cardioversions were significantly reduced both 12 months as well as 24 months after the next ablation. These findings seem to suggest that catheter ablation has a sustained overall impact on resource utilization amongst patients with atrial fibrillation. While the study was not randomized and was a retrospective evaluation of outcomes, these findings are provocative. Certainly as we wait for the results of the Cabana trial in about one year we hope to see whether or not cardiac ablation carries the weight of potential beneficial impacts both in terms of long-term care as well as long-term outcomes. Of course being a retrospective evaluation, one question that lies with regards to these findings is whether or not the reduction in resource utilization might be a byproduct of improved ambulatory care of these patients or whether it's a byproduct of patients understanding their disease process better, and thus perhaps not seeking emergency room care or hospitalization as frequently. The next publication we'll focus on was published by Anselmino et al. in The International Journal of Cardiology entitled Conduction Recovery Following Catheter Ablation in Patients with Recurrent Atrial Fibrillation and Heart Failure. This publication synergizes with several other publications that have come out in the month of July. Focusing on the publication by Anselmino et al., they reviewed retrospectively patients undergoing redo atrial fibrillation ablation in the setting of underlying heart failure. What they demonstrated was that nearly a third of patients had no pulmonary vein reconnection, but tended to have more persistent forms of atrial fibrillation suggesting more extensive atrial substraights. This study is complimentary to a publication by [inaudible 00:15:23] et al., published in JACC EP. this past month where they evaluated the longterm outcomes of patients who, when presenting for redo atrial fibrillation ablation had persistent pulmonary vein isolation. In that article, they found that nearly 17% of patients presenting for redo ablation had persistent pulmonary vein isolation. Moreover, these patients tended to perform significantly worse in terms of longterm outcomes than those who presented with PV reconnection, with about a 56% freedom from affiliate swipe after we do ablation in the setting of persistent pulmonary vein isolation as opposed to 76% when there was PV reconnection seen. So the question becomes if we see this greater atrial substraight, should we automatically be doing more ablation? Of course as we all know, there have been many studies performed trying to tease out whether additional ablation in patients who might have more significant atrial substraight carries benefits. In this regard, Fink et al. in last month's edition of Circulation, Arrhythmia and Electrophysiology demonstrated that in fact as an index procedure of performing a stepwise concomitant café plus linear ablation on top of pulmonary vein isolation in persistent and long standing persistent atrial fibrillation patients did not necessarily confer an increased likelihood of longterm success over pulmonary vein isolation alone. Thus, the jury continues to still be out as far as what the right strategy is in many of these patients. However, these studies highlight the importance of continued evaluation and understanding of how we can use information about atrial substraight to guide our ablation procedures more successfully. Changing gears, we'll move on the pathophysiology mechanisms of disease within atrial fibrillation. The article we will choose to focus on here was published by Die et al. in The Journal of Cardiovascular Electrophysiology entitled The Effects of Extrinsic Cardiac Nerve Stimulation on Atrial Fibrillation Induce-ability: The Regulatory Role of the Spinal Cord. Over the course of the last several years many investigators have sought to show that modulation of the autonomic nervous system can successfully alter cardiac electrophysiology and provide antiarrythmic benefits. However, when subject to prospective trials such as the recently published Defeat HF Trial, they have not necessarily found clear benefit. Thus, a critical question becomes how we translate our animal models into human treatment. The interesting results from Die et al. lie in the fact that they looked at the effects of spinal cord stimulation and spinal cord block in addition to concomitant stimulation of other centers such as the venous nerve, the stellate ganglion and ganglionated plexi. They demonstrated that spinal cord stimulation enhanced the effects of venial nerve stimulation while attenuating the effects of stimulating the left stellate ganglion or ganglionated plexus. In turn, the combinations of these different levels of stimulation had different effects on affiliate swipe induce-ability, whether significantly increasing or decreasing the potential. The reason this article is important is it highlights the extensive cross linking and synergy that exists within the autonomic nervous system and that attention paid to only a single center of autonomic innovation may not be sufficient for certain paradigms of care. This past month there were also two reviews summarizing the role of the autonomic nervous system and modulation of that nervous system and the treatment of arrhythmias. The first was by Witt et al. and Europace. The other by Schwartz et al. in the International Journal of Cardiology. These articles help the reader understand the extensive crosslinking and cross communication that might