Podcasts about Thrombus
- 42PODCASTS
- 63EPISODES
- 20mAVG DURATION
- 1MONTHLY NEW EPISODE
- Nov 19, 2025LATEST
POPULARITY
Best podcasts about Thrombus
Latest news about Thrombus
- Covalent Organic Framework‐Based Nanomotor for Thrombus Therapy Wiley: Small: Table of Contents - Nov 14, 2025
- Fibrin‐Targeting Metal–Organic Framework Nanoagent for NIR‐Triggered Photothermal Thrombus Ablation Wiley: Advanced Healthcare Materials: Table of Contents - Nov 10, 2025
- Reactive Oxygen Species‐Responsive Biomimetic Nanoplatelets for Thrombus‐Mediated Photothermal Immunotherapy of Tumor Wiley: Angewandte Chemie International Edition: Table of Contents - Oct 13, 2025
- Engineered Probiotic‐Powered Micro‐Rod Robot Bomb for Thrombus‐Penetrating Explosion Wiley: Advanced Science: Table of Contents - Sep 25, 2025
- Surface Engineering of Thrombus‐Targeting Nanocarriers for Cardiovascular Diseases: A Short Review Wiley: Advanced Materials Interfaces: Table of Contents - Jun 6, 2025
- Phosphatidylcholine Liposome Accelerated Platinum Nanomachines (PLANEs) With Enhanced Penetration Capability for Thrombus Mechanotherapy Wiley: Advanced Materials: Table of Contents - Apr 24, 2025
- Rivaroxaban shown to be a viable alternative to warfarin for left ventricular thrombus The Medical News - Mar 29, 2025
- Self‐Actuated Clot‐Piercing Nanoassembly Enabling Adaptable Drug Activation and Synergistic Thrombus Ablation Wiley: Advanced Functional Materials: Table of Contents - Dec 16, 2024
- See what happens when a left main thrombus evolves from subtotal occlusion to total occlusion. Dr. Smith's ECG Blog - Oct 20, 2024
- Impact of occluder device configurations in in-silico left atrial hemodynamics for the analysis of device-related thrombus PLOS Computational Biology - Sep 26, 2024
Latest podcast episodes about Thrombus
Blut und Immunsystem, Gerinnungsstörungen
In dieser Woche tauchen wir tief in die faszinierende Welt der Blutgerinnung ein: Vom ersten Alarm an der verletzten Gefäßwand, über die Arbeit der Thrombozyten und der Gerinnungsfaktoren, bis hin zum stabilen Thrombus und der späteren Fibrinolyse. Wir erklären dir, was passiert, wenn die Balance gestört ist – von erhöhter Blutungsneigung über Thrombosen bis hin zur DIC. Lerne typische Warnzeichen zu erkennen und welche pflegerischen Maßnahmen entscheidend sind, um Patienten sicher zu begleiten – und damit machen wir dich wieder fit für deine Prüfungen und die praktische Arbeit auf Station.
ERUS25 special: Prof. Bernhard talks about surgical training for young urologists, and robotic nephrectomy in caval thrombus
UROONCO RCC associate editor Dr. Riccardo Bertolo (IT) talks to Prof. Jean-Christophe Bernhard (FR) about the lectures he presented during the ERUS25 Meeting. Prof. Bernhard discusses surgical training for the next generation of urologists, sharing practical advice and guidance to help young surgeons grow in their careers, as discussed in his Young ERUS lecture. He also shares details of his presentation on "Complex surgery of robotic nephrectomy in level 3 caval thrombus", and provides insights into treatment strategies, highlights the most critical preoperative considerations, and shares practical tips and tricks. He concludes with his opinion on whether robotic surgery represents the future for managing such challenging cases.This interview was recorded at ERUS25 in London, United Kingdom. For more updates on kidney cancer, please visit our educational platform UROONCO RCC.For more EAU podcasts, please go to your favourite podcast app and subscribe to our podcast channel for regular updates: Apple Podcasts, Spotify, EAU YouTube channel.
Stent-Retriever Thrombectomy in STEMI With Large Thrombus Burden: The RETRIEVE AMI Randomized Trial | JACC: Advances
Darshan H. Brahmbhatt, Podcast Editor of JACC: Advances, discusses a recently published original research paper on Stent-Retriever Thrombectomy in STEMI With Large Thrombus Burden: The RETRIEVE AMI Randomized Trial.
Reframing Thrombus Management: Beyond the Clot to Patient-Centered Outcomes in Pulmonary Embolism Treatment (Sponsored by Thrombolex)
In this episode, Drs. Vivian Bishay, Wissam Jaber and Dr. Vlad Lakhter review safety, patient selection, and risk stratification related to device selection. They examine the economics of outcomes in PE treatment, including workflow efficiency and the impact of avoiding post-procedure infusion and ICU resource use. Discussion ensues on the role of treatment location, ease of use, and how broader access to technology may influence care delivery.
Characterization and Clinical Outcomes of High-Risk Device-Related Thrombus in the Amulet IDE Trial | JACC: Clinical Electrophysiology
Dr. Emile Daoud, Deputy Editor of JACC Clinical Electrophysiology discusses Characterization and Clinical Outcomes of High-Risk Device-Related Thrombus in the Amulet IDE Trial.
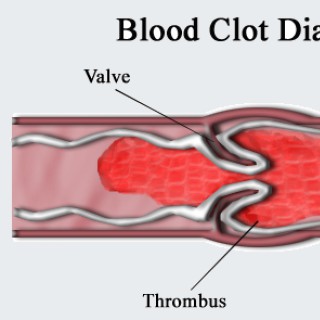
Speichel ist ein blutstillendes Mittel, das auch Bluter immer bei sich haben
Kleine Verletzungen sind im Alltag ganz normal, kleine Schnittwunden beim Rasieren, bei der Gartenarbeit oder beim Hantieren mit scharfkantigem Papier. Instinktiv stecken wir den blutenden Finger in den Mund und unterstützen so die Blutgerinnung. Das funktioniert auch mit dem Speichel von Blutern, hat Prof. Dr. Johannes Thaler von der MedUni Wien herausgefunden. Thaler ist an der Abteilung für Hämatologie und Hämostaseologie tätig. Eine Studie unter seiner Leitung hat sich mit Hämophilie-A-Patienten befasst - das ist die häufigste Form der Bluterkrankheit und betrifft einige hundert Patienten in Österreich. Die Ergebnisse zeigen, dass der Speichel dieser Patienten die Gerinnung des Blutes auslöst, was gerade bei an der Bluterkrankheit leidenden Menschen eine wichtige Information sein kann. Er finde es „hilfreich, seinen Patienten sagen zu können, dass auch ihr Gerinnungssystem teilweise sehr gut funktioniert. Also dass zum Beispiel der Speichel ein Hämostatikum ist, also ein blutstillendes Mittel ist, das sie immer bei sich haben." Und so funktioniert die Blutgerinnung bei gesunden Menschen: Im zirkulierenden Blut gibt es inaktive Vorstufen verschiedener Proteine, die sogenannten „Gerinnungsfaktoren". Um die Gefäße herum gibt es beispielsweise einen Gewebsfaktor, den Tissue-Faktor, und wenn es nun zu einem Gewebsschaden, zu einer Verletzung kommt, wird dieser Tissue-Faktor freigelegt, der kommt in Kontakt mit den anderen Gerinnungsfaktoren im Blut und dann wird die ganze Kaskade an Enzymen ausgelöst, die sich gegenseitig aktivieren und am Schluss steht dann die Bildung von Fibrin, eine Art Gewebskleber und die Aktivierung von Blutplättchen, auch Thrombozyten genannt. Diese verschließen die Wunde mit einem Thrombus, einem Pfropfen. Thaler: „Das ist ein ganz fein abgestimmter Prozess, denn es muss einerseits ausreichend gerinnen, sonst kommt es zu einer Blutung, es darf aber auch nicht zu viel gerinnen, denn sonst würde es zu einer Thrombose, Schlaganfall, Herzinfarkt etc. kommen."
Primary resistance to BCMA-targeted bispecifics in multiple myeloma, emapalumab therapy in hemophagocytic lymphohistiocytosis, and chemotherapy-induced pyroptosis as a mechanism of thrombus formation in patients with cancer
In this week's episode, we'll learn more about mechanisms of primary resistance to BCMA-targeted bispecific T-cell engagers in relapsed/refractory multiple myeloma, the effects of emapalumab therapy on outcomes in patients with pediatric hemophagocytic lymphohistiocytosis who receive stem cell transplants, and a cell death process that may help account for increased thromboembolic risk in patients receiving cancer chemotherapy.Featured Articles:Impact of soluble BCMA and non–T-cell factors on refractoriness to BCMA-targeting T-cell engagers in multiple myelomaEmapalumab therapy for hemophagocytic lymphohistiocytosis before reduced-intensity transplantation improves chimerismGSDME-mediated pyroptosis contributes to chemotherapy-induced platelet hyperactivity and thrombotic potential
TNSPPE: Vacationing in the Virgin Islands While Learning About Venous Thrombus Embolisms
In this episode, we discuss for educational purposes only, the concepts associated with VTEs and the relevant pharmacotherapeutics, for pharmacists in training. ---- Note: The views of this podcast represent those of my guest(s) and I. -- Note: Purpose of these episodes- not at all, for advice or medical suggestions. These are aimed to provide support for peer pharmacists in training in educational and intellectually stimulating ways. Again, these are not at all for medical advice, or for medical suggestions. Please see your local state and board-certified physician, PA or NP, and pharmacist for medical advice and suggestions. --- Note: Some of the content produced involved the use of A.I. .
JACC: Cardiovasc Interventions - Failed Thrombus Aspiration and Reduced Myocardial Perfusion in Patients With STEMI and Large Thrombus Burden
Abdullah Al-Abcha, MD, social media editor of JACC: Cardiovascular Interventions, and Sung Gyun Ahn, MD, PhD, discuss a recently published original research paper reporting the outcomes of failed thrombus aspiration in patients with STEMI and large thrombus burden.
369. Case Report: Apical Obliteration with Biventricular Thrombus – West Virginia University
CardioNerds, Dr. Richard Ferraro and Dr. Dan ambinder join Dr. Li Pang, Dr. Emily Hendricks, and Dr. Bei Jiang from West Virginia University to discuss the following case that features apical obliteration with biventricular thrombus. Dr. Christopher Bianco provides the Expert CardioNerd Perspectives & Review (E-CPR) for this episode. Audio editing by CardioNerds Academy Intern, student doctor Tina Reddy. A 37-year-old Caucasian man with a history of tobacco smoking and hypertension who presented with chest pain and elevated troponin was admitted for non-ST elevation myocardial infarction (NSTEMI). Ischemic evaluation with an invasive coronary angiogram was negative. He was treated as NSTEMI and scheduled for outpatient cardiac MRI (CMR). The patient came back 2 months later with right arm weakness and confusion and was found to have an embolic stroke. Labs showed positive troponin with a flat trend and hypereosinophilia. Transthoracic echocardiogram (TTE) showed obliteration of LV and RV apex with thrombus and reduced LV systolic function. CMR was consistent with myocarditis with biventricular thrombus. The patient was started on corticosteroids and warfarin. Hypereosinophilia workup was positive for PDGFRA alpha rearrangement. He was diagnosed with primary hypereosinophila syndrome. Imatinib was initiated. The patient was followed up with the hematology clinic, achieved a complete hematologic response with normalized cell count, and remained free from any cardiovascular event at the 8-month follow-up. US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here. CardioNerds Case Reports PageCardioNerds Episode PageCardioNerds AcademyCardionerds Healy Honor Roll CardioNerds Journal ClubSubscribe to The Heartbeat Newsletter!Check out CardioNerds SWAG!Become a CardioNerds Patron! Case Media Pearls - Apical Obliteration with Biventricular Thrombus Cardiac MRI is a valuable test for patients presenting with myocardial infarction with non-obstructive coronary arteries (MINOCA). Obliterated apex with apical thrombus on TTE with hypereosinophilia should raise high suspicion for eosinophilic myocarditis. Initiation of corticosteroids is the first-line treatment for eosinophilic myocarditis, which is associated with lower mortality in patients with myocarditis. For other potential complications, such as heart failure, intracardiac thrombus, arrhythmia, and pericardial effusion, the standard of care for each disorder is recommended. Hypereosinophilia can be seen in parasitic infections, vasculitis, asthma, allergy, hematological malignancies, and as a primary disorder. Show Notes - Apical Obliteration with Biventricular Thrombus What is the differential diagnosis for patients with elevated troponin and nonobstructive CAD? The occurrence of acute myocardial infarction (AMI) without significant CAD was reported 80 years ago. However, the term MINOCA (myocardial infarction with non-obstructive coronary arteries) has only been used recently to describe these patients. It involves ischemic and nonischemic etiologies. First, overlooked ischemic etiologies need to be ruled out by reconciling the angiogram images such as spontaneous coronary artery dissection (SCAD) and plaque disruption. Intracoronary imaging, such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT), may be applied to evaluate for SCAD and subtypes of plaque disruption when indicated. The investigation continues with nonischemic causes such as stress cardiomyopathy, myocarditis, pulmonary embolism, demand ischemia from sepsis, anemia, chest trauma, heart failure exacerbation, arrhythmia, and stroke. The diagnosis of MINOCA is established when it fulfills the following criteria: First, it is AMI by the Fourth Universal Definition; Second, less than 50% of stenotic lesion on angiogram; Third, there is no alternate diagnosis.
