Podcasts about Neisseria
- 59PODCASTS
- 94EPISODES
- 25mAVG DURATION
- 1MONTHLY NEW EPISODE
- Nov 25, 2025LATEST
POPULARITY
Best podcasts about Neisseria
Latest news about Neisseria
- We live in the luckiest timeline LessWrong - Nov 12, 2025
- WHO warns of widespread resistance to common antibiotics worldwide News (English) - World Health Organization - Oct 13, 2025
- Neonatal Gonococcal Conjunctivitis Caused by Fluoroquinolone-Resistant Neisseria gonorrhoeae Emerging Infectious Diseases Journal - Sep 18, 2025
- Outbreak of Neisseria meningitidis Conjunctivitis in Military Trainees - Texas, February-May 2025 Morbidity and Mortality Weekly Report (MMWR) - Sep 4, 2025
- AI has produced 2 new antibiotics to kill ‘superbugs’. It’s promising – but we shouldn’t get too excited yet Health – The Conversation - Aug 19, 2025
- Researchers say they used generative AI algorithms to design novel antibiotics targeting drug-resistant Neisseria gonorrhoeae and MRSA (Anne Trafton/MIT News) Techmeme - Aug 15, 2025
- Researchers say they used generative AI algorithms to design novel antibiotics targeting drug-resistant Neisseria gonorrhoeae and MRSA BizToc - Aug 15, 2025
- Artificial intelligence enables discovery of novel compounds to fight drug-resistant bacteria The Medical News - Aug 14, 2025
- Using generative AI, researchers design compounds that can kill drug-resistant bacteria OODA Loop - Aug 14, 2025
- Condoms, PrEP and vaccines: how the UK is expanding STI prevention English – The Conversation - Aug 12, 2025
Latest podcast episodes about Neisseria
On episode #94 of the Infectious Disease Puscast, Daniel and Sara review the infectious disease literature for the weeks of 11/11/25 – 11/19/25. Host: Daniel Griffin and Sara Dong Subscribe (free): Apple Podcasts, RSS, email Become a patron of Puscast! Links for this episode Viral Epstein-Barr virus reprograms autoreactive B cells as antigen-presenting cells in systemic lupus erythematosus (Science Translational Medicine) Hepatitis B reactivation following switch away from tenofovir-containing anti-retroviral therapy in people living with HIV: A case series and lessons for practice (CID) Antimicrobial drug-resistant Neisseria gonorrhoeae (GC) infections in men using doxycycline postexposure prophylaxis. A substudy of the ANRS 174 DOXYVAC trial (CID) HIV Pre-exposure Prophylaxis Does Not Increase Gonorrhea and Chlamydia Incidence in Young Black and Hispanic Men who Have Sex With Men: An Observational Cohort Study (OFID) Bacterial Global and regional knowledge of antibiotic use and resistance among the general public: a systematic review and meta-analysis (CMI: Clinical Microbiology and Infection) Infant Botulism Outbreak Linked to Infant Formula, November 2025 (CDC: Botulism) Outbreak Investigation of Infant Botulism: Infant Formula (November 2025) (FDA) Vitamin D deficiency at hospital admission with community-acquired pneumonia is associated with increased risk of mortality: A Prospective Cohort Study (OFID) Bat-Associated Hemotropic Mycoplasmas in Immunosuppressed Children, Spain, 2024 (Emerging Infectious Diseases) A Multicomponent Intervention to Improve Maternal Infection Outcomes (NEJM) Fungal The Last of US Season 2 (YouTube) Increasing Fluconazole Resistance in Candida parapsilosis: A 10-Year Analysis of Blood Culture Isolates at a US Reference Laboratory (2015–2024) (JID) British Society for Medical Mycology best practice recommendations for the diagnosis of serious fungal diseases: 2025 update (LANCET: Infectious Diseases) In Vivo Evolution of Candida auris Multidrug Resistance in a Patient Receiving Antifungal Treatment (JID) Parasitic Implications of a fatal anaphylactic reaction occurring 4 hours after eating beef in a young man with IgE antibodies to galactose-α-1,3-galactose (JACI: Journal of Allergy and Clinical Immunology In practice) WHO recommends R21/Matrix-M vaccine for malaria prevention in updated advice on immunization (WHO) Effectiveness of the RTS,S/AS01E malaria vaccine in a real-world setting over 1 year of follow-up after the three-dose primary schedule: an interim analysis of a phase 4 study in Ghana, Kenya, and Malawi (LANCET: Global Health) A systematic review and an individual patient data meta-analysis of ivermectin use in children weighing less than fifteen kilograms: Is it time to reconsider the current contraindication? (PLoS Neglected Tropical Diseases) Miscellaneous IL12RB1 deficiency appearing in North America: expanding the clinical phenotypes (CID) Music is by Ronald Jenkees Information on this podcast should not be considered as medical advice.