occur, that might sometimes defeat our efforts to use a single element of the autonomic nervous system to modulate cardiac arrhythmias. Changing gears yet again, we'll move on to risk stratification and management for atrial fibrillation. Perino et al. in last month's edition of The Journal of the American College of Cardiology published an article entitled Treating Specialty in Outcomes in Newly Diagnosed Atrial Fibrillation from the Treat AF Study. They present data based on a very large cohort of over 180,000 veterans regarding the effect of treating specialty on atrial fibrillation outcome. Interestingly they demonstrated that when a cardiologist was involved in the care of the patient, there was an overall decrease in stroke and mortality. Albeit with a concomitant increase in hospitalization for AF. The stroke reduction seen was also seen to be secondary to better anticoagulation prescription within 90 days of diagnosis when those patients were seen by a cardiologist as compared with a general internist. This earlier prescription anticoagulation however did not mediate the mortality reduction. These data presented by a Perino et al. are provocative in this era of rising healthcare costs. The question is, as atrial fibrillation rates rise, as the general population ages, how quickly and how aggressively we should engage specialty care early on in patient evaluation. The data by Perino et al. suggests that maybe this engagement should occur earlier. Part of the reasons for this might be improved understanding of current evidence regarding treatment of such patients or better systems of care that allow for providers to identify patients who might need alterations and care faster. However, if anything this is hypothesis-generating. Why anticoagulation prescriptions are delayed when patients are not seen by a specialist or why there would be a difference in mortality are important factors to review further. In this past month Hernandez et al. in Stroke published an article discussing the large degree of geographic variation that exists with regards to appropriate anticoagulation prescription in patients with atrial fibrillation. They demonstrated that there's extensive inhomogeneity across the United States in terms of how and in whom anticoagulation gets prescribed. Thus, how much of these outcomes are specialist-driven, geographically-driven or based on elements of access to care or other issues are going to be important features that have to be evaluated. The next article in risk stratification was published by Mostofsky et al. in Heart, entitle Chocolate Intake and Risk of Clinically Apparent Atrial Fibrillation: The Danish Diet, Cancer and Heart Study. In this study they demonstrated in a population of over 55,000 patients that when accounting for as many variables as they could, higher chocolate intake, more than once per month, was associated with a decreased atrial fibrillation risk when compared with those consuming less chocolate than once per month. Of course, they note that despite these attempts to account for multiple confounding variables, residuary confounders cannot be accounted for. The relevance of this article lies in the question of lifestyle choices patients are asked to make when thinking about how to either prevent themselves from having atrial fibrillation or trying to even treat their atrial fibrillation risk. Chocolate has been shown to have multiple potential beneficial effects in multiple areas of cardiology, however, how to counsel patients with data like these becomes very difficult. The questions lies in how chocolate might mediate arrhythmia risk and how it might also modulate other potential risks such as weight gain or other factors. Thus while important to consider this in light of patients often asking what they can and cannot have, it is important to further consider that we don't understand the full story. The other key element to understand is that really when they say that chocolate intake reduces risk of clinically apparent atrial fibrillation they are speaking about moderate chocolate intake and not necessarily having it for three meals a day. Changing gears away from atrial fibrillation, we will next focus on the area of ICDs pacemakers and CRT. Aberi et al. in Nature's Scientific Reports published regarding inductively power wireless pacing via miniature pacemaker and remote stimulation control system. Their approach provides potential novel opportunities beyond currently available both lead-based and leadless pacemakers and improving battery and allowing for further miniaturization of such devices. They noted by creating a very novel inductive power supply they're able to miniaturize the pacing components and also significantly reduce the power requirements. In fact, they suggested that they could create a leadless device that could be as small as being delivered out of the anterior ventricular vein. This is the first report of such an inductively powered miniaturized pacing system with low enough power consumption that may prove viable for ambulatory human use. The desire to create improved pacing and fibrillation systems is further highlighted by an article published by [Kalu 00:25:41] et al. in JACC Clinical Electrophysiology this past month where they demonstrated initial results of percutaneous epicardially delivered partially insulated defibrillator lead. Work like these holds the potential to improve options for patients and in traditional vascular access is not desired, or an identifying new ways of delivering pacing