Pediheart Podcast #295: Right Atrial Thrombus Post Gore Cardioform ASD Closure - Reason For Concern?
This week we review a report from Italy regarding the observation of RA disk thrombus formation in some patients following GORE Cardioform ASD closure. How common is this complication seen and are there some patient or device characteristics that would be considered higher risk for this complication? How does this information square with the Assured trial data? Why might there be differences between the two data sources? We speak with Associate Professor of Pediatrics at Kravis Children's Hospital at Mount Sinai, Dr. Barry Love who is also Director of the Congenital Cardiac Catheterization Laboratory at Mount Sinai Hospital. https://doi.org/10.1002/ccd.31002
JACC: Cardiovascular Interventions - Frequency, Predictors, and Clinical Impact of Valvular and Perivalvular Thrombus After Transcatheter Aortic Valve Replacement
Commentary by Dr. Mirza Umair Khalid and Dr. Duk-Woo Park
JACC: Case Reports - HeartBeat: Acute Formation of Thrombus on a Left Atrial Appendage Occlusion Device Immediately After Detachment
In the current episode of HeartBeat, Drs. Edoardo Zancanaro and Indah Sukmawati discuss a case of clot formation on the left atrial surface of the left atrial appendage closure devices with subsequent thromboembolization. In addition, they review LAAC indication, complications, and future perspectives.
Thrombus burden and outcome in patients with COVID-19 presenting with STEMI across the pandemic
Commentary by Dr. Valentin Fuster
Episode 18: Among the topics: Management of left ventricular thrombus - Diagnosis and treatment of HFpEF
ESC TV Today brings you concise analysis from the world's leading experts, so you can stay on top of what's happening in your field quickly. This episode covers: Cardiology This Week: A concise summary of recent studies Management of left ventricular thrombus Diagnosis and treatment of HFpEF – State of the art in 2023 Diagnostics Made Easy: Constriction vs. restriction in echocardiography Host: Rick Grobbee Guests: Glenn Levine and Theresa McDonagh Want to watch that episode? Go to: https://esc365.escardio.org/event/1083 Disclaimer This programme is supported by Siemens Healthineers in the form of an educational grant. The scientific content and opinions expressed in the programme have not been influenced in any way by its sponsor. This programme is intended for health care professionals only and is to be used for educational purposes. The European Society of Cardiology (ESC) does not aim to promote medicinal products nor devices. Any views or opinions expressed are the presenters' own and do not reflect the views of the ESC. Declarations of interests Stephan Achenbach, Rick Grobbee, Nicolle Kraenkel, Glenn Levine and Theresa McDonagh have declared to have no potential conflicts of interest to report. Carlos Aguiar has declared to have potential conflicts of interest to report: personal fees for consultancy and/or speaker fees from Abbott, Alnylam, Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim, Daiichi-Sankyo, Ferrer, Gilead, Lilly, Novartis, Pfizer, Sanofi, Servier, Tecnimede. Davide Capodanno has declared to have potential conflicts of interest to report: Sanofi, Daiichi Sankyo, Terumo, Medtronic, Chiesi. Emma Svennberg has declared to have potential conflicts of interest to report: institutional research grants from Bayer, Bristol-Myers, Squibb-Pfizer, Boehringer- Ingelheim, Johnson & Johnson, Merck Sharp & Dohme.
Light Rounds Volume 3: elderly gentleman with ICMP and LV thrombus
Light Rounds 3: LV thrombus
JACC: Case Reports - HeartBeat: Interventional Removal of LV Thrombus in a Patient With Cardiogenic Shock and Transitory Ischemic Attack
Commentary by Dr. Julia Grapsa, Dr. Edoardo Szancanaro, and Dr. Eric Bates discuss a case from the June 7 issue.
This week our Co-Host and producer is the guest once again! The topic for this week is Pulmonary Embolism, which is a blood clot or thrombus in the lung. A pulmonary embolism (PE) is a sudden blockage in a lung artery. It usually happens when a blood clot breaks loose and travels through the bloodstream to the lungs. PE is a serious condition that can cause: Permanent damage to the lungs Low oxygen levels in your blood Damage to other organs in your body from not getting enough oxygen PE can be life-threatening, especially if a clot is large, or if there are many clots. What causes a pulmonary embolism (PE)? The cause is usually a blood clot in the leg called a deep vein thrombosis that breaks loose and travels through the bloodstream to the lungs. Who is at risk for a pulmonary embolism (PE)? Anyone can get a pulmonary embolism (PE), but certain things can raise your risk of PE: Having surgery, especially joint replacement surgery Certain medical conditions, including Cancers Heart diseases Lung diseases A broken hip or leg bone or other trauma Hormone-based medicines, such as birth control pills or hormone replacement therapy Pregnancy and childbirth. The risk is highest for about six weeks after childbirth. Not moving for long periods, such as being on bed rest, having a cast, or taking a long plane flight Age. Your risk increases as you get older, especially after age 40. Family history and genetics. Certain genetic changes that can increase your risk of blood clots and PE. Obesity What are the symptoms of a pulmonary embolism (PE)? Half the people who have pulmonary embolism have no symptoms. If you do have symptoms, they can include shortness of breath, chest pain or coughing up blood. Symptoms of a blood clot include warmth, swelling, pain, tenderness and redness of the leg. How is a pulmonary embolism (PE) diagnosed? It can be difficult to diagnose PE. To make a diagnosis, your health care provider will: Take your medical history, including asking about your symptoms and risk factors for PE Do a physical exam Run some tests, including various imaging tests and possibly some blood tests What are the treatments for a pulmonary embolism (PE)? If you have PE, you need medical treatment right away. The goal of treatment is to break up clots and help keep other clots from forming. Treatment options include medicines and procedures. Medicines: Anticoagulants, or blood thinners, keep blood clots from getting larger and stop new clots from forming. You might get them as an injection, a pill, or through an I.V. (intravenous). They can cause bleeding, especially if you are taking other medicines that also thin your blood, such as aspirin. Thrombolytics are medicines to dissolve blood clots. You may get them if you have large clots that cause severe symptoms or other serious complications. Thrombolytics can cause sudden bleeding, so they are used if your PE is serious and may be life-threatening. Procedures: Catheter-assisted thrombus removal uses a flexible tube to reach a blood clot in your lung. Your health care provider can insert a tool in the tube to break up the clot or to deliver medicine through the tube. Usually you will get medicine to put you to sleep for this procedure. A vena cava filter may be used in some people who cannot take blood thinners. Your health care provider inserts a filter inside a large vein called the vena cava. The filter catches blood clots before they travel to the lungs, which prevents pulmonary embolism. But the filter does not stop new blood clots from forming. Can pulmonary embolism (PE) be prevented? Preventing new blood clots can prevent PE. Prevention may include: Continuing to take blood thinners. It's also important to get regular checkups with your provider, to make sure that the dosage of your medicines is working to prevent blood clots but not causing bleeding. Heart-healthy lifestyle changes, such as heart-healthy eating, exercise, and, if you smoke, quitting smoking Using compression stockings to prevent deep vein thrombosis (DVT) Moving your legs when sitting for long periods of time (such as on long trips) Moving around as soon as possible after surgery or being confined to a bed (Credits: NIH)
This month on Episode 48 of Discover CircRes, host Cynthia St. Hilaire highlights three original research articles featured in the April 28th issue of Circulation Research. This Episode also includes a discussion between Dr Mina Chung, Dr DeLisa Fairweather and Dr Milka Koupenova, who all contributed to manuscripts to the May 12th Compendium on Covid-19 and the Cardiovascular System. Article highlights: Heijman, et al. Mechanisms of Enhanced SK-Channel Current in AF Chen, et al. IL-37 Attenuates Platelet Activation Enzan, et al. ZBP1 Protects Against Myocardial Inflammation Compendium on Covid-19 and the Cardiovascular System. Cindy St. Hilaire: Hi, and welcome to Discover CircRes, the podcast of the American Heart Association's journal, Circulation Research. I'm your host, Dr Cindy St. Hilaire, from the Vascular Medicine Institute at the University of Pittsburgh. Today, I'm going to be highlighting articles from our April 28th and May 12th issues of Circulation Research. I'm also going to have a chat with Dr Mina Chung, Dr DeLisa Fairweather and Dr Milka Koupenova, who all contributed to articles in the May 12th COVID Compendium. But before we have that interview, let's first talk about some highlights. The first article I want to present is titled Enhanced Calcium-Dependent SK-Channel Gating and Membrane Trafficking in Human Atrial Fibrillation. This article is coming from the University of Essen by Heijman and Zhou, et al. Atrial fibrillation is one of the most common forms of heart arrhythmia in humans and is characterized by irregular, often rapid heartbeats that can cause palpitations, dizziness and extreme fatigue. Atrial fibrillation can increase a person's risk of heart failure, and though treatments exist such as beta blockers, blood thinners and antiarrhythmia medications, they can have limited efficacy and side effects. A new family of drugs in development are those blocking small-conductance calcium-activated potassium channels called SK channels, which exhibit increased activity in animal models of AF and suppression of which attenuates the arrhythmia. In humans however, the relationship between SK channels and atrial fibrillation is less clear, at least in terms of SK channel mRNA levels. Because mRNA might not reflect actual channel activity, this group looked at just that and they found indeed that channel activity was increased in cardiomyocytes from atrial fibrillation patients compared to those from controls even though the mRNA and protein levels themselves were similar. The altered currents were instead due to changes in SK channel trafficking and membrane targeting. By confirming that SK channels play a role in human atrial fibrillation, this work supports the pursuit of SK channel inhibitors as possible new atrial fibrillation treatments. The next article I want to present is titled IL-37 Attenuates Platelet Activation and Thrombosis Through IL-1R8 Pathway. This article comes from Fudan University by Chen and Hong, et al. Thrombus formation followed by the rupture of a coronary plaque is a major pathophysiological step in the development of a myocardial infarction. Understanding the endogenous antithrombotic factors at play could provide insights and opportunities for developing treatments. With this in mind, Chen and Hong, et al. investigated the role of interleukin-1 receptor 8, or IL-1R8, which suppresses platelet aggregation in mice, and of IL-37, a newly discovered human interleukin that forms a complex with IL-1R8 and is found at increased levels in the blood of patients with myocardial infarction. Indeed, the amount of IL-37 in myocardial infarction patients negatively correlates with platelet aggregation. They also show that treatment of human platelets in vitro with IL-37 suppresses the cell's aggregation and does so in a concentration-dependent manner. Moreover, injection of the protein into the veins of mice inhibits thrombus development and better preserves heart function even after myocardial infarction. Such effects were not seen in mice lacking IL-1R8. This suggests IL-37's antithrombotic action depends on its interaction with the receptor. Together, the results suggest IL-37 could be developed as a antithrombotic agent for use in MI patients or indeed perhaps other thrombotic conditions. The last article I want to present before our interview is titled ZBP1 Protects Against Mitochondrial DNA-Induced Myocardial Inflammation in Failing Hearts. This article is coming from Kyushu University and is by Enzan, et al. Myocardial inflammation is a key factor in the pathological progression of heart failure and occurs when damaged mitochondria within the stricken cardiomyocyte release their DNA, triggering an innate inflammatory reaction. In a variety of cells, DNA sensors such as Z-DNA-binding protein 1 or ZBP1 are responsible for such mitochondrial DNA-induced inflammation. In theory then, it's conceivable that therapeutic suppression of ZBP1 might reduce myocardial inflammation in heart failure and preserve function. But as Enzan and colleagues have now discovered to their surprise, mice lacking ZBP1 exhibited worse, not better heart inflammation and more failure after induced myocardial infarction. Indeed, the test animals' hearts had increased infiltration of immune cells, production of inflammatory cytokines and fibrosis together with decreased function compared with the hearts of mice with normal ZBP1 levels. Experiments in rodent cardiomyocytes further confirmed that loss of ZBP1 exacerbated mitochondrial DNA-induced inflammatory cytokine production while overexpression of ZBP1 had the opposite effect. While the reason behind ZBP1's opposing roles in different cells is not yet clear, the finding suggests that boosting ZBP1 activity in the heart might be a strategy for mitigating heart inflammation after infarction. Cindy St. Hilaire: The May 12th issue of Circulation Research is our COVID compendium, which consists of a series of 10 reviews on all angles of COVID-19 as it relates to cardiovascular health and disease. Today, three of the authors of the articles in this series are here with me. Dr Mina Chung is a professor of medicine at