Antimicrobial resistance (AMR) continues to grow as a global health threat, making infections harder to treat and leaving fewer options for patients. The need for new antibiotics is an urgent matter — but traditional discovery methods are slow and limited. In this episode of Let's Talk Micro, Luis is joined by Dr. James Collins, professor at MIT and researcher at the Broad Institute, who is leading efforts to apply AI to antibiotic discovery. We discuss how his team used deep learning to uncover promising new compounds, including NG1 and DN1, which showed activity against drug-resistant Neisseria gonorrhoeae and Staphylococcus aureus. We also talk about the challenges of bringing discoveries from computer models to the clinic, and what this approach could mean for the future of the fight against superbugs. Link to study: https://www.cell.com/cell/abstract/S0092-8674%2825%2900855-4 Check out the website: https://www.letstalkmicro.com/ Questions? Feedback? Send those to letstalkmicro@outlook.com Want to support the podcast? Here's how: Venmo: https://venmo.com/u/letstalkmicro Buy me a Ko-fi: https://ko-fi.com/letstalkmicro
Check-up Semanal #204: Doença de Parkinson, vacina meningocócica e mais!
Confira os temas do Check-up Semanal de hoje: Diretriz brasileira para tratamento de sintomas não motores na doença de Parkinson; Fezolinetant e elinzanetant no tratamento dos sintomas vasomotores da menopausa; CROI 2025: Tecovirimat é eficaz no tratamento de mpox?; Atualização: Quais são as recomendações do novo consenso sobre BIA-ALCL?; FDA aprova vacina meningocócica contra 5 sorotipos de Neisseria meningitidis. Ouça agora!
On episode #85 of the Infectious Disease Puscast, Daniel and Sara review the infectious disease literature for the weeks of 7/3 – 7/21/25. Hosts: Daniel Griffin and Sara Dong Subscribe (free): Apple Podcasts, RSS, email Become a patron of Puscast! Links for this episode Viral Elimination of HIV Reservoirs Harboring Intact Proviruses (JID) Bacterial Expansion of tetM-Carrying Neisseria gonorrhoeae in the United States, 2018–2024 (NEJM) Study hints doxyPEP use coincides with rise in tetracycline-resistant gonorrhea in US (CIDRAP) Potential Impact of Doxycycline Post-Exposure Prophylaxis on Tetracycline Resistance in Neisseria gonorrhoeae and Colonization With Tetracycline-Resistant Staphylococcus aureus and Group A Streptococcus (CID) Methenamine hippurate asprophylaxis for recurrent urinary tract infections in older women – a triple-blind, randomised, placebo-controlled, phase IV trial (ImpresU). (CMI: Clinical Microbiology and Infection) Diagnosis and Management ofCommunity-acquired Pneumonia(American Journal of Respiratory and Critical Care Medicine) Complicated Urinary Tract Infections (cUTI): Clinical Guidelines for Treatment and Management (IDSA) The impact of an intervention to increase follow-up blood cultures for patients with Staphylococcus aureus bacteriuria (Antimicrobial Stewardship & Healthcare Epidemiology) Fungal The Last of US Season 2 (YouTube) Candida auris Containment Responses in Health Care Facilities that Provide Hemodialysis Services (CDC: MMWR) Candidozyma auris: an emerging threat (Reflections on Infectious Prevention and Control) Effects of postoperative antifungal therapy on the recurrence of Aspergillus infection after pulmonary aspergilloma resection (BMC Infectious Diseases) Triazole-resistant Aspergillus fumigatus in the Netherlands between 1994 and 2022: a genomic and phenotypic study (LANCET: Microbe) Large language models and their performance for the diagnosis of histoplasmosis (PLoS Neglected Tropical Diseases) Parasitic Field evidence of Trypanosoma cruzi infection, diverse host use and invasion of human dwellings by the Chagas disease vector in Florida, USA (PLoS Neglected Tropical Diseases) Music is by Ronald Jenkees Information on this podcast should not be considered as medical advice.