therapy that exists outside the traditional lead base or even somewhat miniaturized leadless approaches. We'll next focus on the area of sudden death and cardiac arrest. The first article we'll focus on was published by Stecker et al. in The Journal of The American Heart Association entitled Health Insurance Expansion and Incidence of Out of Hospital Cardiac Arrest: A Pilot Study in the US Metropolitan Community. This article looked at the results of The Affordable Care Act, mainly health insurance expansion, on the rate of out of hospital cardiac arrest in a large US metropolitan community of over 600,000 people. They separately studied a middle aged population that might have been affected by healthcare expansion versus an older population, above 65, who would have had relatively stable insurance plans having been covered by Medicare both prior to and after this change in healthcare plans. They demonstrated that there was a significant decrease in overall out of hospital cardiac arrests amongst middle age people without any significant change amongst the more elderly Medicare population in the same time period. The time period studied was relatively short, nearly less than a decade. Of course, whether there were other events that might have occurred to alter this risk such as improvements in care beyond the combination of availability and mandates plus carrying health insurance, it remains to be seen. However, the data is very suggestive. Further evaluation at the national level in varying communities however would be useful, as well as consideration of population level cost benefit analysis. The next article published by Shen et al. in the New England Journal of Medicine entitled Declining Risk of Sudden Death in Heart Failure. They presented data across 40,000 patients from multiple clinical trials over two decades regarding the changing rates of sudden death amongst heart failure patients. Interestingly they noted there was an overall 44% reduction in sudden death rates across these trials over time dating from the 1990s to 2014. In the earliest trials considered, the mortality rate within 90 days after randomization was as high as 2.4% while the most recent trials suggest that that rate is more like 1.0%. This profound decline was attributed to improved usage and prescription of medications early on in the heart failure course, which may modulate outcomes. The relevance of these findings lies in trials that have been published recently and met analysis that we've discussed regarding utility of defibrillators in nonischemic cardiomyopathy or even ischemic cardiomyopathy. The recently published Danish study suggested that ICDs might not confer an equivalent mortality risk as what would have been expected years ago. However, this publication by Shen et al. is particularly provocative because it calls into question whether the same mortality benefit we anticipated from earlier heart failure trials should still be the rubric by which current defibrillator trials are powered. Namely, if we consider that Danish saw the 25% difference in mortality, with a 44% overall reduction in sudden death seen in trials over time for heart failure, seeking a 25% reduction might be excessive. Thus, this highlights the need to potentially power trials for ICDs and the benefit of such ICDs better. This importance of better stratifying better heart failure patients for sudden death risk has been raised in multiple articles this month, including in a review by Holiday et al. in Circulation and in the series of reviews published in Volume 237 of The International Journal of Cardiology. The last article we choose to focus on in the role of sudden death and cardiac arrest was published by Vehmeijer in Circulation: Arrhythmia and Electrophysiology entitled Prevention of Sudden Cardiac Death in Adults with Congenital Heart Disease: Do the Guidelines Fall Short? They reviewed outcomes amongst 26,000 adults with congenital heart disease in light of existing guidelines for risk prediction and prevention of sudden death. They demonstrated that less than half of the patients with sudden cardiac death actually had a guideline basis recommendation for an ICD on the basis of either the 2014 consensus statement on arrhythmias or the 2015 European Society of Cardiology Guidelines. These findings are very provocative in suggesting that we don't really understand who requires treatment amongst adults with congenital heart disease. With improved care paradigms, both with improvements in surgical outcomes as well as ambulatory care of these patients and recognition of need for interventions, arrhythmias are becoming a greater and greater problem amongst patients with adult congenital heart disease. However, large scale studies are limited in stratifying overall risk of arrhythmias. The risk is certainly present as many of these patients have ventricular scar often attributable to cardiac surgeries or have hemodynamic insults that may result in progressive fibrosis of the ventricles. In addition, the basal abnormalities of cardiac formation itself may lend itself to a sudden increased risk of arrhythmias. Thus, the question remains as how to best risk stratify these patients in order to reduce these overall sudden death rates. Changing gears yet again, we'll focus on two articles within the realm of cellular electrophysiology. The first article was published by Cerrone et al. in Nature Communications entitled Plakophilin-2 is Required for Transcription of Genes that Control Calcium Cycling and Cardiac Rhythm. They