Podcasts about urinary
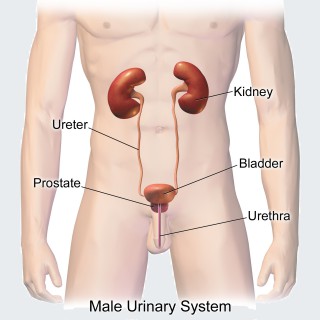
Human anatomical system consisting of the kidneys, ureters, urinary bladder, and the urethra
- 589PODCASTS
- 821EPISODES
- 30mAVG DURATION
- 1WEEKLY EPISODE
- Feb 19, 2026LATEST
POPULARITY
Best podcasts about urinary
Latest news about urinary
- Kirin and Immunosens Launch Joint Development of a Self-Testing Service That Uses Urinary IgA to Visualize a Person’s Immune Status ANTARA News - Latest Indonesia News - Feb 12, 2026
- Doctors discover surprising cause of life-threatening UTIs that plague millions every year Daily Mail - Feb 10, 2026
- Routine medical procedures can feel harder for women – here’s why The Conversation – Articles (UK) - Jan 30, 2026
- Self‐Assembled Hydrophobic Confinement Coupled with Calcium Coordination Enables Selective and Label‐Free SERS Detection of Urinary Biomarkers in Complex Samples Wiley: Advanced Functional Materials: Table of Contents - Jan 20, 2026
- Ultrasensitive Fluorescent Detection of Urinary Trypsin for Early Pancreatic Disease Diagnosis: Toward Smartphone‐Assisted Analysis Wiley: Chemistry – An Asian Journal: Table of Contents - Jan 14, 2026
- Nature’s Pharmacy: 4 Powerful herbs for urinary health NaturalNews.com - Dec 14, 2025
- I treat menopause and its symptoms, and hormone replacement therapy can help – here’s the science behind the FDA’s decision to remove warnings English – The Conversation - Nov 18, 2025
- A Chemical Glycoproteomic Approach Decrypts Urinary Extracellular Vesicle Surfaceome for Prostate Cancer Diagnosis and Grading Wiley: Angewandte Chemie International Edition: Table of Contents - Nov 11, 2025
- Urinary Albumin-Creatinine Ratio Better Measures Risk for Kidney Failure Drugs.com - News for Health Professionals - Nov 6, 2025
- At-Home Urine Analysis Systems - The Withings U-Scan Nutrio Tracks Four Urinary Biomarkers (TrendHunter.com) TrendHunter.com - Technology Trends and Gadgets - Oct 30, 2025
Latest podcast episodes about urinary
The EV-303 trial that led to the FDA approval of perioperative enfortumab vedotin + pembrolizumab in cisplatin-ineligible bladder cancer patients in now published in NEJM. We discuss the results and ponder potential future changes to treating bladder cancer in the future. Urinary diversion surgeries: https://jamanetwork.com/journals/jamaoncology/fullarticle/2842595
Join the Buff Muff Community and stop letting your bladder run your life! https://get.buffmuff.com/methodSupport your pelvic and whole body health with Rejeuve https://rejeuve.com/Rejuve is a line of pelvic health and whole body health supporting supplements that are helping women have a daily poogasm, eliminate leaks and prolapse symptoms, and keep their vulvovaginal tissues supple and resilient. Get your Rejeuve Supplements https://rejeuve.com/ and use code Podcast to save 10% off your first order.Thank you so much for listening! I use fitness and movement to help women prevent and overcome pelvic floor challenges like incontinence and organ prolapse. There is help for women in all life stages! Every Woman Needs A Vagina Coach! Please make sure to LEAVE A REVIEW and SUBSCRIBE to the show for the best fitness and wellness advice south of your belly button. *******************I recommend checking out my comprehensive pelvic health education and fitness programs on my Buff Muff AppYou can also join my next 28 Day Buff Muff Challenge https://www.vaginacoach.com/buffmuffIf you are feeling social you can connect with me… On Facebook https://www.facebook.com/VagCoachOn Instagram https://www.instagram.com/vaginacoach/On Twitter https://twitter.com/VaginaCoachOn The Web www.vaginacoach.comGet your Feel Amazing Vaginal Moisturizer Here
UTIs in Dementia: What Looks Different and What to Do
Urinary tract infections are one of the most common reasons people with dementia end up in the emergency room. In this video, I talk with Dr. Krieger, an emergency room physician, about why UTIs often look different in dementia and why sudden changes should not automatically be blamed on dementia progression. Dr. Krieger is also the creator of Uraguard, a product designed to help reduce bacterial exposure around the urethra for women with incontinence. We talk about where tools like this may fit into UTI prevention, along with other practical strategies caregivers can use. Learn more about Uraguard here: https://tinyurl.com/uraguard-careblazers-yt
The first women's public toilets in London opened on Bedford St on 11th February, 1852 - attempting to capitalize on the success of George Jennings' ‘monkey closets', used by over 800,000 visitors to the 1851 Great Exhibition. Unfortunately, even though the facility had been fought for by campaigning women's sanitary organizations, middle and upper class Victorian ladies were not yet prepared to pee in public - and the toilets closed a year later. In this episode, Arion, Rebecca and Olly explain where the phrase ‘spending a penny' (probably) comes from; reveal why ‘the urinary leash' came to describe the predicament of women's lives; and investigate why the number of 21st century public toilets continues to fall… Further Reading: • ‘Pamphlets of the Ladies Sanitary Association' (Wellcome Collection): https://wellcomecollection.org/works?query=%22Ladies+Sanitary+Association.%22 • ‘London's long-term lav affair: A history of public toilets in the capital' (BBC News, 2022): https://www.bbc.co.uk/news/uk-england-london-59785477 • ‘Victorian realities - how did they use the toilet??!' (Prior Attire, 2016): https://www.youtube.com/watch?v=NUHeSTDv_24 Love the show? Support us! Join
Ep. 87: Liquid Gold Standard: Urinary Sampling & Case Management for House Call Vets; Meet Dr. Surell Levine of Calm Cozy Cat!
Dr. Surell Levine graduated from Brown University with a Bachelor of Arts in 2001 and earned her Doctor of Veterinary Medicine from the University of Pennsylvania School of Veterinary Medicine in 2009. Following graduation, she completed a fellowship in Emergency and Critical Care and worked in the Emergency Room and Intensive Care Unit at Massachusetts Veterinary Referral Hospital. She is a certified veterinary medical acupuncturist and an active volunteer with the MSPCA animal shelter. She is also the inventor of the widely used Calm & Cozy Cat Wrap, a patented swaddle designed to make veterinary visits less stressful for cats. Topics covered in this episode: Preview of Dr. Surell's conference lecture on urinary sample collection and case management in house call practice Different styles of house call medicine, showing there's no single "right" way to practice Common urinary issues seen in home visits, including UTIs, cystitis Practical urine collection strategies in the home Using ultrasound as a quick in-home screening tool for urinary red flags Real-world urinalysis interpretation Balancing gold-standard preventive care with client budgets and real-life practice challenges Links & Resources: Calm & Cozy Cat Wrap: https://calmcozycat.com/ Hopkinton Home Vet https://www.hopkintonhomevet.com/ The House Call Vet Academy Resources: Download Dr. Eve's FREE House Call & Mobile Vet Biz Plan Find out about the House Call Vet Academy online CE course Learn more about the Concierge Vet Mastermind Get your FREE Concierge Vet Starter Kit mini course Learn more about Dr. Eve Harrison Learn more about 1-to-1 coaching for current & prospective house call & mobile vets Learn more about the House Call & Mobile Vet Virtual Conference → Register TODAY for the House Call & Mobile Vet Virtual Conference, February 7th-8th, 2026!!!!!! Music: In loving memory of Dr. Steve Weinberg. Intro and outro guitar music was written, performed, and recorded by house call veterinarian Dr. Steve Weinberg. This podcast is also available in video on our House Call Vet Cafe YouTube channel P.S. Here's a special gift from me as a huge thank you for being a part of our wonderful House Call Vet Cafe podcast community! ☕️ GET 20% OFF your Four Sigmatic Mushroom Coffee when you order through this link! 4Sig truly is my favorite!!! Enjoy it in good health, my friends!