Antimicrobial Resistance in Neisseria Gonorrhoeae: Surveillance Programs
Microbiologist and Associate Professor at the University of Washington Dr. Olusegun Soge reviews four U.S. based surveillance programs: GISP, eGISP, SURGG, and CARGOS – the umbrella program rolled out in August 2024. Dr. Soge and National STD Curriculum Podcast Host Dr. Meena Ramchandani also discuss a vaccine and another STI pathogen developing resistance. View episode transcript and references at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW), Program Director of the UW Infectious Diseases Fellowship Program, and Associate Editor of the National STD Curriculum.
Antimicrobial Resistance in Neisseria Gonorrhoeae: Key Microbiologic Factors
Microbiologist and Associate Professor at the University of Washington Dr. Olusegun Soge reviews six different ways that the microbiology of Neisseria gonorrhoeae contributes to its antimicrobrial resistance. Dr. Soge and National STD Curriculum Podcast Host Dr. Meena Ramchandani then explore how current overuse and misuse of antibiotics in the STI field might be part of the problem. View episode transcript at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW), Program Director of the UW Infectious Diseases Fellowship Program, and Associate Editor of the National STD Curriculum.
Antimicrobial Resistance in Neisseria Gonorrhoeae: Past, Present, and Future
CDC and the World Health Organization consider Neisseria gonorrhoeae an urgent antibiotic-resistant threat because it continuously develops resistance. Microbiologist and Associate Professor at the University of Washington Dr. Olusegun Soge provides a historical overview of past efforts, an update on the current situation, why global surveillance is so important, and a potential new treatment for uncomplicated gonorrhea. View episode transcript at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW), Program Director of the UW Infectious Diseases Fellowship Program, and Associate Editor of the National STD Curriculum.
Épisode 153 – Chlamydia et gonorrhée: les invités qu'on ne veut pas laisser entrer! – Partie 2
Un nouvel épisode du Pharmascope est disponible! Dans ce 153e épisode, Nicolas, Isabelle et Olivier discutent de chlamydia et de gonorrhée. Cette deuxième partie est consacrée au traitement de ces infections. Les objectifs pour cet épisode sont les suivants: Discuter de la prise en charge de la chlamydia et de la gonorrhée. Discuter des traitements antibiotiques de la chlamydia et de la gonorrhée. Discuter de l'utilisation de la DOXY-PEP. Ressources pertinentes en lien avec l'épisode Agence de la santé publique du Canada. Chlamydia, gonorrhée et syphilis infectieuse au Canada : Données de surveillance de 2021. INESSS. Guide d'usage optimal : Infection confirmée à Chlamydia trachomatis ou à Neisseria gonorrhoeae. Septembre 2024. INESSS. Guide d'usage optimal : Approche syndromique. Décembre 2024. Portail VIH/sida du Québec : Notification anonyme des partenaires. MSSS. Traitement accéléré des partenaires pour les infections à Chlamydia trachomatis et à Neisseria gonorrhoeae - Aide-mémoire pour les cliniciens. Juillet 2021. MSSS. Traitement accéléré des partenaires pour les infections à Chlamydia trachomatis et à Neisseria gonorrhoeae - Aide-mémoire pour les pharmaciens. Juillet 2021. MSSS. Carte de notification chlamydia/gonorrhée. Juillet 2021. Páez-Canro C et coll. Antibiotics for treating urogenital Chlamydia trachomatis infection in men and non-pregnant women. Cochrane Database Syst Rev. 2019 Jan 25;1(1):CD010871. Lau A et coll. Azithromycin or Doxycycline for Asymptomatic Rectal Chlamydia trachomatis. N Engl J Med. 2021 Jun 24;384(25):2418-2427. Bížová B et coll. Single-dose cefixime 800 mg plus doxycycline 100 mg twice a day for 7 days compared with single-dose ceftriaxone 1 g plus single-dose azithromycin 2 g for treatment of urogenital, rectal, and pharyngeal gonorrhoea: a randomised clinical trial. Clin Microbiol Infect. 2024 Feb;30(2):211-215. Nguyen PTT et coll. Randomized controlled trial of the relative efficacy of high-dose intravenous ceftriaxone and oral cefixime combined with doxycycline for the treatment of Chlamydia trachomatis and Neisseria gonorrhoeae co-infection. BMC Infect Dis. 2022 Jul 9;22(1):607. Yang KJ et coll. Effectiveness of Cefixime for the Treatment of Neisseria gonorrhoeae Infection at 3 Anatomic Sites: A Systematic Review and Meta-Analysis. Sex Transm Dis. 2023 Mar 1;50(3):131-137. Kirkcaldy RD et coll. The efficacy and safety of gentamicin plus azithromycin and gemifloxacin plus azithromycin as treatment of uncomplicated gonorrhea. Clin Infect Dis. 2014 Oct 15;59(8):1083-91. Bachmann LH, Barbee LA, Chan P, et colll. CDC Clinical Guidelines on the Use of Doxycycline Postexposure Prophylaxis for Bacterial Sexually Transmitted Infection Prevention, United States, 2024. MMWR Recomm Rep. 2024;73(2):1-8.