demonstrated that plakophilin-2, or PKP2, which is known to mediate arrhythmogenic right ventricular cardiomyopathy due to abnormalities in the desmosomes actually has other direct electrical effects independent of substraight effects that are seen. Specifically PKP2 plays a significant role in maintaining gene transcription for several genes that mediate normal electrophysiologic activity, such as the ryanodine receptor, calsequestrin and others. They demonstrated that this reduced expression of other genes secondary to PKP2 absence or abnormality leads to increased isoproterenol or adrenaline-induced arrhythmias that in turn can be suppressed with Flecainide. These findings are provocative in the fact that they suggest that it is possible for patients to have abnormalities of genes such as PKP2 that result in electrical abnormalities independent of the structural abnormalities. Furthermore, it suggests that manifestation of the disease such as catecholaminergic polymorphic ventricular tachycardia may be immediate upstream of typical channels associated with the disease. For example, if PKP2 reduces expression of the ryanodine receptor, this might result in manifestations similar to CPTB in some patients. Along the same lines, Hewitt et al. published in Science Advances regarding deregulated calcium cycling underlies the development of arrhythmia and heart disease due to mutant obscurin. Obscurins are a relatively growing area of interest as these are cytoskeletal proteins that have be associated with both hypertrophic and dilated cardiomyopathy. Similar to the story we just told about PKP2 however, they demonstrated that obscurins, likely through circa 2 and pentameric phospholamban can cause abnormal calcium handling. In fact, they demonstrated that the principle phenotype associated with obscurin abnormalities is one of an electrical abnormality, namely frequent PVCs. In turn, mechanical phenotypes such as cardiomyopathy result in the setting of chronic pathologic stress such as increased afterload, thus these findings demonstrate that genes such as obscurin or PKP2, which are commonly associated with structural or mechanical myopathic processes might have direct independent electrical effects. The story with obscurin raises further question into how this may apply to conditions of PVC-related cardiomyopathy or other such conditions. The other key point about these two areas of interest lie in the fact that it is possible as these genetic abnormalities mediate not just direct substraight elements, but arrhythmogenesis via abnormal channel expression, whether in all patients presenting with such specific genetic abnormalities substraight-based ablation alone will result in reduction of arrhythmia tendency. Of course this remains to be seen and is primarily hypothesis-generating. Next we'll focus on three articles within the area of genetic channelopathies. The first paper was published by Rohatgi et al. in The Journal of the American College of Cardiology entitled Contemporary Outcomes in Patients With Long QT Syndrome. In a large single center practice, they reviewed the results of over 600 patients predominantly affected by LQT1 or LQT2 and demonstrated that after initial evaluation along with treatment based on the individual, done at a highly skilled center, 92% of patients did not experience any breakthrough cardiac events over longterm followup. It was noted however, that the incidence of breakthrough cardiovascular events over longterm followup were far more common in patients who were symptomatic prior to their first evaluation than asymptomatic. In other words, if you were symptomatic prior to your first evaluation, the likelihood of a breakthrough cardiovascular event over longterm followup was as high as 25%, but if you were asymptomatic it was as low as 2%. These data suggest that our overall care of the Long QT patient is improving. However, it also supports that further improvements in care are needed as breakthrough cardiovascular events can continue to occur. It also highlights the importance of close followup of that symptomatic patient in the modern era. The second article was published by Kannenkeril et al. in JAMA Cardiology entitled the Efficacy of Flecainide in the Treatment of Catecholaminergic Polymorphic Ventricular Tachycardia. Flecainide currently carries a class 2A indication according to both the 2015 ENC guidelines and 2013 HRS AHRA APHRS consensus statement for treatment of patients with CPVT who fail max dose beta blockers. A lot of this evaluation however, has been based on retrospective evaluations. Kannenkeril reviewed in a prospective single blind placebo controlled crossover trial the effect of Flecainide on exercise associated arrhythmias in CPTV patients who were already on max tolerated beta blockers and had an ICD. Amongst the 14 patients included of whom 13 completed the study, they showed there was a significant reduction in median ventricular arrhythmia score during exercise and in fact there was complete suppression with Flecainide compared to the placebo of 85%. These findings thus add to the existing literature in terms the potential incremental value of Flecainide in achieving adequate arrhythmia suppression when used in conjunction with maximal tolerated beta blockers. The last article within the realm of genetic channelopathies we'll focus on was published by Yang et al. in The Journal of Physiology entitled A Multi-Scale Computational Modeling Approach Predicts Mechanisms of Female Sex Risk in the Setting of