the Cleveland Clinic. She and Dr Tamanna Singh and their colleagues wrote the article, A Post Pandemic Enigma: The Cardiovascular Impact of Post-Acute Sequelae of SARS-CoV-2. Dr DeLisa Fairweather, professor of medicine, immunology and clinical and translational science at the Mayo Clinic, and she and her colleagues penned the article, COVID-19 Myocarditis and Pericarditis. Dr Milka Koupenova is an assistant professor of medicine at the UMass Chan School of Medical and she led the group writing the article, Platelets and SARS-CoV-2 During COVID-19: Immunity, Thrombosis, and Beyond. Thank you all for joining me today. DeLisa Fairweather: Thank you so much for having us. Mina Chung: Thank you. Milka Koupenova: Thank you for having us, Cindy. Cindy St. Hilaire: In addition to these three articles, we have another seven that are on all different aspects of COVID. Dr Messinger's group wrote the article, Interaction of COVID-19 With Common Cardiovascular Disorders. Emily Tsai covered cell-specific mechanisms in the heart of COVID-19 patients. Mark Chappell and colleagues wrote about the renin-angiotensin system and sex differences in COVID-19. Michael Bristow covered vaccination-associated myocarditis and myocardial injury. Jow Loacalzo and colleagues covered repurposing drugs for the treatment of COVID-19 and its cardiovascular manifestations. Dr Stephen Holby covered multimodality cardiac imaging in COVID, and Arun Sharma covered microfluidic organ chips in stem cell models in the fight against COVID-19. Cindy St. Hilaire As of today, worldwide, there have been over six hundred million individuals infected with the virus and more than six and a half million have died from COVID-19. In the US, we are about a sixth of all of those deaths. Obviously now we're in 2023, the numbers of individuals getting infected and dying are much, much lower. As my husband read to me this morning, one doctor in Boston was quoted saying, "People are still getting wicked sick." In 75% of deaths, people have had underlying conditions and cardiovascular disease is found in about 60% of all those deaths. In the introduction to the compendium, you mentioned that the remarkable COVID-19 rapid response initiative released by the AHA, which again is the parent organization of Circ Research and this podcast, if I were to guess when that rapid response initiative started, I would've guessed well into the pandemic, but it was actually March 26th, 2020. I know in Pittsburgh, our labs have barely shut down. So how soon after we knew of SARS-CoV-2 and COVID, how soon after that did we know that there were cardiovascular complications? Mina Chung: I think we saw cardiovascular complications happening pretty early. We saw troponin increases very early. It was really amazing what AHA did in terms of this rapid response grant mechanism. You mentioned that the RFA was announced, first of all, putting it together by March 26th when we were just shutting down in March was pretty incredible to get even the RFA out. Then the grants were supposed to be submitted by April 6th and there were 750 grants that were put together and submitted. They were all reviewed within 10 days from 150 volunteer reviewers. The notices were distributed April 23rd, less than a month out. Cindy St. Hilaire: Amazing. Mina Chung: So this is an amazing, you're right, paradigm for grant requests and submissions and reviews. DeLisa Fairweather: For myocarditis, reports of that occurred almost immediately coming out of China, so it was incredibly rapid. Cindy St. Hilaire: Yeah, and that was a perfect lead up to my next question. Was myocarditis, I guess, the first link or the first clue that this was not just going to be a respiratory infection? DeLisa Fairweather: I think myocarditis appearing very early, especially it has a history both of being induced by viruses, but being strongly an autoimmune disease, the combination of both of those, I think, started to hint that something different was going to happen, although a lot of people probably didn't realize the significance of that right away. Cindy St. Hilaire: What other disease states, I guess I'm thinking viruses, but anything, what causes myocarditis and pericarditis normally and how unique is it that we are seeing this as a sequelae of COVID? DeLisa Fairweather: I think it's not surprising that we find it. Viruses around the world are the primary cause of myocarditis, although in South America, it's the parasite Trypanosoma cruzi. Really, many viruses that also we think target mitochondria, including SARS-CoV-2, have an important role in driving myocarditis. Also, we know that SARS-CoV-1 and MERS also reported myocarditis in those previous infections. We knew about it beforehand that they could cause myocarditis. Cindy St. Hilaire: Is it presenting differently in a COVID patient than say those South American patients with the... I forget the name of the organism you said, but does it come quickly or get worse quickly or is it all once you get it, it's the same progression? DeLisa Fairweather: Yeah. That's a good question. Basically, what we find is that no matter what the viral infection is, that myocarditis really appears for signs and symptoms and how we treat it identically and we see that with COVID-19. So that really isn't any different. Cindy St. Hilaire: Another huge observation that we noticed in COVID-19 patients, which was the increased risk of thrombic outcomes in the patients. Dr Koupenova, Milka, you are a world expert in platelets and viruses and so you and your team were leading the writing of that article. My guess is knowing what you know about platelets and viruses, this wasn't so surprising to you, but could you at least tell us the state of the field in terms of what we knew about viruses and platelets before COVID, before Feb 2020? Milka Koupenova: Before Feb 2020, we actually knew that influenza gets inside in platelets. It leads to not directly prothrombotic events, but it would lead to release of complement 3 from them. That complement 3 would actually increase the immunothrombosis by pushing neutrophils to release their DNA, forming aggregates. In cases when you have compromised endothelium and people with underlying conditions, you would expect certain thrombotic outcomes. That, we actually published 2019 and then 2020 hit. The difference between influenza and SARS-CoV-2, they're different viruses. They carry their genome in a different RNA strand. I remember thinking perhaps viruses are getting inside in platelets, but perhaps they do not. So we went through surprising discoveries that it seemed like it is another RNA virus. It also got into platelets. It was a bit hard to tweak things surrounding BSL-3 to tell you if the response was the same. It is still not very clear how much SARS or rather what receptor, particularly when it gets inside would induce an immune response. There are some literature showing the MDA5, but not for sure, may be responsible. But what we found is that once it gets in platelets, it just induces this profound activation of programmed cell death pathways and release of extracellular vesicles and all these prothrombotic, procoagulant form of content that can induce damage around, because platelets are everywhere. So that how it started in 2019 and surprisingly progressed to 2021 or 2020 without the plan of really studying this virus. Cindy St. Hilaire: How similar and how different is what you observe in platelets infected, obviously in the lab, so I know it's not exactly the same, but how similar and how different is it between the flu? Do you know all the differences yet? Milka Koupenova: No offense here, they don't get infected. Cindy St. Hilaire: Okay. Milka Koupenova: Done the proper research. The virus does not impact platelets, but induces the response. Cindy St. Hilaire: Okay. Milka Koupenova: That goes back to sensing mechanism. Thank goodness platelets don't get infected because we would be in a particularly bad situation, but they remove the infectious virus from the plasma from what we can see with function. Cindy St. Hilaire: Got it. So they're helping the cleanup process and in that cleaning up is where the virus within them activates. That is a really complicated mechanism. Milka Koupenova: Oh, they're sensing it in some form to alert the environment. It's hard to say how similar and how different they are unless you study them hint by hint next to each other. All I can tell is that particularly with SARS-C, you definitely see a lot more various kinds of extracellular vesicles coming out of them that you don't see the same way or rather through the same proportion with influenza. But what that means in how platelet activates the immune system with one versus the other, and that goes back to the prothrombotic mechanisms. That is exactly what needs to be studied and that was the call for this COVID compendium is to point out how much we have done as a team. As scientists who put heads together, as Mina said, superfast response, it's an amazing going back and looking at what happened to think of what we achieved. There is so much more, so much more that we do not understand how one contributes to all of these profound responses in the organs themselves, such as myocarditis. We see it's important and that will be the problem that we're dealing from here on trying to figure it out and then long COVID, right? Cindy St. Hilaire: Yeah. Related to what you just said about the mechanism, this cleanup by the platelets or the act of cleaning up helps trigger their activation, is that partly why the antiplatelet and anticoagulant therapies failed in patients? Can you speculate on that? I know the jury's still out and there's a lot of work to be done, but is that part of why those therapies weren't beneficial? Milka Koupenova: The answer to that in my personally biased opinion is yes. Clearly, the antiplatelet therapies couldn't really control the classical activation of a platelet. So what I think we need to do from here on is to look at things that we don't understand that non-classically contribute to the thrombotic response downstream. If we manage to control the immune response in some way or the inflammation of the infection or how a platelet responds to a virus, then perhaps we can ameliorate a little bit of the downstream prothrombotic effect. So it's a lot more for us to trickle down and to understand in my personal opinion. DeLisa Fairweather: There is one thing that was really remarkable to me in hearing your experience, Milka, is that I had developed an autoimmune viral model of myocarditis in mice during my postdoc. So I've been studying that for the last 20 years. What is unique about that model is rather than using an adjuvant, we use a mild viral infection so it doesn't take very much virus at all going to the heart to induce it. I also, more recently, started studying extracellular vesicles really as a therapy, and in doing that, inadvertently found out that actually, the model that I'd created where we passage the virus through the heart to induce this autoimmune model, we were actually injecting extracellular vesicles into the mice and that's what was really driving the disease. This is really brought out. So from early days, I did my postdoc with Dr Noel Rose. If you've heard of him, he came up with the idea of autoimmune disease in the '50s. We had always, in that environment, really believed that viruses were triggering autoimmune disease and yet it took COVID before we could really prove that because no one could identify them. Here we have an example and I think the incidence rates with COVID were so high for myocarditis because for the first time, we had distinguished symptoms of patients going to the doctor right at the beginning of their infection having an actual test to examine the virus, knowing whether it's present or not, whether PCR or antibody test, and then being able to see when myocarditis happened. Cindy St. Hilaire: Yeah. I think one thing we can all appreciate now is just some of the basic biology we've learned on the backend of this. Actually, those last comments really led well to the article that your team led, Dr Chung, about what we call long COVID, which I guess I didn't realize has an actual name, post-acute sequelae of SARS-CoV-2 or PASC is the now more formal name for long COVID. But what is it? We hinted at it that there's these bits about autoimmune and things like that. What counts as long COVID? Mina Chung: Yeah. Our article was led by Tamanna Singh. She did a fantastic job of putting this together. We've had, and others, theorized that the huge palette of symptoms that you can experience post-COVID, they can affect all these organ systems with brain fog, these atypical chest pains, postural orthostatic tachycardia, a lot of palpitations, atrial fibrillation, many weakness and fatigue. To us, really, you can get GI symptoms. We've been very interested in, is this an autoimmune phenomenon directed against nerves and all those things. It's also very interesting because many of the non-COVID syndromes that existed pre-COVID like POTS and chronic fatigue syndrome and a lot of other syndromes are associated with autoantibodies. So that is a very interesting area to explore. Is there a persistence of viral fragments. Is there autoimmunity? Is it also a component of persistence of the damage from the initial infection? So it's an area that still needs a lot of work and a lot of work is going into it, but this is like a post or inter pandemic of itself, so hopefully we'll get more insights into that. Cindy St. Hilaire: Yeah, it's really interesting. I have a friend who has very debilitating long COVID and one of her doctors had said, "If I didn't know any better, I would just describe this as a autoimmune type X." What do we know, I guess, about the current hypothesis of the pathogenesis of PASC? Are there any prevailing theories right now as to why it's occurring? Is the virus still active or is it these domino effects that are leading to multi-organ collapse of some sort? Mina Chung: Yeah. In some people, persistent viral particles can be identified for months, but whether or not that's what's triggering it, it's