Episode 655: Ep 655 The Science behind Urinary & Bladder Support
Forever Young Radio Show with America's Natural Doctor Podcast
Millions of Americans are frustrated with their urinary problems. More specifically, the need to urinate multiple times a day and night and leaking urine is frustrating to many people over the age of 45. Fortunately, there have been successful advances in the herbal treatment of common urinary problems. We are excited to share these breakthroughs on the show today. Tracey Seipel, ND, is CEO and founder of Australian-based Seipel Group. Dr. Seipel is a renowned naturopathic doctor, medical herbalist, and clinical nutritionist. Dr. Seipel is also a diabetes educator, researcher, and an award-winning natural products formulator with 35 years of experience in clinical practice.She pioneered the natural urological health category receiving a Nutrition Business Journal award in 2006 for innovation. During the 1990s, Seipel was a leader in establishing standards of education for Australian naturopathic colleges and as an advisor to government boards, including developing nutritional training for Australia Medical Schools. During her research as a product formulator for nutraceutical companies, she uncovered the significant prevalence and underreporting of urinary incontinence in women and then overactive bladder and incontinence in both men and women. Together, this led to her pioneering this natural health category. Understanding the significant health impacts and seeing no other companies willing to take on the challenge of improving bladder control, Seipel developed the initial formulation.Learn more about UROXUROX StudyLearn more about Emerald Labs Bladder Health which contains the branded ingredient UROX. Listeners can save 20% OFF at Emeraldlabs.com when using the code: Forever
EP79: 糖尿病與女性骨盆健康:常見泌尿症狀、鑑別診斷與治療關鍵 Ft. 婦產科謝筱芸醫師 Diabetes and Female Pelvic Health: Urinary Symptoms, Differential Diagnosis, and Clinical Considerations Ft. Dr. Hsieh HY (OBGYN)
本集特別邀請到 台中榮民總醫院 婦產科暨婦女泌尿專科醫師——謝筱芸醫師,一起深入探討糖尿病對女性骨盆健康的影響。許多糖尿病女性常出現頻尿、急尿、漏尿或反覆泌尿道感染,這些症狀究竟是來自血糖控制不良、神經病變,還是骨盆底功能障礙?本集從臨床實務出發,說明常見泌尿症狀的鑑別診斷重點,並分享婦女泌尿科醫師如何與骨盆復健、內科新陳代謝科及家醫科跨團隊合作,協助病患在藥物治療與生活調整之間取得平衡。節目也特別談到:雖然部分排糖藥物可能增加泌尿道感染風險,但血糖控制不良對泌尿與骨盆健康的影響更為關鍵。如何在診斷、治療與提升病患遵醫囑性之間取得臨床平衡,是照顧糖尿病女性不可忽視的一環。
Chegou o episódio escolhido por vocês! Marcela Belleza e Joanne Alves convidam Carol Millon para conversar sobe 6 clinicagens de inibidores de SGLT2, as gliflozinas:Indicações além do DMRisco de CAD euglicêmicaQuando não usar?Cuidados com doença aguda (sick day) e hipovolemiaCuidados pré-operatórioRisco de fratura e amputaçãoReferências:1. Bailey CJ, et al. Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med. 2013;11:43. Published 2013 Feb 20. doi:10.1186/1741-7015-11-432. Bersoff-Matcha SJ, et al. Fournier Gangrene Associated With Sodium-Glucose Cotransporter-2 Inhibitors: A Review of Spontaneous Postmarketing Cases. Ann Intern Med. 2019;170(11):764-769. doi:10.7326/M19-00853. Chang HY, et al. Association Between Sodium-Glucose Cotransporter 2 Inhibitors and Lower Extremity Amputation Among Patients With Type 2 Diabetes. JAMA Intern Med. 2018;178(9):1190-1198. doi:10.1001/jamainternmed.2018.3034 4. Clar C, et al. Systematic review of SGLT2 receptor inhibitors in dual or triple therapy in type 2 diabetes. BMJ Open. 2012 Oct 18;2(5):e001007. doi: 10.1136/bmjopen-2012-001007. PMID: 23087012; PMCID: PMC3488745.5. Das SR, et al. 2020 Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2020 Sep 1;76(9):1117-1145. doi: 10.1016/j.jacc.2020.05.037. Epub 2020 Aug 5. PMID: 32771263; PMCID: PMC7545583. 6. Fralick M, et al. Risk of amputation with canagliflozin across categories of age and cardiovascular risk in three US nationwide databases: cohort study. BMJ. 2020;370:m2812. Published 2020 Aug 25. doi:10.1136/bmj.m28127. Li D, et al. Urinary tract and genital infections in patients with type 2 diabetes treated with sodium-glucose co-transporter 2 inhibitors: A meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2017;19(3):348-355. doi:10.1111/dom.128258. Neal B, et al. Rationale, design, and baseline characteristics of the Canagliflozin Cardiovascular Assessment Study (CANVAS)--a randomized placebo-controlled trial. Am Heart J. 2013;166(2):217-223.e11. doi:10.1016/j.ahj.2013.05.0079. Nyirjesy P, et al. Evaluation of vulvovaginal symptoms and Candida colonization in women with type 2 diabetes mellitus treated with canagliflozin, a sodium glucose co-transporter 2 inhibitor. Curr Med Res Opin. 2012;28(7):1173-1178. doi:10.1185/03007995.2012.69705310. Perkovic V, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med. 2019;380(24):2295-2306. doi:10.1056/NEJMoa181174411. Rosenwasser RF, et al. SGLT-2 inhibitors and their potential in the treatment of diabetes. Diabetes Metab Syndr Obes. 2013 Nov 27;6:453-67. doi: 10.2147/DMSO.S34416. PMID: 24348059; PMCID: PMC3848644.12. Sridharan K, Sivaramakrishnan G. Risk of limb amputation and bone fractures with sodium glucose cotransporter-2 inhibitors: a network meta-analysis and meta-regression. Expert Opin Drug Saf. 2025;24(7):797-804. doi:10.1080/14740338.2024.237775513. Ueda P, et al. Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: nationwide register based cohort study. BMJ. 2018;363:k4365. Published 2018 Nov 14. doi:10.1136/bmj.k436514. Watts NB, et al. Effects of Canagliflozin on Fracture Risk in Patients With Type 2 Diabetes Mellitus. J Clin Endocrinol Metab. 2016 Jan;101(1):157-66. doi: 10.1210/jc.2015-3167. Epub 2015 Nov 18. PMID: 26580237; PMCID: PMC4701850.15. Zhuo M, et al. Association of Sodium-Glucose Cotransporter-2 Inhibitors With Fracture Risk in Older Adults With Type 2 Diabetes. JAMA Netw Open. 2021;4(10):e2130762. Published 2021 Oct 1. doi:10.1001/jamanetworkopen.2021.3076216. Emerson Cestari Marino, Leandra Anália Freitas Negretto, Rogério Silicani Ribeiro, Denise Momesso, Alina Coutinho Rodrigues Feitosa, Marcos Tadashi Kakitani Toyoshima, Joaquim Custódio da Silva Junior, Sérgio Vencio, Marcio Weissheimer Lauria, João Roberto de Sá, Domingos A. Malerbi, Fernando Valente, Silmara A. O. Leite, Danillo Ewerton Oliveira Amaral, Gabriel Magalhães Nunes Guimarães, Plínio da Cunha Leal, Maristela Bueno Lopes, Luiz Carlos Bastos Salles, Liana Maria Torres de Araújo Azi, Amanda Gomes Fonseca, Lorena Ibiapina M. Carvalho, Francília Faloni Coelho, Bruno Halpern, Cynthia M. Valerio, Fabio R. Trujilho, Antonio Carlos Aguiar Brandão, Ruy Lyra e Marcello Bertoluci. Rastreamento e Controle da Hiperglicemia no Perioperatório – Posicionamento Conjunto da Sociedade Brasileira de Diabetes (SBD), Sociedade Brasileira de Anestesiologia (SBA) e Associação Brasileira para o Estudo da Obesidade e Síndrome Metabólica (ABESO). Diretriz Oficial da Sociedade Brasileira de Diabetes (2025). DOI: 10.29327/5660187.2025-10 , ISBN: 978-65-5941-367-6.17. Singh LG, Ntelis S, Siddiqui T, Seliger SL, Sorkin JD, Spanakis EK. Association of Continued Use of SGLT2 Inhibitors From the Ambulatory to Inpatient Setting With Hospital Outcomes in Patients With Diabetes: A Nationwide Cohort Study. Diabetes Care. 2024;47(6):933-940. doi:10.2337/dc23-112918. Mehta PB, Robinson A, Burkhardt D, Rushakoff RJ. Inpatient Perioperative Euglycemic Diabetic Ketoacidosis Due to Sodium-Glucose Cotransporter-2 Inhibitors - Lessons From a Case Series and Strategies to Decrease Incidence. Endocr Pract. 2022;28(9):884-888. doi:10.1016/j.eprac.2022.06.00619. Umapathysivam MM, Morgan B, Inglis JM, et al. SGLT2 Inhibitor-Associated Ketoacidosis vs Type 1 Diabetes-Associated Ketoacidosis. JAMA Netw Open. 2024;7(3):e242744. Published 2024 Mar 4. doi:10.1001/jamanetworkopen.2024.274420. Fleming N, Hamblin PS, Story D, Ekinci EI. Evolving Evidence of Diabetic Ketoacidosis in Patients Taking Sodium-Glucose Cotransporter 2 Inhibitors. J Clin Endocrinol Metab. 2020;105(8):dgaa200. doi:10.1210/clinem/dgaa20021. Neuen BL, Young T, Heerspink HJL, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2019;7(11):845-854. doi:10.1016/S2213-8587(19)30256-622. Braunwald E. Gliflozins in the Management of Cardiovascular Disease. N Engl J Med. 2022;386(21):2024-2034. doi:10.1056/NEJMra211501123. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373(22):2117-2128. doi:10.1056/NEJMoa150472024. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377(7):644-657. doi:10.1056/NEJMoa161192525. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2019;380(4):347-357. doi:10.1056/NEJMoa181238926. McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381(21):1995-2008. doi:10.1056/NEJMoa191130327. Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-1424. doi:10.1056/NEJMoa202219028. Anker SD, Butler J, Filippatos G, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021;385(16):1451-1461. doi:10.1056/NEJMoa210703829. Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2020;383(15):1436-1446. doi:10.1056/NEJMoa202481630. The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, et al. Empagliflozin in...