The Mind-Mouth Connection: How Oral Bacteria Impacts Your Brain
Story at-a-glance Research found that higher levels of harmful bacteria (Prevotella intermedia) in the mouth are linked to cognitive impairment, while beneficial bacteria (Neisseria and Haemophilus) support better brain function Nitric oxide production by beneficial oral bacteria plays a crucial role in maintaining blood flow to the brain. Nitrate-rich vegetables help boost the population of these healthy bacteria People with the APOE4 gene show a distinct oral microbiome composition. Research shows they have lower levels of Neisseria bacteria and higher amounts of Prevotella, which is associated with increased dementia risk Harmful oral bacteria have the ability to enter the bloodstream and cross the blood-brain barrier, leading to brain inflammation that results in cognitive decline Maintaining oral health through proper diet, regular brushing and flossing, nose breathing, avoiding antibacterial mouthwash and practicing oil pulling are effective strategies against cognitive decline
Hosts: Jake Lancaster MD, Chief Medical Information Officer and Amanda Comer DNP, System Director, Advanced Practice ProvidersGuest: Alex Yoby, PharmacistCME Credit Info:Link to complete brief survey and claim CME credit: https://www.surveymonkey.com/r/C55LKSYCME credit is available for up to 3 years after the stated release dateContact CEOD@bmhcc.org if you have any questions about claiming credit.CDC's Sexually Transmitted Infections (STI) TreatmentGuidelines, 2021Notable updates:These guidelines discuss 1) updated recommendations fortreatment of Neisseria gonorrhoeae, Chlamydia trachomatis, andTrichomonas vaginalis; 2) addition of metronidazole to the recommendedtreatment regimen for pelvic inflammatory disease; 3) alternative treatmentoptions for bacterial vaginosis; 4) management of Mycoplasma genitalium;5) human papillomavirus vaccine recommendations and counseling messages; 6) expanded risk factors for syphilis testingamong pregnant women; 7) one-time testing for hepatitis C infection; 8)evaluation of men who have sex with men after sexual assault; and 9) two-steptesting for serologic diagnosis of genital herpes simplex virusSyphilis LoreIt is postulated that syphilis came to Europe in the 1490s when Columbusarrived in Italy from America. After Italy surrendered to the invading Frenchin 1495, this new disease rapidly spread across Europe. The name"syphilis" comes from the work of Girolamo Fracastoro, a noted poetand physician in Verona, Italy. In 1530, he wrote about a shepherd namedSyphilus who angered Apollo, causing the god to curse the entire populationwith the affliction that we now know as syphilisT. pallidumSyphilis is a systemic, bacterial infection caused byTreponema pallidum. Treponema are thin,Gram-negative, slowly metabolizing spirochetal bacterium, requiring an averageof 30 hours to multiply. It is microaerophilic and cannot grow on standardculture media. Treponema pallidum's outer membrane lacks lipopolysaccharidesand has few surface-exposed unique proteins, making it difficult for the immunesystem to fight the infection. Because of this characteristic, Tpallidum is labeled as a stealth pathogen. T. pallidum is theonly Treponema species that causes sexually transmitted disease.Syphilis is characterized by a wide range of variableclinical symptoms that can resemble other diseases, which make it difficult todiagnose without a test, therefore, it is often referred to as “The GreatImitator”. The infection progresses through multiple stages (primary,secondary, latent, and tertiary) and can affect virtually every organ system inthe body, even many years or even decades after the original infection.Infected people are contagious during the primary and secondary stages ofsyphilis.Stages of syphilisPrimary syphilis: Primary syphilis classicallypresents as a single painless ulcer or chancre at the site of infection but canalso present with multiple, atypical, or painful lesions. A chancre is definedas a firm, round, painless ulcer at the...