hard to know. We see more autoimmune disease that's been reported and various antibodies being reported. So those are clearly processes to be investigated. The microthrombosis is still up there in terms of potentially playing a role in long COVID. Milka Koupenova: Mina, you probably know better because you see patients, but to all I have been exposed to, long COVID does not really have a homogeneous symptom presentation and then a few theories as to what may be going on in these patients. Not everybody has a microthrombosis. Not everybody have a D-dimer elevated, but some people do. Some people have, as you pointed out, these spectacularly profound brain fog. People can't function. It's probably your friend, Cindy, right? Cindy St. Hilaire: Yeah. Milka Koupenova: So one of the theories that I have been, from a viral perspective, very interested in is that a lot of the symptoms in certain individuals such as fatigue, brain fog, sensitivity to light and skin can very well be explained by a flare-up of Epstein-Barr virus that may be what SARS-CoV-2 somehow is inducing. I don't know, DeLisa, what your experience with long COVID is as a scientist. I hope only. But I would like to hear your perspective too because it's so heterogeneous and it is amazing what happens. DeLisa Fairweather: I have a very interesting perspective from a number of different directions. One, as I mentioned before, my long history with Dr Rose and I've written many articles theorizing how viruses could cause autoimmune disease. This has grown and really, I think this has been extremely revealing during COVID for many of those theories. One thing that I write about in the review for this article is that mast cells, from all the research I've done with myocarditis in our model, mast cells are central to what is driving everything. We show they're the first innate immune cell acting as an antigen-presenting cell, completely driving the response in a susceptible pattern. One of the things that's very important in autoimmune disease is both sex and race. I'd say one of the big weaknesses we have in myocarditis pre-COVID and post-COVID has been ignoring what's going on with race. In the United States, myocarditis is 90%, 95% white men that are under 50 years of age and most of the cases are under 40 or some of the ones really associated with sudden cardiac death are under 30. So it's very specific. I've been studying sex and race differences and we see those exact differences in our animal models. In animal models, whether you're susceptible or not depends on how many mast cells you have. Well, I've proposed from the beginning, looking, I've written a lot of different sex difference reviews looking at viruses and autoimmune disease with different autoimmune diseases and hypothesizing and really seeing that mast cells do a lot of the things we're talking about. They have all of the receptors, the whole group of them that have been related to SARS-CoV-2 so they can be activated or stimulated by the virus itself. They act as a antigen-presenting cell. They're critical in the complement pathway as well as macrophages. We see the dominant immune phenotype really being macrophages. Mast cells just are usually not counted anywhere. And of course, these receptors, a lot of them have to do with enzymes and things that are all related to mast cells pathways. Then how they activate the immune response and lead it towards the pathway that leads to chronic autoimmune disease with increased autoantibodies in females, mast cells are very different by sex. This has to do also when we talked in the Review about myocarditis and pericarditis. It's both those appearing. Although clinically, we have really boxed them as separate things, because there is some definite clinical pericarditis phenotypes that are different, myocarditis in animal models is always myopericarditis. It always then, in that outer pericardial areas where mast cells sit, they sit around the vascular area in most concentrated. So when they degranulate, we see inflammation coming in the vessel, but really concentrated with fibrosis there and along the pericardium. So that's very typical of what's going on. When we shift anything that shifts that, it changes whether you have more pericarditis or less pericarditis and the vascular inflammation by altering anything that affects the mast cells. I talk a little bit about in the review, I think there's only been a few recent things looking at it in COVID, but I think mast cells and certain susceptibility to autoimmune diseases that occur more often in women can really predispose.We need to pay more attention to mast cells and what they might indicate for all these pathways. Milka Koupenova: I think we should study the platelet mast cell access at this point. DeLisa Fairweather: Yes. Milka Koupenova: Because as you're talking about these sex differences, which is spectacular, these things to me are so mind-boggling how one, the infection itself would be more prevalent in men, but then long COVID is more prevalent in women. All of these things and why we understand so very little, what we found about a few years ago in the Framingham Heart Study in the platelets from those people is that all toll-like receptors are expressed at the higher level in women and they associate with different things between men and female. For instance, toll-like receptors in women will associate more with a prothrombotic response while in male with pro-inflammatory response. I think they grossly underestimate the amount of our sex differences from cell to cell. DeLisa Fairweather: It is, yeah. Mina Chung: One other thing that I learned about the sex differences from this compendium is Mark Chappell also notes, you mentioned TLR and TLR7 and ACE2 are X chromosome in an area that he says escapes X-linked inactivation. So it could very well be involved in further. DeLisa Fairweather: Further, yeah. And ACE2 is expressed more highly in male cells for what's been researched because of the sex difference in COVID, both the COVID infection Cindy St. Hilaire: So a variety of organ systems are impacted in patients with PASC, also referred to as long COVID, the lungs, the heart, the pancreas, the GI system, pretty much any system, the brain, nervous system. We've just been talking about the mast cell impact. I was really thinking in my head, well, the one thing that connects all of it is the vasculature. I'm a vascular biologist, so I have certain biases, I'm sure, but how much of the sequelae that we see is a function of vascular phenotypes? Milka Koupenova: I do think the vasculature is super important. It's clear that not all endothelial cells, for instance, will pick up the virus and respond to it. That's why you have this patchy breakage when you look at autopsies. Hence, platelets will respond according to what's local. That's why you find these micro thrombotic events at certain places. Why does it happen in each organ? How does the virus get to each organ to respond? Or is it just inflammation, but why is it in specific places? That's what we don't understand. That's where we need to go. Perhaps, as DeLisa points out, perhaps it's a lot more complicated than how we traditionally think of thrombosis. Actually, my personal bias, again 100% sure that it is a lot more complicated than the traditional mechanisms that we have understood, and that's where the immune system comes and autoimmunity perhaps stems from and they probably speak to each other, right? It's not just one thing. DeLisa Fairweather: Yeah. I think really, EVs are bringing lots of understanding. A lot of things we used to just think were maybe free-floating and the serum are inside EVs. I think that the immune response is perhaps even more specific than we ever thought and more regulated than we ever understood. When an EV comes through a cardiomyocyte, whether it's from the mitochondria or through a lysosome, is part of what goes into its outer membrane, something that tells the immune system that that came from the heart, so it knows to go. This will solve a lot of our questions with autoimmune disease if it's very specific like that. It doesn't just have to be the release of free-floating cardiac myosin. We know cardiac myosin is the driver of the autoimmune response in myocarditis, but they're probably much more fine-tuned. Cindy St. Hilaire: Yeah. I just would love to end with hearing from each of you. You each have your own domain of specialty. If I gave you a massive pot of money, what would be the question you would want to tackle? What's the gap you would love to answer? Milka Koupenova: We still don't understand specifically what kind of vesicles are coming out, what are their contents in addition to those vesicles. We don't understand. When it comes to platelets, what comes from their granules? We see these breakages of the membrane. Those are non-granule proteins, and non-granule proteins, they serve as dangerous associated molecular pattern signals and can be profoundly inflammatory to the surrounding environment, can be procoagulant. What are those? How are they affecting the surrounding environment? Ultimately, why is there a microthrombi? Why is there not a profound thrombosis everywhere? Thank goodness there isn't, but why isn't? That's what I would do with my money. DeLisa Fairweather: I think I would do something very similar. All of our research in our animal model, on the one side, we are looking in this viral myocarditis animal model and finding the EVs that come from that are driving myocarditis. On the other hand, we're using EVs that come from healthy human plasma or fat, and we're seeing a profound downregulation of everything if you give it early and we're trying to see how late you can give it and still get an effect. So looking at those and really understanding the components in the context of COVID and COVID vaccines to understand those components, I really think that's the future of where we're going to find what's causing disease and also how we can find therapies. They may be able to reverse this. Mina Chung: Yeah, I'm interested very much in the autoimmunity and the autoantibodies that are and how they may react with those microthrombi. Perhaps there's autoantibodies within a lot of that material. We're looking at using human and pluripotent stem cell-derived cell models to study the effects of those. That is what I would use our money for. Cindy St. Hilaire: Well, Dr Mina Chung, Dr DeLisa Fairweather, Dr Milka Koupenova, thank you all so much for joining me today and talking about not only the articles that you wrote and with your colleagues, but also other articles in this amazing compendium. I do think this is one of the first all-encompassing compendiums or group of articles that focus specifically on COVID and cardiovascular disease. So thank you all so much. Mina Chung: Thank you. DeLisa Fairweather: Thank you. Milka Koupenova: You're welcome. Cindy St. Hilaire: That's it for highlights from the April 28th and May 12th issues of Circulation Research. Thank you for listening. Please check out the CircRes Facebook page and follow us on Twitter and Instagram with the handle @circres and #DiscoverCircRes. Thank you to our guests, Dr Mina Chung, Dr DeLisa Fairweather and Dr Milka Koupenova. This podcast is produced by Ishara Ratnayaka, edited by Melissa Stoner and supported by the editorial team of Circulation Research. Some of the copy text for the highlighted articles is provided by Ruth Williams. I'm your host, Dr Cindy St. Hilaire, and this is Discover CircRes, your on-the-go source for the most exciting discoveries in basic cardiovascular research. This program is copyright of the American Heart Association 2023. The opinions expressed by speakers in this podcast are their own and not necessarily those of the editors or of the American Heart Association. For more information, visit ahajournals.org.
Thrombose – Kann mich diese Erkrankung treffen? Welche Folgen hat sie?
Die Thrombose rechtzeitig erkennen Bei der tiefe Beinvenenthrombose (TVT) kommt es zur Thromben- bzw. Gerinnselbildung in einem venösen Gefäß des Beines oder Beckens und sorgt so dafür, dass das venöse Blut dort nicht mehr zum Herzen transportiert werden kann. Es staut sich also vor dem Thrombus und macht in der Folge auch Probleme. Die größte Gefahr einer Thrombose ist allerdings die Lungenembolie. Denn wenn sich der Thrombus aus dem Gefäß löst und Richtung Herzen wandert, kann das Gerinnsel in den Gefäßen der Lunge stecken bleiben. Das kann lebensgefährlich werden. Eine frühzeitige Erkennung einer tiefen Beinenvenenthrombose ist also sehr wichtig. Die Symptome einer TVT Sicherlich kannst du dir vorstellen, dass es, wenn ein Gefäß "praktisch verstopft", zu einem Rückstau von Blut und damit zu einer Schwellung kommen kann. Genau das passiert auch bei einer Thrombose. Das betroffene Bein ist meist geschwollen und schmerzt natürlich auch. Ganz besonders, wenn man das Bein berührt oder auch den Fuß belastet. Häufig fühlt sich das betroffene Bein auch wärmer an und erscheint auch etwas bläulich gefärbt. Leider gibt es aber auch häufig keine so deutlichen Symptome. Deshalb ist der Besuch beim Arzt immer unerlässlich. In der heutigen Podcastfolge erkläre ich dir, - welche Risikofaktoren eine tiefe Beinvenenthrombose begünstigen können, denn einigen davon hast du selbst im Griff. - Außerdem verrate ich dir, wie die Diagnose gestellt wird - und welche Therapiemaßnahmen dann unbedingt erfolgen müssen. - Grundsätzlich kannst du vielen Erkrankungen vorbeugen, so auch hier. Auch darauf gehe ich in der Podcastfolge ein. Ich freue mich auf dich. "Nimm deine Gesundheit wieder selbst in die Hand!" Herzlichst deine Alex ______________________________________________ Hier sind Links, um raus aus dem Hormonchaos zu kommen: Webseite: www.alexbroll.com Kennenlerngespräch: www.alexbroll.com/sprechstunde Youtube: https://bit.ly/2hzB6dl Instagram: https://www.instagram.com/alex_broll/
Pieter Abbeel joins Lexman for a chat about his new paper, "Nihility and Thrombus: A DRAGONESS Perspective." Pieter describes how the flow of blood can be disrupted by notions of nihility, and how this can have serious consequences for patients.