Fear Isn't Just in Your Mind: It Lives in Your Kidneys(Urinary System + Generational Trauma Healing)
Fear isn't just a thought.For many women, fear is a body pattern — and it often lives in the kidneys, adrenals, pelvic floor, and urinary system.In this episode of The Sovereign Sisterhood Movement Podcast (Body Systems + Generational Healing Series), I'm breaking down — in simple language — how your urinary system is actually one of your body's main survival + safety systems.What you'll learn in this episode:-Why anxiety and chronic stress can show up as a kidney/adrenal pattern (not a “weak mindset”)-How generational trauma trains the body to stay on alert (and why it feels like you can't relax even when life is “fine”)-The urinary system basics: kidneys, bladder, urethra, pelvic floor — and what they're doing all day to keep you alive-How cortisol + adrenaline overload the system (and why dehydration can make anxiety louder)-The Root Chakra connection (safety, support, trust, survival) through trauma-informed Kundalini Yoga Therapy-The faith over fear reframe through A Course in Miracles spiritual psychotherapy: how faith can become chemical, not just spiritual-A simple, supportive kidney-nourishing practice + recipe you can start integrating right awayNow here's your Permission (because you might be in the “I didn't even know this was a thing” stage)-If you've been blaming yourself for being “too anxious,” “too tense,” or “unable to rest”…you're not broken.Your body may have been trained, for generations, to live like danger is always around the corner.And the good news is: the body can be re-educated. Safety can be rebuilt. Faith can be embodied. Your nervous system and brain can learn a new normal.Want support doing this work with structure + sisterhood?I'm Veronica Barragán, trauma-informed Kundalini Yoga Therapist and founder of The Sovereign Sisterhood Sanctuary, an online sanctuary for first-time cycle breakers healing rewiring their nervous system + brain from generationla trauma body + mind + spirit.If this episode hit home, your next step is simple:✨ Join us inside the Sanctuary (link below) and start rebuilding safety from the inside out.
NSH Poster Podcast (2025): Comparative assessment of routine H&E and Mason's Trichrome Stain to Differentiate Normal from Infected Urinary Bladders in the Göttingen Minipig
Title: Comparative assessment of routine H&E and Mason's Trichrome Stain to Differentiate Normal from Infected Urinary Bladders in the Göttingen Minipig Authors: Stephanie D. Rivera, MS, HT(ASCP); Anthony Romanello, BS; Ronnie Chamanza, BVSc, MSc, FRC Path, MRCVS, FIATP, Preclinical Sciences & Translational Safety, Johnson & Johnson Innovative Medicine, Spring House, Pa Abstract: The objective of this experiment was to evaluate the difference between normal and infected Göttingen minipig urinary bladder and determine the difficulty of microscopically evaluating infectious urinary bladder. The focus was on the histology of the tissue using routine Hematoxylin and Eosin(H&E) staining and the Masson Trichrome (MT) special stain to demonstrate the morphology of normal and infectious urinary bladder. To improve on the translation between preclinical and clinical studies, the Göttingen minipig model is appropriate to use for research for diseased human bladder treatment because the minipig anatomy and organ system are similar to humans. The procedure was designed to evaluate normal uninfected urinary bladder and bacteria infected (E. coli) urinary bladder by evaluating morphology/cellular changes associated with the resultant inflammatory response in the urinary bladder of the Ellegaard Gottingen Minipig. The H&E-stained urinary bladder tissue section and a Masson Trichrome stained urinary bladder section were used to evaluate control ‘normal' tissue vs infected tissue cellular differences. Optimal microscopic evaluation requires that the urinary bladders are properly fixed and processed. By using proper fixation and diligent histologic practices, all components of the urinary bladder are captured for proper histologic evaluation.
#385 - Dr. Andrew Beverstock - Exploring Neonatal Nutrition: The Role of Urinary Sodium
Send us a textIn this episode, Dr. Andrew Beverstock discusses his research on urinary sodium and its relationship with growth in preterm neonates. He shares insights into the importance of sodium for neonatal growth, the methodology of his study, and the unexpected results that challenge existing literature. The conversation also touches on his diverse medical training, mentorship experiences, and his involvement in medical education and point-of-care ultrasound (POCUS). Dr. Beverstock emphasizes the significance of careful population selection in research and outlines his future research directions. Support the showAs always, feel free to send us questions, comments, or suggestions to our email: nicupodcast@gmail.com. You can also contact the show through Instagram or Twitter, @nicupodcast. Or contact Ben and Daphna directly via their Twitter profiles: @drnicu and @doctordaphnamd. The papers discussed in today's episode are listed and timestamped on the webpage linked below. Enjoy!
EM Quick Hits 69 Pediatric Urinary Retention & Acute Transverse Myelitis, Post-Dural Puncture Headache, Med Mal Cases: Clenched Fist Injury, IV Thrombolysis for Minor Stroke, EM Leadership Spotlight #4
On this month's EM Quick Hits podcast: Deborah Schonfeld on the differential diagnosis and work up of pediatric urinary retention & acute transverse myelitis, Jesse McLaren on his Tryptic Approach to Occlusion MI Diagnosis, Matthew McArthur on recognition and management of post-dural puncture headache, Joseph Yasmeh on Med Mal Cases: Clenched fist injury, Brit Long on IV thrombolysis for minor strokes and Victoria Myers & Lauren Westafer on mentorship and what it means to be a physician leader... Please consider a donation to EM Cases to support high quality Free Open Access Medical Education here: https://emergencymedicinecases.com/donation/
The latest in cat urinary disease with Dr. Allison Kendall
Why do so many indoor cats develop urinary disease? Meet Dr. Allison Kendall, Associate Professor of Internal Medicine at NC State and feline nephrology & urology specialist. In this episode of Purr Podcast, we talk pee, pain, and common causes for urinary probems in cats.
TRT: Your Complete Guide to Safe Dosing, Risks, and Boosting Longevity
Pre-Order The Forever Strong PLAYBOOK and receive exclusive bonuses: https://drgabriellelyon.com/playbook/Want ad-free episodes, exclusives and access to community Q&As? Subscribe to Forever Strong Insider: https://foreverstrong.supercast.comIn this compilation episode, Dr. Gabrielle Lyon is joined by the top experts in Testosterone and men's health treatments. You'll learn:Why aging alone doesn't drop T levels and why acquisition of conditions like obesity is the real culprit.Why the standard "low T" cutoff is misleading and why you must check your Free Testosterone.How erectile dysfunction is a sensitive marker of overall health and heart risk.The efficacy of Cialis/Viagra for both erections and cardiac protection, and the risks of unchecked influencer advice on steroids.The direct link between muscle mass, exercise, and sexual function—and why the penis is the "first to go" when overall health declines.Chapter Markers:0:00 - Testosterone is a Brain Hormone0:40 - Debunking the Myth: Male Menopause (Andropause) Doesn't Exist1:33 - The Dangers of Unchecked Influencer Advice on Testosterone3:07 - Defining Testosterone Deficiency: Symptoms vs. Signs5:10 - The Arbitrary Number: Why Guidelines Disagree on Low T8:29 - Free Testosterone: The Most Reliable Indicator of Male Health15:28 - TRT vs. Steroids: Defining the Line and Risks18:59 - The Real Risks of TRT: Infertility and Hematocrit22:36 - The Shocking Backstory: Challenging the Prostate Cancer Myth26:40 - Erectile Dysfunction (ED) and Lifestyle Modification29:21 - Shockwave Therapy for ED: The Science and the Cash Business33:53 - Penile Tissue Atrophy and Venous Leak37:25 - The Role of Muscle Mass, Sarcopenia, and Sexual Function39:41 - The Single Best Marker for Male Health: Erectile Function42:02 - The Science of Cialis and Viagra (PDE5 Inhibitors)45:49 - The Viagra Story: From Heart Drug to ED Cure50:50 - Tadalafil (Cialis) as a Triple-Threat Drug (Cardiac, Urinary, Sexual)53:57 - The Role of Testosterone in Female Sexual Function55:20 - Hypogonadism: Diagnosis, Treatment, and Fertility RiskAbout the guests: Dr. Abraham Morgentaler is an Associate Clinical Professor of Urology at Harvard Medical School and founder of Men's Health Boston. He is an internationally recognized expert in men's health, particularly known for his pioneering work in testosterone therapy. Dr. Morgentaler is credited with reversing the long-held belief that testosterone therapy causes prostate cancer and is the author of several books on men's health. YouTubeLinkedInT4L EducationX/Twitter Dr. Tobias Kohler is the co-founder of the Erectile Restoration Outcomes Study (EROS) penile implant registry. In addition to his clinical and research activities, Dr. Kohler is active in education, providing mentorship to residents and fellows.Mayo Clinic ResearchGateLinkedIn
Send us a textOver 200 million people worldwide suffer from incontinence but few seek treatment or education. Urinary incontinence is not age related and is manageable and treatable without surgery. Want more education and resources: nafc.org Support the showSeniorSupportStrategies.com when you need guidance navigating senior care or how to create your own Aging in Place strategy.