Arousal-Induced Arrhythmias. It is recognized that female gender can increase the risk of Torsades in the setting of both inherited and acquired prolonged QT syndromes. In a combination of experimental and computational approaches, Yang et al. demonstrated that hormone concentrations can partly mediate this risk, specifically as it relates to her-related mutations. They demonstrated testosterone and high progesterone levels provide a protective effect against Torsades. However, estrogen can enhance Torsadogenic potential, particularly in the setting sympathetic stress. They also demonstrated the mechanism by which this likely occurs is due to interaction of estrogen with pore loop or intracavity binding site of the her channel. In fact, on top of this they demonstrated that combined treatment with both estrogen and Dofetilide can simultaneously blockade the pore channel of her. These findings are provocative and hypothesis-generating. In terms of potential future research to further clarify risk for patients, particularly as it may apply to menstruating females who might have varying levels of estrogen, especially when being treated with concomitant QT prolonging agents such as Defetilide. Next we will focus on three articles within the realm of ventricular arrhythmias. The first article was published by Sapp et al. in JACC Clinical Electrophysiology entitled Real Time Localization of Ventricular Tachycardia Origin from the Twelve Lead Electrocardiogram. They presented a methodology for rapidly determining in real time the approximate origin of a ventricular tachycardia using the 12 lead during cardiac ablation. In 38 patients they used a variety of methods that involved multiple linear regression learning methods and demonstrated that a patient-specific regression method using at least 10 training set pacing sites in the individual patient can provide a localization accuracy of the exit site for VT of as much as five millimeters. Furthermore, with additional pacing sites that accuracy could improve further. These findings support the continued utility of the standard 12 lead ECG in localizing the exit site of ventricular tachycardia. Furthermore, it points out the importance of considering that the electrocardiogram can be patient-specific. By using multiple pacing sites, this helps an algorithm learn how a patient-specific heart exists in terms of its electrical propagation potential. Further informing based on a 12 lead of a specific VT approximately where it should be exiting from. The next article we will focus on was published by Muser et al. in again, JACC Clinical Electrophysiology entitled Longterm Outcomes of Catheter Ablation of Electrical Storm in Nonischemic Dilated Cardiomyopathy COMpared with Ischemic Cardiomyopathy. The summary point to this article is in a single center, large volume group of patients including about 267 total, the longterm outcomes of VT recurrence or mortality was no different between nonischemic and ischemic patients. This is important to note as most prospective studies and in fact retrospective studies of the role of ventricular tachycardia ablation have focused on ischemic patients where the substraight is relatively predicable. These findings highlight that ablation may provide a reasonably effective therapy irrespective of the cause of the myopathy. Finally, changing gears within the realm of ventricular arrhythmias, we'll focus on a translational article by Motloch et al. in JACC Basic to Translational Science entitled Increased Afterload Following Myocardial Infarction Promotes Conduction-Dependent Arrhythmias That Are Unmasked by Hypokalemia. They studied the role of increased afterload after myocardial infarction in a listing arrhythmias in a porcine infarct model. They demonstrated that in the setting of increased afterload there was increased widespread interstitial fibrosis. Interestingly, pacing -induced arrhythmias induced by a rapid burst pacing were mediated by hypokalemia associated conduction abnormalities rather than repolarization abnormalities. The reason these findings are potentially important lie in the fact that arrhythmias in the early stages after myocardial infarction, especially in a setting of increased afterload, might be considered to be secondary to either repolarization abnormalities or depolarization abnormalities. These findings suggest that in the setting of concomitant hypertension the primary problem really lies in hypokalemia associated conduction abnormalities. Thus, treatments that impair cardiac excitability, for example, even sodium channel blockade, may similarly confer an increased risk of ventricular arrhythmias when in the presence of increased afterload and myocardial infarction. It also calls into question whether interventions such as antitachycardia pacing in patients with hypertension, in other words increased afterload, might be more prone to acceleration of the ventricular arrhythmias than patients who are relatively better managed as far as afterload. Changing gears yet again, we will focus on EP relevant myopathies. [inaudible 00:44:19] et al. published in JACC Clinical Electrophysiology regarding use of the 12 lead electrocardiogram to localize regions of abnormal electron atomic substraight in arrhythmogenic ventricular cardiomyopathy. There were really two major articles in this regard that have been published both in the same month. The other article was published by Andrews et al. in Circulation, Arrhythmia and Electrophysiology entitled Electrical and Structural Substraight