Episode 67: Successful Conservative Management of Aortic Thrombus after Neonatal Arch Repair
Dr. Judith Mathieu (Icahn SOM Mount Sinai Kravis Children's Hospital) and Dr. Raj Sahulee (NYU Grossman SOM Hassenfeld Children's Hospital) discuss an interesting case of aortic thrombus in a neonate after arch repair. Hosted/Edited by: Raj Sahulee, MD. Producer: Deanna Todd Tzanetos, MD, MSCI (U of Louisville SOM Norton Children's Hospital)
Tammy Sparacino's Journal Club #25 — Technical implementation of percutaneous thrombus aspiration using the AngioVac system — Perfusion
Technical implementation of percutaneous thrombus aspiration using the AngioVac system. Hosted by Tammy Sparacino, CCP.
Left Ventricular Thrombus Following Acute Myocardial Infarction: JACC State-of-the-Art Review
Commentary by Dr. Valentin Fuster
VTE Dublin Podcast 66 | Eric Klok | Direct Thrombus Imaging
Welcome back to the VTE Dublin Podcast where you'll find all the recent talks from the VTE Dublin Conference. Be sure to subscribe to the VTE Dublin Podcast Video: Audio:
Join Yvonne Brandenburg, RVT, VTS SAIM and Jordan Porter RVT, LVT, VTS SAIM as we talk about: FATE… the acronym that makes us all cringe and slightly tear up. Feline Arterial Thromboembolism… cold paws that we just want to warm up. Question of the Week Have you ever seen the procedure where they remove the thrombus? Leave a comment at https://imfpp.org/episode98 Resources We Mentioned in the Show Linda Merrill, L. V. (2012). Small Animal Internal Medicine for Veterinary Technicians and Nurses. Ames: Wiley-Blackwell. Feline Aortic Thromboembolism (FATE or Saddle Thrombus). Wendy Brooks, DVM, DABVP. Date Published: 02/27/2012. Date Reviewed/Revised: 11/21/2019. https://veterinarypartner.vin.com/default.aspx?pid=19239&catId=102903&id=5307199. Blood Clots and Aneurysms in Cats. By Suzanne M. Cunningham , DVM, DACVIM (Cardiology), Department of Clinical Sciences, Cummings School of Veterinary Medicine, Tufts University;Kursten V. Roderick , DVM, Tufts University. Last full review/revision Jul 2018 | Content last modified Aug 2018. https://www.merckvetmanual.com/cat-owners/heart-and-blood-vessel-disorders-of-cats/blood-clots-and-aneurysms-in-cats. Thanks so much for tuning in. Join us again next week for another episode! Want to earn some RACE approved CE credits for listening to the podcast? You can earn between 0.5-1.0 hour of RACE approved CE credit for each podcast episode you listen to. Join the Internal Medicine For Vet Techs Membership to earn and keep track of your continuing education hours as you get your learn on! Join now! http://internalmedicineforvettechsmembership.com/ Get Access to the Membership Site for your RACE approved CE certificates Sign up at https://internalmedicineforvettechsmembership.com Get Access to the Technician Treasure Trove Sign up at https://imfpp.org/treasuretrove Thanks for listening! – Yvonne and Jordan
In this episode, we will be discussing Central Lines. We'll try to hit everything about PICC lines, what they are, why we use them, and how to properly maintain them. We will also be discussing the different veins where the central line can be inserted and the risks and complications along with it. Another informational episode for nurses and incoming nurses as we delve into these topics. Go to www.nursingworld.org Sale Ends Sept 6. Use code SUMMERSALE21 at check out. Cup of Nurses: https://fanlink.to/CONsite Frontline Warriors: https://fanlink.to/FWsite Apple https://fanlink.to/Applepodcast Spotify https://fanlink.to/Spotifypodcast Cup of Nurses Store https://fanlink.to/CONshop Frontline Warriors store https://fanlink.to/FWshop Interested in Travel Nursing? https://fanlink.to/TravelNurseNow Free Travel Nursing Guide https://fanlink.to/Travelnursingchecklist Nclex Guide https://fanlink.to/NCLEXguide Cup of Nurses FB Group https://www.facebook.com/groups/cupofnurses Frontline Warriors FB group https://fanlink.to/FWFBgroup 0:03 | A quick word for the sponsors 0:55 | Introduction with the Hosts & Affiliates/Updates 3:09 | Central Lines 3:26 | Central line insertions 8:03 | PICC lines 9:30 | Central line uses 11:31 | Hemodialysis Catheter 14:13 | Tunneled vs non-tunneled catheters 15:22 | Ports 22:14 |Risks and Complications 22:21 | Air embolism 23:56| Infection| 26:30| Phlebitis 28:07| Thrombus formation 29:25| Maintenance 37:30| Closing thoughts
Predictors of Device-Related Thrombus Following Percutaneous Left Atrial Appendage Occlusion
Commentary by Dr. Valentin Fuster
CCFP 105 Topics: Deep Vein Thrombosis
The GenerEhlist - CCFP Exam & Canadian Primary Care Medicine
Written By: Caleb Dusdal Peer Review By: Sarah Donnelly https://thegenerehlist.ca/ccfp-exam-105-topics-podcast/ Objective One: In patients complaining of leg pain and/or swelling, evaluate the likelihood of deep venous thrombosis (DVT) as investigation and treatment should differ according to the risk. Objective Two: In patients with high probability for thrombotic disease (e.g., extensive leg clot, suspected pulmonary embolism) start anticoagulant therapy if tests will be delayed. Objective Three: Identify patients likely to benefit from DVT prophylaxis. Objective Four: Utilize investigations for DVT allowing for their limitations (e.g., Ultrasound and D-dimer). Objective Five: In patients with established DVT, use oral anticoagulation appropriately, (e.g., start promptly, watch for drug interactions, monitor lab values and adjust dose when appropriate, stop warfarin when appropriate, provide patient teaching). Objective Six: Consider the possibility of an underlying coagulopathy in patients with DVT, especially when unexpected. Objective Seven: Use compression stockings in appropriate patients, to prevent and treat post-phlebetic syndrome.
Aujourd'hui j'ai l'honneur de vous proposer le témoignage plein de vie de Morgane, une jeune femme de 40 ans qui a été victime d'un AVC en 2013, à la suite duquel elle a dû se battre pour tout réapprendre. Tout d'abord nous avons évoqué les circonstances de son accident ainsi que sa longue reconstruction physique et psychologique, puis nous avons parlé de son rôle de maman, de lithothérapie, de sophrologie, et de sport aussi ; sans oublier son rôle au sein d'APF France HANDICAP pour constituer des groupes de paroles concernant l'AVC partout en France. Mais je n'en dis pas plus, je vous laisse découvrir ma conversation avec Morgane. Bonne écoute ! Notes de l'épisode : Pour contacter Morgane sur Facebook : https://www.facebook.com/morganesurviver Pour contacter Morgane sur Instagram : https://www.instagram.com/morganem42/ Site web de l'association APF France Handicap : https://www.apf-francehandicap.org Si vous souhaitez donner votre avis, poser une question ou me suggérer un invité vous pouvez me contacter sur le compte Instagram @pepinpodcast Musique originale composée par Not The King-Ice Tea : https://soundcloud.com/coreygagne
Sophia Khattak discusses 'Left main coronary artery thrombus after cannabis consumption: a case report' by Anthony Matta et al.
In this episode, Sophia Khattak discusses key points from a recent case report published in EHJ – Case Reports.
Prevalence of Left Atrial Thrombus in Anticoagulated Patients with Atrial Fibrillation
Commentary by Dr. Valentin Fuster
PERT Podcast: Five Questions with Dr John Moriarty (mostly about clot in transit!)
Episode 7: Our guest, John Moriarty MD FSIR is an interventional radiologist and an Associate Professor at UCLA with appointments in both the Departments of Radiology and Internal Medicine. James Horowitz MD FACC FAHA is a cardiac intensivist and is the director of the Cardiac ICU and NYU Langone Health. Links: Endovascular Removal of Thrombus and Right Heart Masses Using the AngioVac System: Results of 234 Patients from the Prospective, Multicenter Registry of AngioVac Procedures in Detail (RAPID). Moriarty J, et al. JVIR. 2021. PMID: 33526346 https://pubmed.ncbi.nlm.nih.gov/33526346/ The AngioVac system as a bail out option in infective endocarditisStarck CT, et al. Ann Cardiothoracic Surg. 2019. PMID: 31832358 https://pubmed.ncbi.nlm.nih.gov/31832358/ The Role of Percutaneous Vacuum-Assisted Thrombectomy for Intracardiac and Intravascular Pathology Basman C, et al. J of Cardiac Surg. 2018. PMID: 30187515 https://pubmed.ncbi.nlm.nih.gov/30187515 Factors Associated with Successful Thrombus Extraction with the AngioVac Device: An Institutional Experience D'Ayala et al. Annals of Vascular Surgery. 2017. PMID: 27521826 https://pubmed.ncbi.nlm.nih.gov/27521826/ Percutaneous Retrieval of an Embolized Vegetation from Pulmonary Artery After ICD Lead Extraction Bhansal HM et al JACC 2020 Supplement https://www.jacc.org/doi/pdf/10.1016/S0735-1097%2820%2933256-3
Thomas Slater discusses 'Massive pulmonary embolism and thrombus-in-transit via a patent foramen ovale: a case report of successful use of extracorporeal membrane oxygenation to manage post-embolectomy severe right ventricular dysfunction'.
In this episode, Thomas Slater discusses key points from a recent case report by Helen Saunders et al. published in EHJ – Case Reports.
Ep 10: Venous Purgatory: What Are We Unsure Of?
Purgatory is defined as “a place or state of suffering” according to the Oxford dictionary. This month's episode is ‘the podcast with all the questions but not all of the answers' as Steve Elias, MD, and his expert guest panel including Mark Meissner, Raghu Kolluri, Manu Aggarwal and Tom O'Donnell consider the interesting questions in the grey zones of venous disease. Hear them discuss the unknowns around techniques, technology, diagnostics, therapeutics and education in venous disease and how there is so much more to understand in this exciting field of medicine. In this episode they discuss: [02.25] Diagnostic uncertainty [16.25] Thrombus ageing [24.54] Below the groin: treating spider veins [30.45] Saphenous vein reflux [36.54] Ulcer care: healing rates - have we got it all wrong? [44.45] Drugs: prevention and treatment [51.00] Concluding comments Listen now for the latest episode from the veinPODCAST series. Prefer video? View the vodcast video episode here: https://www.radcliffevascular.com/veinvodcast-episode-10 Prefer video? Watch the latest episode via the vodcast video here. Submit your questions/feedback to Steve via: podcast@radcliffe-group.com. Hosted by @DrSteveElias and produced by Radcliffe Vascular. Follow us on social media for the latest updates on the next episode @RadcliffeVASCU today!
Sophia Khattak discusses 'To treat or not to treat: left ventricular thrombus in a patient with cerebral amyloid angiopathy: a case report' by Alexander D Hilt et al.
In this episode, Sophia Khattak discusses key points from a recent case report published in EHJ – Case Reports.
The business of blood clots with Jim Biggins - CEO Access Vascular
Jim Biggins, Founder and CEO, Access Vascular joins me to discuss what it's like to be a start-up in the med device space, commercializing a product and leading his organization pre-COVID, during COVID and into the future.
Dr. Kazuhiko Kido discusses the use of DOACs in patients with LV thrombi. Check out cardioscripts.com for episode references!