Ep.180 Beyond Kegels: Functional Pelvic Floor Care for Leaks, Prolapse & Painful Sex
Urinary (and yes, bowel) leakage isn't “just part of getting older”—it's a signal from your core and pelvic floor. In this straight-talk episode, physical therapist Christina Walsh, co-founder of Tighten Your Tinkler, joins me to dismantle the shame around pelvic health and lay out a functional path forward that goes far beyond “just do more Kegels.” We cover what's really driving leaks, pressure, prolapse, urgency, and painful sex in midlife; how breath, posture, fascia, and daily toileting habits influence symptoms; when conservative care is enough—and when devices, pessaries, or surgery may be appropriate. Christina also shares practical first steps you can start today (hello, decompression and diaphragmatic breathing), plus how to talk with your partner without pushing through pain.What you'll learnWhy leaking is common—but not normal—and what it's trying to tell youThe limits of isolated Kegels and what a functional approach looks likeHow breathing, posture, sitting, and constipation ramp up pelvic pressureStaging prolapse (1–4), what's realistic to “functionally heal,” and red-flagsPainful sex in midlife: estrogen, lubrication, tone, and boundaries that helpFascia's surprising role (yes, your bladder “talks” to your neck)Links & resourceshttps://www.tightenyourtinkler.com/ (listener code Michele for $50 off)https://www.instagram.com/tighten.your.tinkler/ Tighten Your Tinkler free quiz https://www.surveymonkey.com/r/tinklerquizIf this helped, share it with a friend, rate the show, and hop on my weekly newsletter for midlife health, fitness, and no-BS motivation._________________________________________1:1 health and nutrition coaching or Faster Way - Reach me anytime at mailto:mfolanfasterway@gmail.com If you're doing “all the right things” and still feel stuck, it may be time to look deeper. I've partnered with EllieMD, a trusted telehealth platform offering modern solutions for women in midlife—including micro-dosed GLP-1 peptide therapy—to support metabolic health and longevity. https://elliemd.com/michelefolan - Create a free account to view all products. ✨ Sign up for my weekly newsletter: https://michelefolanfasterway.myflodesk.com/i6i44jw4fq
Beyond Kegels: Know Your Options for Bladder Leaks
Live Greater | A University of Maryland Medical System Podcast
Urinary incontinence isn't “just part of getting older.” In this episode, Dr. Briana Walton, a urogynecologist at UM Capital Region Health, explains medical and surgical options to help, clears up myths, and shares why women don't have to live with bladder leaks in silence. For more information about Dr. Walton
Intelligent Medicine Radio for November 8, Part 2: New Non-Invasive Option for Men's Age-Related Urinary Problems
As little as 3000 steps per day can slow progression to Alzheimer's Disease; Self-reports of memory impairment soaring among young people; New study vindicates unprocessed red meat—and even often-vilified processed red meat—for cancer and overall health. Prostate artery embolization (PAE) offers new non-invasive option for men's age-related urinary problems; Targeting the mitochondria and the microbiome for Parkinson's Disease; Popular prostate and hair loss prevention drugs linked to depression and suicide—while Cialis for urinary symptoms may stave off cardiovascular disease; Discovery that a safe, cheap medication may increase survival after breast cancer surgery.
Managing UTIs: What You Need to Know, with Helen Lake, Specialist Urology Nurse. S7. Ep 6.
Urinary tract infections — or UTIs — aren't the most glamorous topic, but they're incredibly important, and we just don't talk about them enough. If you've ever had one, you'll know how miserable they can be: the burning, the stinging, those endless trips to the loo, the pain, and that bone-crushing fatigue. They can really knock you sideways.For many women, UTIs become more common — and more stubborn — during perimenopause and menopause.In this episode, I'm joined by the brilliant Helen Lake, a specialist urology nurse, to help us understand why UTIs happen, why they mustn't be ignored, and what you can do about them — from medical treatments to nutrition and supplements.Helen explains everything you need to know about identifying, understanding, and managing UTIs — and hopefully banishing them for good. We cover the key symptoms, prevention strategies like staying hydrated and double-voiding, why test results aren't always conclusive, and when antibiotics are needed. We also look at the role of beneficial bacteria, cranberry and D-mannose, vaginal moisturisers, topical oestrogen, and how to advocate for yourself with your GP.If you've found this episode helpful, please share it with a friend who might benefit too. And if you love The Happy Menopause podcast, I'd be so grateful if you could leave a five-star rating and a quick review on Apple Podcasts — or wherever you like to listen.And don't forget to subscribe, so you don't miss out on upcoming episodes. These small steps make a huge difference to the algorithm, and help more women find the show.After all, every woman deserves to have a happy menopause.Check out the full Show Notes for this episode on my website www.well-well-well.co.uk/podcast, where you'll find all the relevant links and references for each guest. Learn how to build your own menopause diet to manage your symptoms with my book The Happy Menopause: Smart Nutrition to Help You Flourish. And if you're tired of feeling tired and grappling with brain fog, check out my new book: The Happy Menopause Guide to Energy; Nutrition to Rejuvenate Your Brain & Body. It's available in all the usual places.
Urinary Frequency, PTSD, Arthritis, Aid and Attendance, & Many More: Attorneys Carol Ponton and Matthew Hill Answer Veterans' Questions – Hill and Ponton Q&A 11.04.25
H&P Disability Direct - Live Answers on the Road to VA Compensation
~Chat opens 1 hour before stream~Here is the link to the Williams Waiver https://www.hillandponton.com/wp-content/uploads/2025/05/Waiver-example.pdfVA Disability Calculator is here https://www.hillandponton.com/va-disability-calculator/Struggling to get the benefits you know you deserve? Get a free case evaluation now! - https://www.hillandponton.com/free-case-evaluation?utm_source=youtube&utm_medium=organic-video&utm_campaign=description&utm_id=Livestream+ShowJoin in our Live VA Disability Q&A Session in which we answer your questions live. We can't get to every single question so we will answer them as they come in. If you have any questions about the VA Disability Benefits process you can ask the question in the comment section when we go live and a little earlier. We are nationwide VA Accredited Disability Lawyers. We can't wait to answer your questions!For a FREE Case Evaluation go here: https://www.hillandponton.com/free-ca...Visit our website at https://www.hillandponton.com/?utm_so...Like us on Facebook at www.facebook.com/HillandPontonFor questions please email us at Info@hillandponton.comSpeakers: TBAThe content of this YouTube channel is provided for informational purposes only and is not intended to constitute legal advice. You should not rely upon any information contained on this YouTube channel for legal advice. Viewing this YouTube channel is not intended to and shall not create an attorney-client relationship between you and Hill and Ponton, PA. Messages or other forms of communication that you transmit to this YouTube channel will not create an attorney-client relationship and thus information contained in such communications may not be protected as privileged. Hill and Ponton, PA does not make any representation, warranty, or guarantee about the accuracy of the information contained in this YouTube channel or in links to other YouTube channels or websites. This YouTube channel is provided "as is," does not represent that any outcome or result from the viewing of this channel. Your use viewing of this YouTube channel is at your own risk. You enjoy this YouTube channel and its contents only for personal, non-commercial purposes. Neither Hill and Ponton, PA, nor anyone acting on their behalf, will be liable under any circumstances for damages of any kind.
Prostate Cancer: Symptom Management and Optimizing Quality of Life
Urinary incontinence and sexual dysfunction are common side effects of prostate cancer treatment, but both are manageable. Dr. Lindsay Hampson explains the types of incontinence—stress, urge, mixed, and overflow—and how identifying the cause guides treatment. Management strategies include pelvic floor physical therapy, medications, and surgical options like slings or artificial urinary sphincters. For sexual dysfunction, approaches range from oral medications and vacuum devices to injections and implants. Dr. Michael Rabow also highlights the side effects of androgen deprivation therapy, including fatigue, depression, hot flashes, and cardiovascular risk. He outlines evidence-based strategies—like exercise, cognitive behavioral therapy, and medications—to help preserve well-being and quality of life during treatment. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40869]
Prostate Cancer: Symptom Management and Optimizing Quality of Life
Urinary incontinence and sexual dysfunction are common side effects of prostate cancer treatment, but both are manageable. Dr. Lindsay Hampson explains the types of incontinence—stress, urge, mixed, and overflow—and how identifying the cause guides treatment. Management strategies include pelvic floor physical therapy, medications, and surgical options like slings or artificial urinary sphincters. For sexual dysfunction, approaches range from oral medications and vacuum devices to injections and implants. Dr. Michael Rabow also highlights the side effects of androgen deprivation therapy, including fatigue, depression, hot flashes, and cardiovascular risk. He outlines evidence-based strategies—like exercise, cognitive behavioral therapy, and medications—to help preserve well-being and quality of life during treatment. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40869]
Prostate Cancer: Symptom Management and Optimizing Quality of Life
Urinary incontinence and sexual dysfunction are common side effects of prostate cancer treatment, but both are manageable. Dr. Lindsay Hampson explains the types of incontinence—stress, urge, mixed, and overflow—and how identifying the cause guides treatment. Management strategies include pelvic floor physical therapy, medications, and surgical options like slings or artificial urinary sphincters. For sexual dysfunction, approaches range from oral medications and vacuum devices to injections and implants. Dr. Michael Rabow also highlights the side effects of androgen deprivation therapy, including fatigue, depression, hot flashes, and cardiovascular risk. He outlines evidence-based strategies—like exercise, cognitive behavioral therapy, and medications—to help preserve well-being and quality of life during treatment. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40869]
Prostate Cancer: Symptom Management and Optimizing Quality of Life
Urinary incontinence and sexual dysfunction are common side effects of prostate cancer treatment, but both are manageable. Dr. Lindsay Hampson explains the types of incontinence—stress, urge, mixed, and overflow—and how identifying the cause guides treatment. Management strategies include pelvic floor physical therapy, medications, and surgical options like slings or artificial urinary sphincters. For sexual dysfunction, approaches range from oral medications and vacuum devices to injections and implants. Dr. Michael Rabow also highlights the side effects of androgen deprivation therapy, including fatigue, depression, hot flashes, and cardiovascular risk. He outlines evidence-based strategies—like exercise, cognitive behavioral therapy, and medications—to help preserve well-being and quality of life during treatment. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40869]
Urinary incontinence affects millions of women, yet many continue to suffer in silence due to stigma or the misconception that it's just a normal part of aging. Bladder control issues can impact women of all ages, and they are highly treatable, and there are real solutions that can help. On this episode of the Healthier You Podcast, Dr. Ashlee Williams welcomes Dr. Nwamaka Fadahunsi, a board-certified urologist at Kaiser Permanente, to discuss the causes of urinary incontinence and the many tools available to treat it. Dr. Fadahunsi explains the differences between stress and urge incontinence, debunks common myths, and offers practical guidance on what women can do at home. She also outlines the full range of treatment options, including physical therapy, medications, and outpatient procedures, helping women regain control and confidence without relying on pads or assuming surgery is the only answer. Learn more about Nwamaka Fadahunsi, MD
In this very special 100th episode of the Cat Café Podcast, Dr. Susan and Dr. Jolle take a cozy walk down memory lane — catnip lattes in hand — to celebrate a century of cat conversations!