of Arrhythmogenic Right Ventricular Cardiomyopathy Determined Using Noninvasive Electrocardiographic Imaging and Late Gadolinium Magnetic Resonance Imaging. The relevance of both of these articles lies in their statements about the potential utility of noninvasive approaches essentially using electrocardiograms to determine the distribution of substraight in arrhythmogenic right ventricular cardiomyopathy. The article by [inaudible 00:45:16] et al. specifically focused on fractionation of the QRS. They showed that patients with evidence of fractionation in the QRS on a 12 lead ECG had more extensive substraight. Furthermore, distribution of fractionation to specific leads such as inferior, anterior or basal superior leads, was 100% specific, but veritably sensitive for identifying substraight as it localizes to specific cardiac regions. In turn, the publication by Andrews et al. in Circulation, Arrhythmia and Electrophysiology reviewed how the addition of multiple leads by a noninvasive electrocardiographic imaging could be used to even more specifically hone in on the relevant substraights. Their further benefit was in the suggestion that repolarization abnormalities in fact co-localized with origination sites for ventricular ectopy in these patients. In combination, these sites highlight the utility of simple, noninvasive methods of electrocardiographic imaging in identifying and defining the arrhythmogenic substraight in the NRVC. The next article we will review was by Sommariva et al. in Nature's Scientific Reports published just this past month entitled MIR 320A as a Potential Novel Circulating Biomarker of Arrhythmogenic Cardiomyopathy. They did micro RNA analysis on 53 healthy controls, 21 idiopathic VT patients and 36 arrhythmogenic cardiomyopathy patients and demonstrated that the circulating micro RNA 320A was significantly higher in arrhythmogenic cardiomyopathy than in either other cohorts. It is recognized that some patients with idiopathic VT, especially right ventricular [inaudible 00:47:09] VT might reflect a cohort that might have what we call "concealed ARVC." The question thus becomes how to define why a patient has a specific manifestation of disease because longterm outcomes, if there is some underlying ARVC might be worse if the ARVC is not recognized and if cure is assumed based on treatment of the initial presenting rhythm. Thus identifying novel ways of defining the presence of a disease even in the absence of obvious structural abnormalities carries benefit in terms of suggestions on longterm followup. Complimentary to the previously discussed article on the role of PKP2 mutations on mediating electrical instability in the heart, the study by [inaudible 00:48:01] et al. does in fact suggest that there might be methods of distinguishing arrhythmogenic cardiomyopathy from whether it be controls or truly idiopathic ventricular tachycardia using a very specific circulating biomarker. On a completely different route, we'll finish our podcast today with a discussion of Bruner et al. published in European Heart Journal entitled Alcohol Consumption, Sinus Tachycardia and Cardiac Arrhythmias at the Munich Oktoberfest: Results from the Munich Beer-Related Electrocardiogram Workup Study or Munich Brew. Bruner et al. studied over 3,000 voluntary participants with a combination of breath alcohol concentration measurements and electrocardiographic recordings via smartphone throughout the Munich Oktoberfest. In addition, they sought to evaluate chronic alcohol consumption effects on arrhythmias in a separate cord of over 4,000 patients from the Cora S4 study. In the study regarding acute alcohol effects, they demonstrated that in line with increasing BAC, there was a greater occurrence of arrhythmias in particular sinus tachycardia in almost a third of patients. What was even further interesting was that respiratory sinus arrhythmia over the course of higher BAC is from baseline was reduced in the setting of alcohol use. Similarly, with chronic alcohol consumption there was an apparent significant association with the occurrence of sinus tachycardia. The reason these findings are important is in their suggestive element that the effects of alcohol intake in terms of whether it be acute or chronic arrhythmogenesis might somewhat lie in their effects on the basal autonomic states. As demonstrated by the reduction in overall sinus arrhythmia. These findings serve to further elucidate mechanisms by which alcohol may mediate arrhythmias in a large real world patient sample. Thank you for joining us on this edition of On The Beat. Tune in next month again for more articles that might be of interest to the general electrophysiologic community all summarized in a single location.
Author: Aaron Lessen M.D. Educational Pearls: Imodium (loperamide) is a mu-opioid receptor agonist. Traditionally, it is used as an anti-diarrheal. It is also abused recreationally for an opioid high and to self-treat opioid withdrawal. 40 or more pills are often ingested. People often co-ingest with cimetidine to potentiate the desired effects. Patients will present with opioid overdose symptoms (narrow pupils, respiratory depression). Narcan is effective in reversing an overdose of Imodium. Imodium prolongs QT and predisposes to Torsades, so monitor rhythm and then treat like any other opioid OD. References: http://www.tandfonline.com/doi/abs/10.3109/15563650.2016.1159310
PVCs, Tach, Torsades and more. The post S2 E023 Ventricular Rhythms appeared first on Physician Assistant Exam Review.