High Thrombus Burden in Patients with COVID-19 Presenting with ST-Elevation Myocardial Infarction
Commentary by Dr. Valentin Fuster
20.LES GRANDES ÉTAPES ET LES PIÈGES DE LA NÉPHRECTOMIE POUR THROMBUS CAVE - Pr ARNAUD MEJEAN
Comment préparer son intervention ? Quel bilan préopératoire ?Quels principes pour réaliser une exérèse complète ?Dans quel ordre faire les clampages ? Quels traitements péri-opératoires ?Le Pr Arnaud MEJEAN (Hôpital Européen Georges Pompidou) répond à toutes vos questions !L’orateur n’a pas reçu de rémunération pour la réalisation de cet épisode.Musique du générique : Via AudioNetworkResponsable projet AFUF : Dr Benjamin PradèreProduction : La Toile Sur Ecoute See acast.com/privacy for privacy and opt-out information.
HMP #24 : recensione Thrombus - Mental Turmoil (2018) voto 9/10
Ciao a tutti, oggi vi parlo del gruppo americano di death metal Thrombus e della riedizione del 2018 del suo disco Mental Turmoil via La Caverna Records. In vista del sano death metal d'oltreoceano, bello deviato, ben suonato, ben prodotto e estremamente underground. Solo per palati fini. Buon ascolto ! band : Thrombus album : Mental Turmoil (riedizione del 2018) paese : Stati Uniti stile : death metal label : La caverna Records formazione : Mike Brown - Guitars, vocals / Isamu Sato - Guitars / Karl Fowler - Drums, vocals / Darren Baker - Bass Guitar link : https://lacavernarecs.bandcamp.com/album/mental-turmoil grazie a La Caverna Records per il sostegno ! https://lacavernarecs.bandcamp.com/
JACC: Case Reports - Late Atrial Thrombus Formation After Percutaneous Patent Foramen Ovale Closure
Commentary by Dr. Julia Grapsa
Antithrombotic Therapy for Patients with Left Ventricular Mural Thrombus
Commentary by Dr. Valentin Fuster
JACC: Case Reports - A Dangerous Dilemma: Thrombus in Transit During Pregnancy
JACC: Case Reports - Audio Summary by Dr. Julia Grapsa
Zwei große Studien der Universitätsmedizin Mainz empfehlen neue Strategien im Krankenhaus und belegen die Wirksamkeit und Sicherheit der ambulanten Behandlung In Deutschland erleiden immer mehr Menschen eine akute Lungenembolie. Mehr schwerkranke Patienten könnten von einer frühen Auflösung des Lungenthrombus mit einem Medikament profitieren. Für stabile Patienten, die einen Blutgerinnungshemmer erhalten, kommt eine frühe Entlassung in Betracht. Dies belegen zwei Studien aus dem Centrum für Thrombose und Hämostase (CTH) und dem Zentrum für Kardiologie, Kardiologie I der Universitätsmedizin Mainz. Sie unterstreichen die große Bedeutung des Krankheitsbildes „akute Lungenembolie“ für die Bevölkerung und liefern Hinweise für eine bessere Behandlung. Die beiden Studien wurden in der renommierten kardiologischen Fachzeitschrift „European Heart Journal“ veröffentlicht. Eine akute Lungenembolie entsteht durch ein Blutgerinnsel, das sich zumeist in den Beinvenen bildet und von dort in die Lungenarterien eingeschwemmt wird. Die Patienten leiden an Atemnot und in schweren Fällen kann es zum Herz-Kreislaufversagen kommen. Ziel der Therapie ist es, den Thrombus möglichst schnell aufzulösen und neue Lungenembolien („Rezidive“) zu verhindern. Centrum für Thrombose und Hämostase (CTH) der Universitätsmedizin Mainz Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Keller K, Hobohm L, Ebner M, Kresoja KP, Münzel T, Konstantinides SV, Lankeit M. Eur Heart J. 2019 May 18. pii: ehz236. doi: 10.1093/eurheartj/ehz236. [Epub ahead of print]. PMID: 31102407 Link: https://doi.org/10.1093/eurheartj/ehz236 Weitere Informationen erhalten Sie auf MEDIZIN ASPEKTE
Commentary by Dr. Valentin Fuster
Dr Thomas Craven discusses ‘Post-ischaemic exuberant left ventricular mass: thrombus vs. tumour—case report ' by Paul V Viscuse, David J Bartlett, Thomas A Foley, and Hector I Michelena
In this episode, Dr Thomas Craven discusses key points from a recent case report published in EHJ – Case Reports. For the paper discussed in this episode, please visit https://doi.org/10.1093/ehjcr/yty077.
Commentary by Dr. Valentin Fuster
#dasSMACC - PE with Right Heart Thrombus, Pediatric Cardiology Emergencies, and TEE in Cardiac Arrest
We are in Berlin for #dasSMACC and have lots of pearls to share from the speakers at this amazing conference. Talks will be released for free on the SMACC podcast over the next year, but this podcast holds some pearls that we thought couldn't wait. We cover... Dr. Leanne Harnett on Pulmonary Embolism with Right Heart Thrombus (PE with RHT) Dr. Michele Domico on Pediatric Cardiology Emergencies Dr. Haney Mallemat (@CriticalCareNow) on Transesophageal Echocardiography (TEE) during Cardiac Arrest Thanks for listening! Jeremy Faust and Lauren Westafer
GRAFT reduces potential flow diverter malapposition and occasional acute thrombus formation
In this podcast, Dr Robert Tarr interviews Dr Matthew Gounis and Dr Ajit Puri on their latest study, "Grading of Regional Apposition after Flow-Diverter Treatment (GRAFT): a comparative evaluation of VasoCT and intravascular OCT". GRAFT is a semi-automated image post-processing software, which uses intuitive two-dimensional representations of wall apposition from either high-resolution contrast-enhanced cone-beam CT (VasoCT) or intravascular optical coherence tomography (OCT) images. The technique brings great prospects of reducing stroke-related complications when treating intracranial aneurysms. It delivers quantitative and visually convenient representations of potential flow diverter malapposition and occasional acute thrombus formation. The paper, published on the August 2016 issue of JNIS, can be read here: http://jnis.bmj.com/content/8/8/847.full.
Left Atrial Thrombus on Novel Oral Anticoagulant Therapy
Commentary by Dr. David Wilber
Antikörper als neue Faktoren im immunologischen Prozess der venösen Thrombose
Tierärztliche Fakultät - Digitale Hochschulschriften der LMU - Teil 07/07
Die tiefe Venenthrombose (TVT) entsteht nicht allein durch eine pathologische Blutgerinnung, sondern wird primär durch eine Entzündungsreaktion mit massiver Rekrutierung von Zellen der unspezifischen Immunabwehr ausgelöst. In der vorliegenden Dissertation wurde, mit Hilfe eines etablierten Mausmodells zur Untersuchung der zellulären und molekularen Entstehungsmechanismen der tiefen Venenthrombose (TVT), der Einfluss von Antikörpermolekülen auf die Bildung venöser Thromben untersucht - einer weiteren wichtigen Komponente in immunologischen Prozessen und bekannter Auslöser verschiedener pathologischer Geschehen. Dabei stellte sich heraus, dass Antikörpermoleküle die Entstehung venöser Thromben im Mausmodell beeinflussen: In Mäusen ohne Antikörper war die Thrombusbildung massiv beeinträchtigt und konnte durch Antikörper-Substitution wiederhergestellt werden. Es wurde eine starke Korrelation zwischen IgM-Serumspiegel und Thrombusgewicht sowie eine Beteiligung natürlicher Antikörper festgestellt. Die zugrunde liegenden Mechanismen konnten bereits in Ansätzen aufgeklärt werden: Beteiligte Antikörpermoleküle scheinen an Strukturen des hypoxischen Endothels zu binden und Einfluss zu nehmen auf die initiale Thrombozytenrekrutierung, auf die Leukozytenakkumulation im Thrombus wie auch auf die Fibrinbildung und –stabilisierung. Die gewonnenen Ergebnisse weisen demnach darauf hin, dass bestimmte Antikörpermoleküle in der Lage sind, die Entstehung einer TVT zu begünstigen. Dieses Wissen und eingehendere Forschung kann dazu beitragen, zukünftig neue prognostische Faktoren für das Auftreten venöser Thrombose zu gewinnen und Behandlungsstrategien zu entwickeln, welche die unerwünschten Nebenwirkungen einer alleinigen Hemmung der Blutgerinnung umgehen.
Untersuchungen zur mechanischen Thrombektomie beim Carotis T Verschluss
Tierärztliche Fakultät - Digitale Hochschulschriften der LMU - Teil 07/07
Ein Schlaganfall ist eine plötzlich auftretende Erkrankung des Gehirns, die entweder durch einen Gefäßverschluss oder eine Hirnblutung verursacht wird. Dadurch kommt es zu einer Unterversorgung des Gehirns mit möglichen folgenden Ausfällen der Gehirnfunktionen. Beim Menschen ist der Schlaganfall der vierthäufigste Todesgrund und die häufigste Ursache für Langzeitbehinderung bei Erwachsenen. Akute Carotis T Verschlüsse werden bei konservativer Therapie mit ausgedehnten ischämischen Läsionen, einem schlechten Outcome und bis zu 53 % Mortalität in Verbindung gebracht. Die endovaskuläre mechanische Thrombektomie ist eine vielversprechende alternative Behandlung bei großen Gefäßverschlüssen. Bei dieser Therapiemethode wird versucht, das verschlossene Gefäß mit mechanischen Instrumenten, wie den Stentretrievern, zu rekanalisieren und den Thrombus dabei möglichst restlos zu entfernen. In dieser Arbeit wurden die Daten von 51 Patienten, die aufgrund eines akuten Carotis T Verschlusses mechanisch rekanalisiert wurden, retrospektiv untersucht. Eine erfolgreiche Rekanalisation (TICI 2b/3) wurde bei 78,4 % (40/51) erreicht. Ein gutes klinisches Outcome (mRS 0-2) wurde bei 24,4 % der Patienten beobachtet und auch nur bei denjenigen, die erfolgreich rekanalisiert werden konnten (TICI 2b/3). Mit Stentretrievern wurde eine höhere Rekanalisationsrate und ein besseres klinisches Outcome erzielt als mit anderen mechanischen Instrumenten. Zwölf Patienten (29,3 %) starben während des Beobachtungszeitraums (90 Tage). Klinisch relevante, prozedurbezogene Komplikationen traten bei zwei Patienten auf, eine Gefäßperforation mit einem Mikrodraht und eine symptomatische parenchymale Blutung nach Einleitung einer Antikoagulanztherapie aufgrund eines unbeabsichtigten Ablösens eines Stentretrievers. Ziel der retrospektiven Analyse war es, die Durchführbarkeit, Sicherheit und Effizienz der mechanischen Thrombektomie bei akutem ischämischem Schlaganfall infolge eines Carotis T Verschlusses zu untersuchen. Das Ergebnis war, dass die mechanische Thrombektomie hohe Rekanalisationsraten erzielt, wirksam und, mit einer niedrigen Komplikationsrate, angemessen sicher ist. Eine erfolgreiche Rekanalisation scheint die Voraussetzung für ein gutes klinisches Outcome zu sein.
Dan and Eric talk to author MJ Preston about his new book Acadia Event, and the experiences that inspired it.