#270: Regain Control & Confidence with Dr. Nigel Brayer
Urinary incontinence is more common than you think. It's rarely talked about. Dr. Nigel Bayer sheds light on this often-ignored issue, offering real solutions to help women restore confidence and improve their quality of life. In this episode, we explore: The root causes of urinary incontinence—and why conventional advice like Kegels or medication often falls short. The Iron Clad Bladder System, an innovative approach using neuroplasticity and nervous system retraining for lasting results. Practical, holistic strategies to improve urinary health naturally without surgery, drugs, or fear of leaks. It's time to take back control. Tune in and discover a new path to freedom! About Dr. BrayerDr. Nigel Brayer, a nationally recognized expert in natural medicine and the creator of the -Iron Clad Bladder System, a groundbreaking, drug-free approach that combines modern neurology and traditional Chinese medicine to heal urinary incontinence. With over 27 years of experience, he has helped countless women overcome this life-altering condition by addressing both the physical symptoms and the deeper neurological and emotional roots of the issue. About TheresaA wife and a mother to two children and grandmother, Theresa Alexander Inman is a Parenting Coach, Board Certified Behavior Analyst, Infant Toddler Development Specialist, Autism Spectrum Disorder Clinical Specialist. Introduced to behavior analysis in 2007 after years in the juvenile justice system.Her goal is to improve the lives of children and families by helping them strategize child develop skills to prevent or reduce the effects of possible delays while having fun! She also served as a panelist on the first annual Autism World Summit.Theresa is also an author, having published “Pathways to Early Communication” in 2022.Connect with Theresa today!• Instagram | Theresa Inman• LinkedIn | Theresa Inman• BabyBoomer.org | Theresa Inman• YouTube | Parenting with Confidence• Tiktok | https://www.tiktok.com/@parentcoachtheresa• Spotify via Anchor.fm | Parenting with Confidence Website: https://www.theresaalexanderinman.com/About Parenting on the SpectrumRaising autistic children comes with unique joys, challenges, and learning moments. Join host Theresa as she explores the diverse experiences of parenting kids on the spectrum. Each episode features expert insights, real-life stories, and practical strategies to help you navigate this journey with understanding, compassion, and strength. Whether you're a parent, caregiver, or ally, this podcast is your go-to resource for fostering connection and celebrating neurodiversity. Please share, comment, rate, and download! Be blissful! Theresa
Prostate Cancer Survivorship: Urinary and Sexual Wellness
Dr. Lindsay Hampson discusses urinary incontinence and sexual dysfunction following prostate cancer treatment, emphasizing that both are common and treatable. She explains the different types of incontinence—stress, urge, mixed, and overflow—and outlines how understanding the cause helps guide treatment. Options include pelvic floor physical therapy, medications, surgical interventions like slings or artificial sphincters, and supportive devices. Dr. Hampson also reviews effective strategies for managing erectile dysfunction, such as oral medications, vacuum devices, injections, and penile implants. She highlights the importance of shared decision-making and reassures patients that even small symptoms can significantly affect quality of life and deserve attention. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40814]
Prostate Cancer Survivorship: Urinary and Sexual Wellness
Dr. Lindsay Hampson discusses urinary incontinence and sexual dysfunction following prostate cancer treatment, emphasizing that both are common and treatable. She explains the different types of incontinence—stress, urge, mixed, and overflow—and outlines how understanding the cause helps guide treatment. Options include pelvic floor physical therapy, medications, surgical interventions like slings or artificial sphincters, and supportive devices. Dr. Hampson also reviews effective strategies for managing erectile dysfunction, such as oral medications, vacuum devices, injections, and penile implants. She highlights the importance of shared decision-making and reassures patients that even small symptoms can significantly affect quality of life and deserve attention. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40814]
Prostate Cancer Survivorship: Urinary and Sexual Wellness
Dr. Lindsay Hampson discusses urinary incontinence and sexual dysfunction following prostate cancer treatment, emphasizing that both are common and treatable. She explains the different types of incontinence—stress, urge, mixed, and overflow—and outlines how understanding the cause helps guide treatment. Options include pelvic floor physical therapy, medications, surgical interventions like slings or artificial sphincters, and supportive devices. Dr. Hampson also reviews effective strategies for managing erectile dysfunction, such as oral medications, vacuum devices, injections, and penile implants. She highlights the importance of shared decision-making and reassures patients that even small symptoms can significantly affect quality of life and deserve attention. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40814]
Prostate Cancer Survivorship: Urinary and Sexual Wellness
Dr. Lindsay Hampson discusses urinary incontinence and sexual dysfunction following prostate cancer treatment, emphasizing that both are common and treatable. She explains the different types of incontinence—stress, urge, mixed, and overflow—and outlines how understanding the cause helps guide treatment. Options include pelvic floor physical therapy, medications, surgical interventions like slings or artificial sphincters, and supportive devices. Dr. Hampson also reviews effective strategies for managing erectile dysfunction, such as oral medications, vacuum devices, injections, and penile implants. She highlights the importance of shared decision-making and reassures patients that even small symptoms can significantly affect quality of life and deserve attention. Series: "Prostate Cancer Patient Conference" [Health and Medicine] [Show ID: 40814]
Your Bladder Matters: Common Urinary Issues in Women
Send us a textHave you ever wondered why urinary issues seem to affect women differently than men? The answer lies in our unique anatomy and hormonal makeup — factors that make female urinary health both fascinating and complex.Dr. Holly Thacker takes listeners on a comprehensive journey through the most common urologic conditions affecting women during Urology Awareness Month. From the annoying but potentially dangerous urinary tract infections to the embarrassing reality of pelvic organ prolapse that affects up to one in eight women, this episode breaks down what's happening and why."Everyone needs a bladder that works," Dr. Thacker emphasizes as she explores how bladder health connects to overall wellness and quality of life. She tackles taboo topics with medical precision while offering practical advice for prevention and management. You'll learn why maintaining pelvic floor strength matters even if you've never been pregnant, how hormonal changes dramatically affect urologic health, and why sexual function is inextricably linked to bladder health.Subscribe to the Speaking of Women's Health Podcast wherever you listen to podcasts and visit speakingofwomenshealth.com for more resources on taking charge of your health.Support the show
Episode 182 - Bladder Health After Cancer: What's Normal and What's Not
In this episode of The Menopause and Cancer Podcast, we're joined by Dr Carys Sonnenberg — GP, menopause specialist, and women's health expert — for a practical, empowering workshop all about bladder health.We ask the questions many of us wonder but rarely say out loud:What's normal when it comes to bladder habits?How often is too often to wee?Urinary tract infections and treatmentsProlapse and what helpsDr Carys breaks it all down for us — from understanding how cancer treatment, menopause, and pelvic floor changes can affect bladder function, to simple and effective things you can do to feel more confident and in control.We also explore what can help, including:Pelvic floor exercisesLifestyle strategiesHormone-free treatmentsMedications that may be suitable for cancer survivorsEpisode Timestamps:00:00 Intro04:04 Understanding Bladder Health Issues07:24 Discussing Sensitive Health Symptoms12:27 Pelvic Floor and Bladder Health15:10 Urinary Health and Hygiene Tips19:11 Managing Acute & Recurrent UTIs21:34 Managing Recurrent Urine Infections24:54 Managing Bladder Urges & Incontinence33:20 Individualised Pelvic Floor Treatment34:59 Cancer, Intimacy, and Body Image44:46 Pelvic Floor Exercise Misconceptions50:01 Overcoming Pelvic Floor ChallengesBuy my book here: Navigating Menopause After Cancer: https://www.amazon.co.uk/Navigating-Menopause-After-Cancer-comprehensive/dp/1068499907You can find Dr Sonnenberg here https://rowenahealth.co.uk/These are resources Dr Sonnenberg mentions: https://thepogp.co.uk/resources/booklets/https://squeezyapp.com/ Connect with us:For more information and resources visit our website: www.menopauseandcancer.org Or follow us on Instagram @menopause_and_cancerJoin our Facebook group: www.facebook.com/groups/menopauseandcancerchathub
Contributor: Travis Barlock MD Educational Pearls: Meningitis retention syndrome is a relatively novel and rare clinical condition Aseptic meningitis + acute urinary retention One study reports an incidence of about 8% in patients with acute aseptic meningitis Clinical presentation Typical meningeal symptoms including fever, stiff neck, and headache Urinary retention occurs about one week after initial symptoms Potential pathophysiology Immune-mediated dysfunction of the central nervous system Detrusor muscle underactivity from inflammation of the spinal cord Management Supportive care Bladder decompression References Hiraga A, Kuwabara S. Meningitis-retention syndrome: Clinical features, frequency and prognosis. J Neurol Sci. 2018;390:261-264. doi:10.1016/j.jns.2018.05.008 Pellegrino F, Funiciello E, Pruccoli G, et al. Meningitis-retention syndrome: a review and update of an unrecognized clinical condition. Neurol Sci. 2023;44(6):1949-1957. doi:10.1007/s10072-023-06704-0 Summarized & Edited by Jorge Chalit, OMS4 Get your tickets to Tox Talks Event, Sept 11, 2025: https://emergencymedicalminute.org/events-2/ Donate: https://emergencymedicalminute.org/donate/