This week, we review a simplified approach to determining the rhythm on an EKG with a tachydysrhythmia. https://media.blubrry.com/coreem/content.blubrry.com/coreem/Podcast_Episode_88_0_Final_Cut.m4a Download One Comment Tags: Atrial Fibrillation, AVNRT, SVT, Tachycardias, Tachydysrhythias, Ventricular Tachycardia Show Notes Take Home Points When looking at a tachy rhythm that isn't sinus tach, quickly differentiate by determining if the QRS complexes is narrow or wide and then determine if the rhythm is regular or irregular. This approach quickly drops the rhythm into 1 of 4 boxes and makes rhythm determination much easier Each of those 4 categories has a small set of rhythms included. Narrow and irregular – AF, Aflutter with variable block or MFAT. Narrow and regular – SVT or Aflutter. Wide and irregular – Torsades, VF, AF with aberrancy or a BBB. Wide and regular – VTach, SVT with aberrancy or SVT with a BBB. If you see wide and regular, the top 3 diagnoses are VT, VT and VT. Assuming VT and treating for that will almost never send you astray Read More EM: RAP: Episode 84 – Tachycardia Core EM:
This week, we review a simplified approach to determining the rhythm on an EKG with a tachydysrhythmia. https://media.blubrry.com/coreem/content.blubrry.com/coreem/Podcast_Episode_88_0_Final_Cut.m4a Download One Comment Tags: Atrial Fibrillation, AVNRT, SVT, Tachycardias, Tachydysrhythias, Ventricular Tachycardia Show Notes Take Home Points When looking at a tachy rhythm that isn’t sinus tach, quickly differentiate by determining if the QRS complexes is narrow or wide and then determine if the rhythm is regular or irregular. This approach quickly drops the rhythm into 1 of 4 boxes and makes rhythm determination much easier Each of those 4 categories has a small set of rhythms included. Narrow and irregular – AF, Aflutter with variable block or MFAT. Narrow and regular – SVT or Aflutter. Wide and irregular – Torsades, VF, AF with aberrancy or a BBB. Wide and regular – VTach, SVT with aberrancy or SVT with a BBB. If you see wide and regular, the top 3 diagnoses are VT, VT and VT. Assuming VT and treating for that will almost never send you astray Read More EM: RAP: Episode 84 – Tachycardia Core EM: A Si...
Episode 66: The latest on drug-induced torsades.
Episode 66: The latest on drug-induced torsades.
Best Case Ever 26: Chloral Hydrate Poisoning and Cardiac Arrest
I met up with Mike Betzner at North York General's Update in EM Conference in Toronto. He is the medical director of Air Transport STARS air ambulance out of Calgary and an amazing speaker on the national lecturing circuit. His Best Case Ever on Chloral Hydrate poisoning & cardiac arrest describes a young man in cardiac arrest with resistant Ventricular Fibrillation and Torsades de Pointes. There is only one class of drugs that can get him back into normal sinus rhythm. Dr. Betzner describes how he recognized that this patient was suffering from Chloral Hydrate poisoning and how he saved his life with one simple intervention. The post Best Case Ever 26: Chloral Hydrate Poisoning and Cardiac Arrest appeared first on Emergency Medicine Cases.
Best Case Ever 26: Chloral Hydrate Poisoning and Cardiac Arrest
I met up with Mike Betzner at North York General's Update in EM Conference in Toronto. He is the medical director of Air Transport STARS air ambulance out of Calgary and an amazing speaker on the national lecturing circuit. His Best Case Ever on Chloral Hydrate poisoning & cardiac arrest describes a young man in cardiac arrest with resistant Ventricular Fibrillation and Torsades de Pointes. There is only one class of drugs that can get him back into normal sinus rhythm. Dr. Betzner describes how he recognized that this patient was suffering from Chloral Hydrate poisoning and how he saved his life with one simple intervention. The post Best Case Ever 26: Chloral Hydrate Poisoning and Cardiac Arrest appeared first on Emergency Medicine Cases.













