Commentary by Dr. Valentin Fuster
Contrast enhanced transesophageal echocardiography in patients with atrial fibrillation referred to electrical cardioversion improves atrial thrombus detection and may reduce associated thromboembolic events
Aims: Transesophageal echocardiography (TEE) is the gold standard for the detection of thrombi in patients with atrial fibrillation (AF) before undergoing early electrical cardioversion (CV). However, TEE generates inconclusive results in a considerable number of patients. This study investigated the influence of contrast enhancement on interpretability of TEE for the detection of left atrial (LA) thrombi compared to conventional TEE and assessed, whether there are differences in the rate of thromboembolic events after electrical cardioversion. Methods: Of 180 patients with AF (51 females, 65.2 +/- 13 years) who were referred to CV, 90 were examined with native imaging and contrast enhancement within the same examination (group 1), and 90 were examined with native TEE alone and served as control (group 2). Cineloops of the multiplane examination of the LA and LA appendage (LAA) were stored digitally before and, in group 1, after intravenous bolus application of a transpulmonary contrast agent. Images of group 1 were assessed offline and the diagnosis of LA thrombi was made semi-quantitatively: 1= thrombus present; 2=inconclusive result; 3=no thrombus. The presence of spontaneous echocontrast (SEC) was registered and flow velocity in the LA appendage (LAA-flow) was measured. All patients in whom CV was performed were followed up for 1 year or until relapse of AF. CV related adverse events were defined as any thromboembolic event within 1 week after CV. Results: No serious adverse events occurred during TEE and contrast enhanced imaging. In group 1 atrial thrombi were diagnosed in 14 (15.6%) during native and in 10 (11.1%) patients during contrast enhanced imaging (p
Conservative treatment of a left atrial intramural hematoma after left atrial thrombus resection and concomitant mitral valve replacement - case report
Left atrial intramural hematoma is a seldom cause of left atrial mass. It has been described to occur spontaneously, after interventional procedures, after blunt chest trauma, or after aortocoronary bypass surgery. We present a case of mitral valve replacement together with the removal of a large intraatrial space-occupying lesion. Intraoperative transesophageal echocardiography confirmed a successful resection of this mass. Surprisingly, upon admission to ICU, transesophageal and transthoracic echocardiography revealed a recurrence of an intramural lesion, closest matching a hematoma, which was confirmed by contrast-enhanced computed tomography. Surgical intervention was thoroughly discussed but a conservative management was favoured. 3 months after surgery, a reassessed transthoracic echocardiography and computed tomography demonstrated an almost complete resolution of the pre-existing hematoma.
Aktivierung von Thrombozyten durch humane atherosklerotische Plaques: Mechanismen und Inhibition
Medizinische Fakultät - Digitale Hochschulschriften der LMU - Teil 09/19
Atheromatöse Plaques sind vulnerabel, und deren Ruptur kann die Bildung gefäßverschließender plättchen- und fibrinreicher Thromben induzieren, welche akute Myokardinfarkte und ischämische Schlaganfälle verursachen können. Bisher geht man davon aus, dass der Plaque-„tissue factor“ als Aktivator der extrinsischen Blutgerinnung und Stimulator der Thrombin-vermittelten Plättchenaktivierung und Aggregation die bedeutendste prothrombogene Substanz atheromatöser Läsionen darstellt. Zu Beginn dieser Arbeit war nicht geklärt, ob und wie das lipidreiche atherosklerotische Plaquematerial auch direkt mit den Thrombozyten im Blut interagieren und auf diese Weise die Bildung eines gefäßverschließenden Plättchenthrombus induzieren kann. Die atheromatösen Läsionen von mehr als 60 verschiedenen Patienten mit Karotisstenose wurden mittels Endarterektomie isoliert und Kollagen Typ I- und Kollagen Typ III-positive, morphologisch äußerst heterogene Strukturen in den Plaques identifiziert, welche direkt die Adhäsion, Sekretion und Aggregation von Plättchen in Puffer, Plasma und Blut stimulierten. Darüber hinaus lösten die Plaques auch die Bildung von Thrombozyten-Monozyten-Aggregaten sowie eine plättchenbeschleunigte Fibrinbildung und Gerinnung aus. Unter arteriellen Flussbedingungen induzierten die kollagenpositiven Komponenten des Plaquematerials die Adhäsion, das Ausbreiten und die Aggregatbildung der Thrombozyten. Die Plaque-stimulierte Plättchenaggregatbildung erfolgte sehr rasch (< 5 min) und wurde in Hirudin-antikoaguliertem Blut beobachtet, was darauf schließen lässt, dass diese direkt und unabhängig von der Plaque-„tissue factor“-vermittelten Koagulation erfolgte und sehr wahrscheinlich für die initiale und schnelle Thrombusbildung nach einer Plaqueruptur in vivo von Bedeutung ist. Sowohl die Ergebnisse mit humanen, als auch mit murinen Blutplättchen wiesen auf eine essentielle Rolle morphologisch diverser Kollagen Typ I- und Kollagen Typ III-positiver Plaquestrukturen und des thrombozytären Kollagenrezeptors GPVI bei der durch atheromatöse Läsionen stimulierten Plättchenformveränderung, Adhäsion, Ausbreitung, Sekretion und Aggregation im statischen System und unter arteriellen Flussbedingungen hin. Der zweite bedeutende thrombozytäre Kollagenrezeptor, das Integrin α2β1, schien hingegen nicht an der durch die atheromatösen Läsionen hervorgerufenen Plättchenadhäsion und Aggregation im statischen System und unter Fluss beteiligt zu sein. Diese Beobachtungen führten zur Annahme, dass die Verabreichung von z. B. spezifischen anti-GPVI-Antikörpern oder löslichem GPVI-Protein, welche die Interaktion des thrombozytären GPVI-Rezeptors mit dessen Liganden im Plaquegewebe (Kollagen Typ I/Typ III) inhibieren, viel versprechende neue und effektive antithrombotische Strategien zur frühen Prävention kardio- und cerebrovaskulärer Gefäßverschlüsse darstellen könnten. Der thrombozytäre VWF-Rezeptor GPIbα war weder im gerührten System, noch unter Fluss mit niedrigeren Scherraten von 500 s-1 von Bedeutung für die durch atheromatöse Plaques induzierte Plättchenaggregation im Blut. Unter arteriellen Flussbedingungen mit höheren Scherraten von 1500 s-1 allerdings resultierte die Blockade von GPIbα in einer starken Reduktion (77±5%) der Plaque-stimulierten Thrombozytenadhäsion und Aggregatbildung. Dies lässt darauf schließen, dass unter diesen Strömungebedingungen auch die Interaktion des VWF mit dem Plättchen-GPIbα-Rezeptor eine wichtige Rolle für die Thrombusbildung nach Plaqueruptur spielt. Sowohl die ADP-Rezeptor-Antagonisten MRS2179 (P2Y1-Antagonist) und AR-C69931MX (P2Y12-Antagonist), als auch Aspirin® konnten die Plaque-vermittelte Thrombozytenaggregation in gerührtem PRP und Blut signifikant verringern, wobei die Kombination aller drei Plättchenhemmer am effektivsten wirkte und die Plaque-induzierte Aggregation vollständig inhibierte. Unter arteriellem Fluss (Scherraten: 1500 s-1) wirkten MRS1279, AR-C69931MX sowie deren Kombination allerdings deutlich weniger effizient als im statischen System und reduzierten die Plaque-stimulierte Plättchenaggregatbildung nur um 35±14%, 32±13% und 58±12%. Überraschender Weise führte die Zugabe von Aspirin® unter Fluss zu keiner signifikanten Reduktion der Plaque-induzierten Thrombozytenaggregatbildung. Diese Ergebnisse lassen vermuten, dass ADP-Rezeptor-Antagonisten sowie Aspirin® die Bildung eines gefäßverschließenden Thrombus nach Plaqueruptur eher ineffizient hemmen dürften. Die atheromatösen Plaquehomogenate verschiedener Patienten wiesen unterschiedliche thrombozytenaktivierende Eigenschaften auf, welche weder auf deren variierenden Gehalt an löslichem Kollagen, noch auf die unterschiedliche Morphologie der Kollagen Typ I- und Kollagen Typ III-positiven Plaquekomponenten zurückgeführt werden konnte. Weiterhin verhielt sich sowohl fibrilläres als auch lösliches Kollagen Typ I und Kollagen Typ III anders als das Plaquematerial bezüglich der Plättchenaggregation im PRP. Die Bindung des thrombozytären GPVI-Rezeptors an das Plaquematerial stellte die Voraussetzung für die Plättchenaktivierung der Plaques dar, wobei jedoch keine eindeutige positive Korrelation zwischen der GPVI-Bindung und der Aktivität der atheromatösen Läsionen verschiedener Patienten hergestellt werden konnte. Der Grund für die unterschiedliche Thrombozytenaktivierung induziert durch das Plaquematerial verschiedener Patienten bleibt letztlich also unklar. Die weitere Erforschung möglicher Ursachen für die unterschiedlichen plättchenaktivierenden Eigenschaften der lipidreichen atheromatösen Läsionen verschiedener Patienten stellt eine interessante und vor allem klinisch relevante zukünftige Fragestellung dar.
Einfluß einer postischämischen Hypothermie auf die Basalmembran bei der experimentellen zerebralen Ischämie mit Reperfusion
Medizinische Fakultät - Digitale Hochschulschriften der LMU - Teil 05/19
Experimentelle Untersuchungen konnten zeigen, dass es beim Schlaganfall in der Reperfusionsphase zu einer Schädigung der Basalmembran und zu einem Zusammenbruch der mikrovaskulären Integrität kommt. Dies kann zu einer intrazerebralen Hämorrhagie mit zusätzlichen neurologischen Schäden führen. Die systemische Thrombolyse mit rekombinantem Gewebe-Plasminogen-Aktivator (rt-PA) zielt auf die Fibrinolyse des Thrombus, der das Hirngefäß verschließt, um den zerebralen Blutfluß wiederherzustellen und den Infarkt zu verkleinern. Jedoch haben klinische Studien gezeigt, dass die Thrombolyse die Gefahr einer intrazerebralen Blutung steigert. Klinische und experimentelle Untersuchungen haben gezeigt, dass eine postischämische Hypothermie das Infarktvolumen verkleinern kann. Der postulierte Wirkungsmechanismus einer Hypothermie ist die Verminderung der Aktivität unspezifischer und spezifischer proteolytischer Systeme (z.B. endogene Plasminogenaktivatoren (u-PA und t-PA) oder die Matrix-Metallo-Proteinasen MMP-2 und MMP-9). Ziel dieser Arbeit war es, den Einfluß einer postischämischen Hypothermie auf die Basalmembran der Hirngefäße nach einer zerebralen Ischämie mit Reperfusion zu untersuchen und mögliche Schädigungsmechanismen darzulegen. Hierzu wurde bei narkotisierten, beatmeten Ratten eine 3-stündige transiente fokale zerebrale Ischämie mit 24-stündiger Reperfusion erzeugt. Postischämisch wurde durch extrakorporale Kühlung eine 24-stündige milde bis moderate Hypothermie erzeugt und mittels Temperatursonde ständig gemessen und überwacht. Nach Beendigung des Versuches wurden die Hirne entnommen und einer volumetrischen, immunohistochemischen und biochemischen Aufarbeitung und Auswertung zugeführt. Es konnte gezeigt werden, dass eine postischämische Hypothermie die Degradation der Basalmembran zum großen Teil verhindert und die Infarktgröße signifikant reduziert. Gleichzeitig kommt es durch diesen strukturellen Erhalt der Basalmembran zu einem funktionellen Erhalt der Integrität und zu einer Verminderung der Extravasation von korpuskulären und nichtkorpuskulären Blutbestandteilen. Zusätzlich konnte eine mögliche Ursache für die Degradation der Basalmembran und den Verlust der mikrovaskulären Integrität aufgezeigt werden. Die postischämische Hypothermiebehandlung verhinderte die Steigerung der Aktivität der Plasminogen-Aktivatoren u-PA und t-PA und der Matrix-Metallo-Proteinasen MMP-2 und MMP-9. Wir schließen aus den vorliegenden Untersuchungen, dass eine postischämische Hypothermie das Risiko des Auftretens einer Hämorrhagie als gefürchtete Komplikation nach einer zerebralen Ischämie senken kann. Dies gewinnt zusätzlich an Bedeutung, da die therapeutische Anwendung der systemischen Thrombolyse die Gefahr des Auftretens einer Hämorrhagie steigert. Eine systemische Thrombolyse in Kombination mit einer Hypothermie wäre eine mögliche Therapieoption, um die Gefahr des Auftretens einer intrazerebralen Blutung zu vermindern. Der genaue Pathomechanismus ist jedoch nach derzeitigem Kenntnisstand unklar. Deshalb sind vor der Anwendung beim Menschen noch weitere experimentelle und klinische Studien notwendig.