Episode 202: BPA OverviewWritten by Cameron Carlisle, MSIV, Ross University School of Medicine. Comments by Hector Arreaza, MD.You are listening to Rio Bravo qWeek Podcast, your weekly dose of knowledge brought to you by the Rio Bravo Family Medicine Residency Program from Bakersfield, California, a UCLA-affiliated program sponsored by Clinica Sierra Vista, Let Us Be Your Healthcare Home. This podcast was created for educational purposes only. Visit your primary care provider for additional medical advice._____________________Arr: Welcome to another episode of Rio Bravo qWeek. My name is Hector Arreaza, I'm an associate program director and faculty in the Rio Bravo Family Medicine Residency Program. Today my co-host is Cameron Carlisle, who is a 4th-year medical student finishing his last rotation of med school. Welcome, Cameron, please introduce yourself.Arreaza: What are we talking about today, Cameron?Cam: Dr. Arreaza, did you know you're probably carrying around a chemical in your body that mimics estrogen? In fact, a 2004 CDC study found over 92% of Americans had detectable levels of Bisphenol A (BPA) in their urine. Today's topic is BPA.BPA is everywhere: receipts, water bottles, canned foods, baby bottles, and even our dental fillings. It's one of the most ubiquitous endocrine-disrupting chemicals (EDCs), which interferes with the body's hormone systems. That's why today's episode is about making the invisible visible. Our goals for today's podcast:Break down what BPA isShow how it affects the human bodyExplain how you and your patients can limit exposureEmpower both clinicians and the public with real, practical informationArreaza: Thanks for clarifying BPA today. It seems like we always have to learn about a new carcinogen or toxic substance that we are exposed to. I remember when I was a child, Yellow #5 became very concerning for the general public but it is still being used in our foods. So, it's good you are talking about this. What Is BPA?Cam: Bisphenol A (BPA) is an industrial chemical used since the 1950s, primarily in polycarbonate plastics and epoxy resins. It makes plastic clear, and is often found in:Water bottlesCanned food liningsBaby bottles (pre-2012)Takeout containersCash register receiptsDental sealantsArreaza: So, I've seen the “BPA-free” labels many times, and today I'm glad you are going to shed some light about it.Cam: What's alarming is that BPA leaches out of these products, especially when exposed to heat, acidity, or repeated use. A Harvard study found that people who drank from plastic bottles for just one week had a 69% increase in urinary BPA levels (Carwile & Michels, 2009).Arreaza: That's a lot of people 69%. Section 3: What happens when BPA gets into our body? How BPA Works in the BodyCam: BPA is classified as an endocrine disruptor, meaning it can bind to estrogen receptors and mimic or block natural hormone functions.It affects:Reproductive systems (both male and female)NeurodevelopmentThyroid signalingPancreatic β-cell functionMetabolism and fat storageEven low-dose exposure can disrupt cellular function. BPA acts as a xenoestrogen (foreign estrogen) and has been shown to alter DNA methylation, leading to epigenetic changes that persist across generations (Manikkam et al., 2013).Arreaza: So, BPA can cause epigenetic changes that can be inherited. BPA can persist for generations in your offspring.BPA's Health Impacts – What the Research SaysHere's where it gets serious. Let's go system-by-system:1. Reproductive HealthFemales: Linked to PCOS, infertility, and early puberty (Peretz et al., 2014).Males: Reduced sperm count and motility; altered testosterone levels.2. Pregnancy and Birth OutcomesIncreased risk of preterm birth, gestational diabetes, and low birth weight (Snijder et al., 2013).Studies show BPA crosses the placenta, directly affecting the fetus.3. Neurological DevelopmentAssociated with ADHD, anxiety, and impaired executive function in children exposed in utero (Mustieles et al., 2015).4. Metabolism and DiabetesBPA exposure is linked to insulin resistance, obesity, and type 2 diabetes, even at low doses (Lang et al., 2008).5. CancerAnimal and human data link BPA to increased risk of breast and prostate cancer via estrogenic mechanisms.6. MortalityA 2020 JAMA study found individuals with higher BPA levels had a 49% increased risk of all-cause mortality compared to those with lower levels (Gao et al., 2020).Arreaza: You are scaring me. I wonder what my BPA level is in my blood. Actually, BPA can be detected in urine. This is the most common approach for population-level biomonitoring, because BPA and its metabolites are mostly excreted in urine. Studies have found that BPA is present in most people, even up to 85–99% in large cohorts. Cam: That's literally everyone. Sources of BPA ExposureLet's talk about things we use every day:Thermal receipts (like from Target or Starbucks): BPA can transfer onto your skin and be absorbed, especially if your hands are wet or lotioned.Canned soups: One study showed that eating canned soup daily for five days led to a 1000% increased urinary BPA levels (Carwile et al., 2011).Plastic water bottles left in the car on hot days or plastic food trays for microwaving = chemical leaching.Baby bottles and pacifiers (pre-2012): primary concern for newborns.Arreaza: So, Cameron, you were exposed to BPA as a baby.Cam: Here's the jaw-dropper: We ingest up to 5 grams of plastic per week, roughly the weight of a credit card (WWF, 2019; University of Newcastle). This includes microplastics like BPA, which enter through food, water, and air.Arreaza: So, it translates into 40 lbs of plastic in a lifetime, by age 70. What can we do as family physicians?Family Medicine and Preventive CareAs family physicians, we are at the frontlines of prevention. Our role includes:Anticipatory guidance: during prenatal visits, well-child visits, and chronic disease managementScreening opportunities: ask about storage habits, microwave use, and receipt handlingEnvironmental health counseling: AAFP recommends addressing endocrine disrupting chemicals (EDCs) when relevant to a patient's concerns.It's not just about treating diabetes or obesity. It's about recognizing that environmental exposure may be a root cause.Arreaza: Prevention is my favorite topic!Cam: One helpful clinical practice:Arreaza: What else can we do to reduce BPA exposure?Practical Steps to Reduce BPAHere's what patients and doctors alike can do today:Switch to BPA-free products, but be careful, as replacements like BPS or BPF may also be harmful (Rochester & Bolden, 2015).Avoid microwaving or dishwashing plastic containers.Use digital receipts.Filter tap water using carbon filters, which can reduce microparticle ingestion.Choose fresh produce over canned goods when possible.Also, wash your hands after handling receipts, especially before eating or touching your face.Arreaza: What is our government doing to protect us?Public Health and Policy UpdatesRegulations are slowly catching up:The FDA banned BPA in baby bottles and sippy cups in 2012.The European Union has stricter limits, and France banned BPA in all food packaging in 2015.California's Proposition 65 requires BPA warning labels.Arreaza: Proposition 65, passed by direct voter initiative in 1986, “WARNING: This product contains chemicals known to the State of California to cause cancer and birth defects or other reproductive harm.”Arreaza: The FDA is planning to phase out petroleum-based food dyes (certified color additives) from the American food supply – marking a significant milestone in the efforts to protect the public. Cam: Many products still contain BPA analogs (BPS, BPF), which are not yet well-regulated.This is where clinician advocacy matters, where we can guide public opinion and support legislative change.Arreaza: So, millions of pounds of toxic substances are produced by many industries in the US. As physicians, we have to stay informed and update our patients.Cameron: How can we wrap up this episode?Conclusion and TakeawaysBPA is a hormone disruptor hiding in plain sight.People are exposed to BPA every day, but small lifestyle changes can dramatically reduce it.Family medicine has a role in education, prevention, and advocacy.Let's all be part of the solution for our health and future generations. Stanley (tumblers) are not sponsoring this episode, and we did not receive any money from them. Arreaza: That's it for today's episode of Rio Bravo qWeek. If you enjoyed this episode, share it with a colleague or medical student who may need to know about BPA. I'm Dr. Arreaza, signing off.Cameron: Hopefully, in the future I will talk to you about more endocrine disrupting chemicals. Thanks for listening._____________________Even without trying, every night you go to bed a little wiser. Thanks for listening to Rio Bravo qWeek Podcast. We want to hear from you, send us an email at RioBravoqWeek@clinicasierravista.org, or visit our website riobravofmrp.org/qweek. See you next week! _____________________References:Carwile, J. L., & Michels, K. B. (2009). Urinary bisphenol A and obesity: NHANES 2003–2006. Environmental Research, 111(6), 825–830.Carwile, J. L., et al. (2011). Canned soup consumption and urinary bisphenol A: A randomized crossover trial. JAMA, 306(20), 2218–2220.Centers for Disease Control and Prevention (CDC). (2004). Fourth National Report on Human Exposure to Environmental Chemicals.Gao, X., et al. (2020). Urinary bisphenol A and mortality risk. JAMA Network Open, 3(8), e2011620.Lang, I. A., et al. (2008). Association of urinary bisphenol A with medical disorders and laboratory abnormalities in adults. JAMA, 300(11), 1303–1310.Manikkam, M., et al. (2013). Epigenetic transgenerational inheritance of disease. PLOS ONE, 8(1), e55387.Mustieles, V., et al. (2015). Bisphenol A and neurodevelopmental outcomes in children. Environmental Health Perspectives, 123(7), 689–695.Peretz, J., et al. (2014). Bisphenol A and reproductive health. Environmental Health Perspectives, 122(8), 775–786.Rochester, J. R., & Bolden, A. L. (2015). Bisphenol S and F: A systematic review. Environmental Health Perspectives, 123(7), 643–650.Snijder, C. A., et al. (2013). Fetal growth and prenatal exposure to bisphenol A. Environmental Health Perspectives, 121(3), 393–398.World Wildlife Fund (WWF). (2019). No Plastic in Nature: Assessing Plastic Ingestion from Nature to People.University of Newcastle (Australia). (2019). Human Consumption of Microplastics.Theme song, Works All The Time by Dominik Schwarzer, YouTube ID: CUBDNERZU8HXUHBS, purchased from https://www.premiumbeat.com/.