Today we will discuss if screening asymptomatic Men who have sex with Men, also referred to as MSM, who are receiving HIV pre-exposure anti-retroviral medication, called HIV PrEP, routinely for bacterial STIs, gonorrhoea and chlamydia through pharyngeal, urine and rectal PCR testing every three months- also referred to as 3x3 testing is indeed of benefit or may cause harm. This year, in Lancet HIV, the Gonoscreen trial, a randomised controlled trial, of 500 MSM on PrEP in each arm followed up for 12 months reported that 3x 3 testing does not reduce the incidence of gonorrhoea and chlamydia infections in this specific cohort. In Belgium, this trial has led to a change in clinic practice through the Belgium HIV PrEP guidelines where patients will be screened less frequently and intensely. Lancet ID on the other hand published an opinion piece by Raccagni et al where concerns about transmission and morbidity risk of untreated infection and implications of using poor quality screening tools are voiced. We will discuss today the merit of the Gonoscreen trial and other studies that support a decrease in screening & treating asymptomatic bacterial STIs and exercising stricter antimicrobial stewardship versus the risks associated with leaving asymptomatic infections untreated and risking morbidity and transmission. Relevant links: Effect of screening for Neisseria gonorrhoeae and Chlamydia trachomatis on incidence of these infections in men who have sex with men and transgender women taking HIV pre-exposure prophylaxis (the Gonoscreen study): results from a randomised, multicentre, controlled trial Primum non-nocere: Is it time to stop screening for Neisseria gonorrhoeae and Chlamydia trachomatis in men who have sex with men taking HIV pre-exposure prophylaxis? The arrested immunity hypothesis in an immunoepidemiological model of Chlamydia transmission Gonorrhoea and chlamydia screening for asymptomatic people with HIV and HIV PrEP users: open issues Host: Dr Fabiola Martin, Sexual Health Specialist and Associate Professor, Australian National University, Canberra, Australia Dr Thibaut Vanbaelen, physician and post-doctoral researcher at The Institute of Tropical Medicine in Antwerp, Belgium Dr Angelo Roberto Raccagni, physician at Vita-Salute San Raffaele University in Milan, Italy
Dr. Johan Melendez, a Johns Hopkins School of Medicine Assistant Professor, discusses STI antimicrobial resistance (AMR) and why Neisseria gonorrhoea is resistant, AMR diagnostic options such as point-of-care assays, and his work on evaluating AMR in resource-limited settings with National STD Curriculum Podcast Editor Dr. Meena Ramchandani. View episode transcript at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW) and Program Director of the UW Infectious Diseases Fellowship Program.
A microbicide for Neisseria gonorrhoeae? In this episode Luis is joined by Dr. María Rendón from the University of Arizona. Dr. Rendón joins the podcast to talk about a novel microbicide that was developed which has activity against N. gonorrhoeae . How does it work? Does it affect commensal Neisseria? What about methylation signatures? Tune in to learn more about this microbicide.Link to articles referenced in episode:http://microbialcell.com/researcharticles/2019a-so-microbial-cell/https://www.cell.com/action/showPdf?pii=S1931-3128%2819%2930347-6Link to study: https://journals.asm.org/doi/abs/10.1128/aac.00794-24?doi=10.1128/aac.00794-24Questions? Feedback? Send those to letstalkmicro@outlook.comWant to support the podcast? Here's how:Venmo: https://venmo.com/u/letstalkmicroBuy me a Ko-fi: https://ko-fi.com/letstalkmicro
Meningitis B outbreaks: vaccination and risk in university settings
Send us a textOn this episode of the CMAJ Podcast, Dr. Blair Bigham and Dr. Mojola Omole explore the ongoing public health concern of meningococcal disease, focusing on meningitis B outbreaks in Canadian universities. They are joined by Dr. Cristin Muecke, a medical officer of health in Halifax, and Dr. Savita Rani, a public health specialist at the University of Saskatchewan. The episode also features the personal story of Megan Plamondon, a Queen's University student who contracted invasive meningococcal disease.The discussion opens with a look at recent meningitis B outbreaks, including cases at Dalhousie University in 2022 and Queen's University in 2023. The Halifax outbreak led to a targeted vaccination effort offering publicly funded MenB vaccines to students in congregate living environments, such as dormitories and residences.Dr. Muecke provides insights into the Halifax outbreak and the public health response that followed. She discusses the complexities of identifying and controlling meningococcal disease in university settings, where asymptomatic carriers of Neisseria meningitidis can unknowingly contribute to the spread of the