Einfluss des Gαq-Proteins auf die myokardiale Infarktgröße der knochenmarktransplantierten Gαq-Knockout-Maus im Ischämie/Reperfusionsmodell
Tierärztliche Fakultät - Digitale Hochschulschriften der LMU - Teil 02/07
Influence of the Gαq-protein on myocardial infarct size of the bone marrow-engrafted Gαq-knockout-mouse in a ischemia/reperfusion-model Platelets play a key role in the pathogenesis of an acute myocardial infarction. Thrombus formation, which is mediated by the activation of platelets, results in the occlusion of the coronary artery. On the other hand, agglutinated platelets in the small myocardial vessels impair the myocardial microcirculation. Due to their pro-inflammatory effects, platelets also contribute to the pathogenesis of ischemia/reperfusion injury. The myocardium of Gαq-deficient mice showed a reduced susceptibility to ischemia and reperfusion compared to that of wild-type mice (HEUER, in preparation). Activation of platelets lacking the Gαq-protein is markedly impaired, resulting not only in an increased haemophilia but also in a decreased thrombophilia of Gαq-deficient mice. A bone marrow transplantation was performed to investigate whether the impaired platelet-activation is responsible for the reduced susceptibility of Gαq-deficient mice to ischemia/reperfusion injury. Wild-type mice were lethally irradiated to facilitate the engraftment of bone marrow cells of Gαq-deficient mice and vice versa. A reconstitution phase of at least 90 days for both groups guaranteed, that blood of wild-type mice contained normal levels of Gαq-deleted platelets, while blood of Gαq- deficient mice contained only wild-type platelets. Afterwards, according to the study of HEUER (in preparation), myocardial ischemia was artificially induced by surgically ligating the left coronary artery for 30 minutes and was followed by a reperfusion phase of 24 hours. Heart function of both groups was examined by echocardiography before and after surgery. After euthanasia the size of infarction-area to area at risk (I/AAR) and infarction-area to left ventricle (I/LV) in the stained hearts was determined by planimetry. As a result neither the cardioechography (relative difference of fractional shortening prae and post op: 17, 1 % ± 2,9 % (SEM) versus 10,8 % ± 4,0 % (SEM)) nor the infarct-sizes (I/AAR: 18,2 % ± 4,2 % (SEM) versus 10,0 % ± 3,7 % (SEM); I/LV: 9,5 % ± 2,7 % (SEM) versus 5,6 % ± 2,2 % (SEM)) showed any significant differences between the two groups. In conclusion it could be assumed, that the impaired platelet-activation is not the only reason for the different susceptibility of wild-type and Gαq-deficient mice to ischemia/reperfusion injury; in fact, the reduced susceptibility of Gαq-deficient mice seems to be a result of both - their impaired platelet-activation and unknown protecting effects based on the absence of the Gαq-protein in other cells such as cardiomyocytes.
Erste Erfahrungen mit früher und später Stentimplantation bei Myokardinfarkt im Zeitraum von August 1992 bis April 1998 an dem Klinikum Innenstadt der Ludwigs-Maximilians-Universität München mit Ausblick auf die aktuelle Situation der Stentimplantation be
Medizinische Fakultät - Digitale Hochschulschriften der LMU - Teil 03/19
Die vorliegende Arbeit belegt, dass bei etwa 90% TIMI 3 Fluss nach Stentimplantation mit hoher Sicherheit erzielt werden konnte und dies vor allem in der Gruppe < 24 Stunden mit höherem Anteil an Thrombus und Gefäßokklusion als in der Gruppe ³ 24 Stunden bei überwiegend komplexen Läsionscharakteristika Typ B2 und C. Es zeigte sich in der Angiographie ein geringer Stenosegrad nach Intervention. Und ebenso verzeichnete man auch eine niedrige Rate an Revaskularisierungsmaßnahmen. Aufgrund einer hohen Offenheitsrate des Infarktgefäßes und eine niedrige Revaskularisierungsrate, konnte man die Indikation zur PTCA und Stentimplantation nach Myokardinfarkt am Klinikum Innenstadt München, bei bestehender klinischer Symptomatik, durchaus auch bei später Implantation diskutieren. Unter Berücksichtigung des verhältnismäßig großen Anteils an Risikopatienten in dieser Gruppe, war die Infarktsterblichkeit im Rahmen vergleichbarer Studien. Die Patientengruppe profitierte von einer guten Offenheitsrate des entsprechenden Infarktgefäßes. Die ischämischen Komplikationen blieben im Rahmen vergleichbarer Studien. Die Komplikationsrate war insgesamt mit entsprechenden Studien vergleichbar. Bei den Studien bis März 2003 zeigt sich bei Patienten im akuten Myokardinfarkt sowie im kardiogenen Schock als auch bei Rescue PTCA ein Vorteil der Stentimplantation mit Abciximab gegenüber alleiniger Stentimplantation.
Das aortopulmonale Shuntmodell am Schwein - Untersuchung zur Hämodynamik und zum Endothelin-1-Plasmaspiegel
Tierärztliche Fakultät - Digitale Hochschulschriften der LMU - Teil 01/07
Vorliegende Studie befasst sich mit den hämodynamischen Veränderungen sowie den Veränderungen des Endothelin-1 (ET-1) Plasmaspiegels am aortopulmonalen Shuntmodell beim Schwein. Hierzu werden in Vorversuchen die akuten hämodynamischen Veränderungen, wie sie nach Shuntimplantation auftreten, an Ferkeln im Alter von 3 bis 8 Wochen erfasst. Dabei ist ein signifikanter Abfall des mAoP sowie ein signifikanter Anstieg des mPAP, sowie PVR bei nahezu gleichbleibendem pulmonalarteriellem Fluss zu verzeichnen. Schließlich wird an 12 Absatzferkeln im Alter von durchschnittlich 32 Tagen wie auch schon bei der Vorversuchsgruppe ein aortopulmonaler Shunt mit einem Durchmesser von 6 mm und einer Länge von ca. 2 cm unter Propofolnarkose implantiert. Dabei werden vor Shuntimplantation die Basalwerte der Hämodynamik sowie des ET-1-Plasmaspiegels erfasst. Nach Shuntimplantation kommt es zu einem signifikanten Anstieg des ET-1, der sich bis zum Ende der Operation weiter erhöht. Die postoperative Mortalität der Shuntgruppe liegt bei 50%. Von diesen sterben 2 Schweine bereits wenige Stunden nach dem Eingriff an akutem Lungenödem. Der weitere Versuchsverlauf erstreckt sich über 5 Wochen. In die Kontrollgruppe gehen 4 Tiere in die Endauswertung ein, in die Shuntgruppe 6 Tiere. Bei 5 Shuntschweinen ist nach 5 Wochen der Shunt mit einem organisierten Thrombus verschlossen, lediglich bei einem Schwein ist der Shunt durchgängig. Deutliche hämodynamische Unterschiede von der Shunt- zur Kontrollgruppe bestehen zur Finalmessung im pulmonalarteriellen sowie rechtsventrikulären Druck. Die ET-1-Plasmakonzentration der Shuntgruppe ist im Vergleich zum Ausgangswert immer noch erhöht, jedoch nicht signifikant unterschiedlich zur Kontrollgruppe. In Lungenbiopsien zeigen sich nach 5 Wochen in der Shuntgruppe Parenchymverdichtungen, beim Shuntschwein mit offenem Shunt zusätzlich perivaskuläre Ödeme und Entzündungsreaktionen sowie Gefäßthromben. Zusammenfassend lässt sich sagen, dass das aortopulmonale Shuntmodell am Schwein dienliche Hinweise bezüglich der ET-1-Ausschüttung aus Endothelzellen bei erhöhtem Fluss liefert, sich jedoch wegen der Neigung zur Thrombenbildung im Shunt nicht zum Langzeitversuch eignet.
Plättchenassoziierter Tissue Factor als schnell aktivierbarer, intravaskulärer Starter des menschlichen Gerinnungssystems
Medizinische Fakultät - Digitale Hochschulschriften der LMU - Teil 02/19
Der Tissue Factor (TF) der Gefäßwand gilt heute als der wichtigste Starter der menschlichen Blutgerinnung. Es wird davon ausgegangen, dass die Lokalisation von TF innerhalb der Gefäßwand unter physiologischen Verhältnissen eine strikte Trennung von den plasmatischen Gerinnungsfaktoren gewährleistet, so dass es unter physiologischen Bedingungen nur nach Wegfallen der endothelialen Barriere zur Bildung des TF/VIIa-Komplexes und dort zur Auslösung der Blutgerinnung kommt. Nach der bisherigen Lehrmeinung stellen Monozyten die einzigen bekannten Blutzellen dar, die nach Langzeitstimulationsbedingungen in der Lage sind, TF zu synthetisieren und zu exprimieren. Der monozytäre TF spielt vor allem bei der Pathogenese der Sepsis und der damit assoziierten Disseminierten Intravasalen Gerinnung (DIC) eine wichtige Rolle. In der vorliegenden Arbeit zeigte sich, dass TF bereits nach einer fünf minütigen Stimulation von Vollblut mit fibrillärem Kollagen in Monozyten-Plättchen-Komplexen und Neutrophilen-Plättchen-Komplexen gemessen wurde. Die TF Präsentation in den Leukozyten-Plättchen-Komplexen war streng abhängig von der vorhandenen Plättchenzahl. Mit Hilfe von Vollblutgerinnungsmodellen und prokoagulatorischen Assays konnte gezeigt werden, dass der schnell präsentierte Tissue Factor funktionell aktiv war und somit die Fibrinbildung auslöste. Elektronenmikroskopische Aufnahmen zeigten, dass das TF Antigen auf der Oberfläche von Plättchen vorhanden war, die sich in Konjugaten mit Leukozyten befanden. Um die Frage nach dem Ursprung dieses intravaskulären TF zu klären, wurden Monozyten, Neutrophile Granulozyten und Plättchen auf ihren Gehalt an TF Protein mit einem Double-Sandwich-ELISA untersucht. Dabei konnte nur in den Plättchen TF Antigen nachgewiesen werden. Weitergehende Untersuchungen zeigten, dass TF in der Tat in den a-Granula und dem „open cannanicular system“ der Plättchen lokalisiert ist. In den Plättchen und in deren Vorläuferzellen war keine m-RNA für TF vorhanden. So bleibt die letztendliche Quelle des intravaskulären TF bis auf weiteres ungeklärt. Durch Hemmung von Adhäsionsproteinen, die die Interaktion von Plättchen mit Leukozyten vermitteln, wie P-Selektin und CD40L, konnte die TF-Präsentation in den Plättchen-Leukozyten-Komplexen inhibiert werden. Daher ist davon auszugehen, dass mehrere Adhäsionsproteine an dem Prozess der Präsentation von intravaskulärem TF beteiligt sind. Ein aus den Ergebnissen der vorliegenden Arbeit abgeleitetes Modell der Aktivierung des intravaskulären TF geht davon aus, dass in dem zwischen Leukozyten und Plättchen entstandenen Microenvironment ein von dem Plasma weitgehend unabhängiger Raum entsteht. In diesem Microenvironment wird möglicherweise der von den aktivierten Plättchen sezernierte TFPI durch die leukozytenassoziierte Elastase sowie weitere Proteasen und reaktive Sauerstoffspezies inaktiviert. TF kann damit zusammen mit FVIIa und FXa die Gerinnung starten. Die Ergebnisse lassen vermuten, dass die gesamte Blutgerinnung auf der Oberfläche von Plättchen stattfinden kann. Der intravaskuläre TF spielt vermutlicherweise eine Rolle bei der Aufrechterhaltung der Gerinnung innerhalb des lumenwärts wachsenden Thrombus. Somit kann die Fibrinbildung gezielt dort aktiviert werden, wo sie benötigt wird, um den Thrombus zu stabilisieren. Das Vorhandensein eines schnell aktivierbaren, intra-vaskulären Tissue Factor Systems stellt ein neues Konzept dar, um sowohl den physiologischen als auch den pathologischen Gerinnungsstart besser zu verstehen.













