DR. SABINE VESTING -Postpartum Exercise & Your Pelvic Floor: What Really Happens with Running, Diastasis & Leakage
Send us a textIn this episode, I'm joined by Dr. Sabine Vesting, a pelvic health physiotherapist and researcher whose work explores how exercise impacts the pelvic floor and abdominal muscles postpartum. Her research dives into common symptoms like urinary incontinence, pelvic girdle pain, and vaginal heaviness, and how they affect daily life for new moms.Now based in Ottawa, Dr. Vesting leads cutting-edge studies at the Motor Function Measurement (MFM) Lab, including research on running-induced urinary incontinence, pelvic floor responses after a single run, and the use of intravaginal devices to reduce leakage in female runners. She's also writing a review on how to best measure intra-abdominal pressure during exercise.We talk about:-Does diastasis actually matter?-Coning and doming explained-Finding exercise you enjoy postpartum-Urinary incontinence and new solutions-Intravaginal devices to understand the pelvic floor in sport and runningTime Stamps1:00 Introduction6:05 work as a PhD10:40 does diastasis even matter?16:24 pelvic girdle pain after pregnancy 21:00 changes over the last 15 years28:58 being comfortable with activity postpartum34:21 looking at pain and causes40:18 getting better measurements 51:42 intra-abdominal pressure55:32 doing what works with patients58:28 rapid fire questionsCONNECT WITH CARRIEIG: https://www.instagram.com/carriepagliano/Website: https://carriepagliano.comCONNECT WITH SABINE:Website: https://mfmlab.caLinkedIn: https://www.linkedin.com/in/sabine-vesting-aa4317135/?originalSubdomain=se We are currently recruiting participants for our RCT, aimed at evaluating whether readily available intravaginal devices, such as off-the-shelf pessaries or tampons, can effectively reduce or eliminate urine leakage during running, enabling active women to remain physically engaged. The study offers a remote option and welcomes female runners from all of North America who experience urine leakage while running.https://mfmlab.ca/portfolio-items/running-induced-urinary-incontinence-rct/The Active Mom Podcast is A Real Moms' Guide to pregnancy, postpartum, perimenopause & beyond for active moms & the professionals who help them in their journey. This show has been a long time in the making! You can expect conversation with moms and professionals from all aspects of the industry. If you're like me, you don't have a lot of free time (heck, you're probably listening at 1.5x speed), so theses interviews will be quick hits to get your the pertinent information FAST! If you love what you hear, share the podcast with a friend and leave us a 5 ⭐⭐⭐⭐⭐ rating and review. It helps us become more visible in the search algorithm! (Helps us get seen by more moms that need to hear these stories!!!!)
Like the life cycle of a butterfly, menopause is a transformative season that has its highs and lows. Saying goodbye to periods and embracing the beauty found in midlife are the positives. But dealing with frustrating symptoms like hot flashes, insomnia, mood changes and more can feel overwhelming. If you are in your menopause era, you'll want to listen to part one of the latest episode of The Healthiest You podcast, where we talk about how to navigate each stage of menopause with OB-GYN and Menopause Society Certified Practitioner Susan Haas, MD, PhD, with Lehigh Valley Health Network (LVHN), part of Jefferson Health. What age does menopause start? How long does menopause last? What can help with hot flashes? Can all women take menopausal hormone therapy? How is bone health impacted during menopause? We answer these questions and more on The Healthiest You podcast this month. Chapters: · 0:01 - Intro · 1:08 - Perimenopause and menopause · 4:40 - Menstrual cycle changes · 8:23 - Help with hot flashes · 12:27 - Hormone therapy · 13:16 - When to consider hormone therapy · 14:51 - Alternative treatment options · 22:23 - Risks of hormone therapy · 25:36 - If you've had a total hysterectomy · 29:22 - Bone health and calcium supplements · 33:19 - Estrogen and progesterone · 36:47 - Urinary tract infections (UTIs) · 38:55 - Part two coming soon
Takes the Guess Work Out of Many Bladder and Vaginal Symptoms with Keely McCann
Dr. Kelly McCann is a board-certified physician in Internal Medicine and Pediatrics, trained in Functional, Integrative, and Environmental Medicine. Known for her expertise in mold illness, chronic infections, MCAS, and complex chronic conditions, she integrates science, intuition, and spiritual psychology to help people heal at the deepest levels. Through her private practice, The Spring Center, and her upcoming transformational programs, she guides clients from suffering to sovereignty—reclaiming their health, purpose, and power. She has hosted 3 virtual worldwide summits reaching over 100,000 people and an author of a forthcoming book that explores how illness is not the enemy but a portal to healing the whole self.https://thespringcenter.com/ https://drkellymccann.comhttps://www.facebook.com/drkellymccannhttps://www.instagram.com/drkellymccann/?hl=enhttps://www.youtube.com/@DrKellyMcCann____________________________________________________________________________________Come join my Buff Muff Community www.buffmuff.comThank you so much for listening! I use fitness and movement to help women prevent and overcome pelvic floor challenges like incontinence and organ prolapse. There is help for women in all life stages! Every Woman Needs A Vagina Coach! Please make sure to LEAVE A REVIEW and SUBSCRIBE to the show for the best fitness and wellness advice south of your belly button. *******************I recommend checking out my comprehensive pelvic health education and fitness programs on my Buff Muff AppYou can also join my next 28 Day Buff Muff Challenge https://www.vaginacoach.com/buffmuffIf you are feeling social you can connect with me… On Facebook https://www.facebook.com/VagCoachOn Instagram https://www.instagram.com/vaginacoach/On Twitter https://twitter.com/VaginaCoachOn The Web www.vaginacoach.comGet your Feel Amazing Vaginal Moisturizer Here
Episode 622: Ep 622 New Research for people dealing with Urinary & Bladder Issues.
Forever Young Radio Show with America's Natural Doctor Podcast
Millions of Americans are frustrated with their urinary problems. More specifically, the need to urinate multiple times a day and night and leaking urine is frustrating to many people over the age of 45. Fortunately, there have been successful advances in the herbal treatment of common urinary problems. We are excited to share these breakthroughs on the show today. Tracey Seipel, ND, is CEO and founder of Australian-based Seipel Group. Dr. Seipel is a renowned naturopathic doctor, medical herbalist, and clinical nutritionist. Dr. Seipel is also a diabetes educator, researcher, and an award-winning natural products formulator with 35 years of experience in clinical practice.She pioneered the natural urological health category receiving a Nutrition Business Journal award in 2006 for innovation. During the 1990s, Seipel was a leader in establishing standards of education for Australian naturopathic colleges and as an advisor to government boards, including developing nutritional training for Australia Medical Schools. During her research as a product formulator for nutraceutical companies, she uncovered the significant prevalence and underreporting of urinary incontinence in women and then overactive bladder and incontinence in both men and women. Together, this led to her pioneering this natural health category. Understanding the significant health impacts and seeing no other companies willing to take on the challenge of improving bladder control, Seipel developed the initial formulation.Learn more about UROXUROX StudyLearn more about Emerald Labs Bladder Health which contains the branded ingredient UROX. Listeners can save 20% OFF at Emeraldlabs.com when using the code: Forever
Dr David Nolan, assistant professor of Sport and Exercise Sciences at the DCU School of Health and Human Performance, talks about the frequency of urinary leakage as an issue for women of all ages and the importance of breaking the stigma around talking about it
Solifenacin Pharmacology
Real Life Pharmacology - Pharmacology Education for Health Care Professionals
Solifenacin is a bladder antimuscarinic medication most commonly used for overactive bladder (OAB) with symptoms of urinary frequency, urgency, and urge incontinence. Like other agents in its class, understanding the pharmacology can help anticipate potential side effects, drug interactions, and downstream prescribing problems. Mechanism of Action Solifenacin selectively blocks muscarinic M3 receptors in the bladder detrusor muscle. Inhibiting these receptors reduces involuntary bladder contractions, increases bladder capacity, and delays the urge to void. While M3 selectivity may theoretically reduce side effects compared to nonselective antimuscarinics, in clinical practice, many anticholinergic effects still occur. Adverse Effects Because muscarinic receptors are present throughout the body, solifenacin can lead to a range of anticholinergic adverse effects: Dry mouth – among the most common, can be significant enough to cause dental issues with long-term use. Constipation – especially problematic in older adults; severe cases may require hospitalization. Blurred vision – due to impaired accommodation. Cognitive impairment – increased risk in older adults, particularly with cumulative anticholinergic burden. Urinary retention – paradoxical worsening in patients with bladder outlet obstruction. Drug Interactions CYP3A4 inhibitors (e.g., ketoconazole, clarithromycin, ritonavir) can increase solifenacin plasma concentrations, raising the risk of side effects. Other anticholinergics (e.g., diphenhydramine, tricyclic antidepressants, other bladder antimuscarinics) can result in additive toxicity and higher anticholinergic burden. QT-prolonging drugs (e.g., amiodarone, certain fluoroquinolones) may have additive cardiac risk since solifenacin has been associated with QT prolongation in rare cases. Prescribing Cascade Examples Constipation → Laxative initiation – A patient starts solifenacin for OAB and develops severe constipation, leading to chronic use of stimulant laxatives like senna or bisacodyl. Dry mouth → Mouth rinse prescription – Dry mouth is treated with saliva substitutes or prescription rinses, instead of reassessing the anticholinergic therapy. Cognitive decline → Donepezil initiation – In older adults, cognitive impairment may be mistaken for dementia progression, leading to cholinesterase inhibitor prescribing—directly counteracting the anticholinergic effects of solifenacin. Solifenacin can be an effective treatment for OAB, but the risk of adverse effects and prescribing cascades—especially in older adults—cannot be ignored. Healthcare professionals should regularly review the indication, monitor for anticholinergic burden, and look for opportunities to deprescribe when appropriate.
Dr. John sits down with nurse practitioner Ruth Kriz to talk about her personal and professional journey with interstitial cystitis (IC). After years of misdiagnoses and living with chronic pain, Ruth uncovered what traditional medicine often misses — hidden infections, biofilms, and genetic factors that make healing harder. She explains how advanced testing, targeted treatments, and even vitamin D play a role in getting to the root of IC and other chronic urinary issues. Ruth also shares how to find practitioners who really understand these complex conditions and can help guide the healing process. Key Takeaways To Tune In For: (03:31) – What finally worked: finding answers and hope (04:58) – The hidden pathogens most tests don't catch (09:10) – Why traditional urine tests fall short (17:34) – How your genes can make infections stick around (19:40) – Ruth's personalized, targeted treatment approach (23:02) – Why vitamin D matters more than you think (29:20) – How to find practitioners who actually get it Resources talked about in this episode: Website: www.ruthkriz.com
Why men have urinary dribble and what to do about it! | After Dribble (YouTube Relay)
Have you ever experienced going to the bathroom and after relieving, a little bit just dribbles out as you close your zipper? Even I can tell that that's incredibly annoying for men! So here is what we know about post void Dribble or better known as urinary Dribble! Be sure to watch until the end to learn how you can minimize or even prevent this! Rena Malik, MD is a urologist and pelvic surgeon on youtube to educate people about all things urology including erectile dysfunction, how to increase testosterone, problems with sex, premature ejaculation, urinary leakage, or incontinence, overactive bladder, urinary tract infections, prostate issues and more. Subscribe: https://www.youtube.com/c/RenaMalikMD/?sub_confirmation=1 Share this video with a friend: https://youtu.be/k9Uoniw9Byk DISCLAIMER: This video is purely educational and does not constitute medical advice. The content of this video is my personal opinion and not that of my employer(s). Use of this information is at your own risk. Rena Malik, M.D. will not assume any liability for any direct or indirect losses or damages that may result from the use of the information contained in this video including but not limited to economic loss, injury, illness, or death. Learn more about your ad choices. Visit megaphone.fm/adchoices
The Urinary Explorations - Mini Prep Series Episode 7 | Sarah and Romana Bonus Series
Send us a textWelcome back guys, the explorations continue. This week's MINI PREP SERIES episode brings you insight into UTI's, diuretics, peak weeks and plenty more!If you have been tuning in, you'll know Romana and I are on a mission to talk about every area of prep, including the ones you may not have heard about.If you have any suggestions for us, be sure to let us know.All the love to you, our tribe.S & R xWatch it here: https://youtu.be/KGZ-gIsSjDITHE ULTIMATE SHOW DAY GUIDE E-BOOK: Purchase here Beyond Condition Coaching Application: Click here Find Sarah on Instagram: @sarahparker_bb
Nutritional Considerations for Healthy Cats and Feline Urinary Health
VetFolio - Veterinary Practice Management and Continuing Education Podcasts
Diet plays a role in feline kidney disease, urinary problems such as stones and crystals, feline lower urinary tract disease and gastrointestinal problems such as inflammatory bowel disease. Tune in to this CE episode of the VetFolio Voice podcast to gain insights behind feeding strategies for cats and their species-specific quirks. You'll learn the key factors in diets that support a cat's urinary tract health. You'll also get tips on how to provide informed recommendations for clients regarding feeding their healthy, young, adult cats.
NutraCast: Evvy connects the gut, vaginal and urinary health dots
Evvy, a vaginal microbiome testing and care company, launched in 2021 with a mission to close the gender health gap by leveraging overlooked female biomarkers. Through its platform, the company has built the world's largest dataset on the vaginal microbiome and is using this novel data to drive better outcomes in women's health.
Episode #199. Rewiring Medicine: A Physician's Path to Intuitive Healing, Dr Anona Blackwell, Genito-urinary specialist, author, academic
Can you be both a scientist and a mystic? In this extraordinary episode, Professor Selena Bartlett speaks with Dr. Anona Blackwell — a Lancet-published academic, former consultant physician, and author of From Medic to Mystic — about the turning point where evidence-based medicine no longer had all the answers.Raised in rural poverty in Wales and rising to the heights of British medical academia, Dr. Blackwell quietly navigated a parallel world of intuitive experiences, energy healing, and psychic insight. For decades, she kept this side hidden. Now, at 75, she's sharing it all — and helping rewire our understanding of medicine and healing.In this conversation, we explore:· The moments science couldn't explain — and why she couldn't ignore them· How trauma, intuition, and healing intersect in clinical settings· The courage it takes to speak about the unseen in a sceptical world· Why the future of medicine must integrate both body and energy, logic and intuitionDr. Blackwell's story challenges the idea that you must choose between science and spirit. Instead, she shows us that healing lives at the intersection of both.Her memoir, From Medic to Mystic, is available now.https://www.amazon.com/Medic-Mystic-Academic-Physicians-Paranormal/dp/1068511001Listen and discover what it really means to rewire medicine. Support the showSubscribe and support the podcast at https://www.buzzsprout.com/367319/supporters/newLearn more at www.profselenabartlett.com
Urinary tract infections (or UTIs) are more than a nuisance-they can be recurring and painful. Join our registered dietitians Melanie Beasley and Britni Vincent in our newest episode of Dishing Up Nutrition as they unravel the connection between your diet, your microbiome, and these infections. Listen now for expert insights regarding what makes UTIs such a frequent issue, and explore how specific foods and supplements can aid in prevention, relief, and recovery.
Uterine incarceration in pregnancy, is a rare but troublesome complication. This occurs when a retroverted uterus becomes trapped in the pelvic cavity during pregnancy. This happens when the uterus fails to move forward as it grows, becoming stuck between the sacral promontory and pubicsymphysis. It's more common in women with prior pelvic issues or uterine anomalies. Urinary retention is the most common symptom that occurs because of elongation of the urethra by displacement of the cervix, loss of the urethro-vesical angle, and mechanical compression of the bladder neck. It is estimated to occur in 1 in 3000 patients. How do we release an incarcerated uterus? Is laparoscopy an option? And how can an ultrasound probe help (April 2025publication)? Listen in for details.
87. Fixing Your Urgency Incontinence (And the Free Resource That You'll Need to Help!)
Urinary urgency and incontinence are topics that often don't get enough attention in women's health—which is exactly why we're diving into them in today's episode. Join hosts Amy and Krystle as they share top tips for better bladder health! It's common to be practicing unhealthy bladder habits without even knowing it, so we will cover what healthy habits should look like for you, your partner, and your kids!Urinary urgency is when you get the feeling that you have to rush to the bathroom, which can lead to incontinence. This is mainly caused by poor bladder habits. The good news is that you can retrain your bladder! We'll share some great tips and strategies to help retrain your brain and bladder for a more functional, healthy bladder. Whether you've had babies or not, these tips are for you!If you enjoyed listening to this episode, we would love it if you could share it to your Instagram stories and tag us, @expectingandempowered. As we like to say, knowledge is power, and we just really want to give more people the information that they may need on their motherhood journey!Expecting and Empowered Blog Post - Regaining Control: Tips for Dealing with Urge Urinary IncontinenceBladder Diary FREEBIE!Links & ResourcesExpecting and Empowered App - Enter code 'PODCAST25' at checkoutExpecting and Empowered WebsiteExpecting and Empowered InstagramThis episode was brought to you by the Pivot Ball Change Network.



































