infection.Dr. Rani expands on the current state of MenB vaccination, explaining why the vaccine is not included in routine immunization schedules and outlining the challenges of securing broader vaccine coverage across the country. She emphasizes the importance of early detection, given that meningitis can present with nonspecific symptoms which complicates diagnosis.Megan Plamondon's story brings a lived experience perspective to the conversation, highlighting the severe impact of meningococcal disease and the critical need for prevention efforts, particularly among students entering congregated living environments for the first time.Join us as we explore medical solutions that address the urgent need to change healthcare. Reach out to us about this or any episode you hear. Or tell us about something you'd like to hear on the leading Canadian medical podcast.You can find Blair and Mojola on X @BlairBigham and @DrmojolaomoleX (in English): @CMAJ X (en français): @JAMC FacebookInstagram: @CMAJ.ca The CMAJ Podcast is produced by PodCraft Productions
Ces dangereuses bactéries: la Neisseria meningitidis Si la majorité des bactéries sont inoffensives voire bénéfiques pour la santé, certains types de bactéries sont pathogènes et à l'origine de nombreuses maladies comme la peste, la tuberculose ou le choléra. Tout au long de la semaine, Anne Baecher propose de découvrir le monde complexe, fascinant et terrifiant de ces organismes microscopiques. Résistance aux antibiotiques, taux de mortalité élevé malgré les traitements. Jacques Schrenzel, chef du laboratoire de bactériologie et du laboratoire de génomique des Hôpitaux universitaires de Genève (HUG), fait le point sur la bactérie Neisseria meningitidis, responsable de la méningite. Micro sciences: le zèbre est-il blanc avec des rayures noires, ou lʹinverse? C'est une question qui m'a toujours amusée : le zèbre est-il blanc avec des rayures noires, ou noir avec des rayures blanches ? Figurez-vous que ce sont les mathématiques qui nous permettent de faire la lumière sur les motifs du zèbre (et sur ceux d'autres animaux). Michel Milinkovitch, professeur ordinaire au département de génétique et évolution de l'Université de Genève, m'explique comment ces motifs peuvent être expliqués par des formules mathématiques trouvées par deux pères fondateurs de l'informatique, Alan Turing et John von Neumann. La science en chansons: "Bébéboa" Stéphane Délétroz dévoile sa liste de chansons qui évoquent des concepts scientifiques et sʹamuse à les décortiquer. Dans cet épisode: "Bébéboa" (2021) dʹOrelsan pour parler dʹalcoolisme.
117. Meningococcal Vaccine: Prevention of Meningococcal Disease in Adolescents and Young Adults
On this episode of NP Pulse: The Voice of the Nurse Practitioner®, Drs. Mary Koslap-Petraco and Ruth Carrico will discuss meningococcal disease, the maze of meningococcal vaccines, ACIP recommendations and the use of shared clinical decision-making. Meningococcal disease — a life-threatening infection caused by Neisseria meningitidis — demands our attention. It strikes swiftly, leaving devastation in its wake. Still, we have powerful tools at our disposal: MenACWY and MenB vaccines, and a new, game-changing pentavalent vaccine that covers serogroups A, B, C, W and Y. Additionally, a meningitis point-of-care tool will be available on AANP's Tools and Resources page. To earn 1.0 contact hours of continuing education (CE) credit, you will need the participation code provided at the end of the podcast. To claim your CE credit, log in and register for the activity within the AANP CE Center, then enter the participation code and complete the post-test and evaluation. CE credit is available for this podcast through June 2025. This educational activity is supported by an independent medical education grant from GSK.
Episode 168: UTI in MalesFuture Dr. Tran gives a summary of UTIs in Males, including epididymitis, orchitis, urethritis, prostatitis, and pyelonephritis. Diagnosis and treatment were briefly described and some differences with female patients were mentioned by Dr. Arreaza. Written by Di Tran, MS-3, Ross University School of Medicine. Editing and comments by Hector Arreaza, MD.You are listening to Rio Bravo qWeek Podcast, your weekly dose of knowledge brought to you by the Rio Bravo Family Medicine Residency Program from Bakersfield, California, a UCLA-affiliated program sponsored by Clinica Sierra Vista, Let Us Be Your Healthcare Home. This podcast was created for educational purposes only. Visit your primary care provider for additional medical advice.WHAT ARE URINARY TRACT INFECTIONS?Urinary Tract Infection (UTI) is an infection of any part of the urinary tract system. It may involve any part of the renal system, the kidneys, the ureters, the bladder, the prostate, and the urethra. Different from men, a woman may get a UTI more easily due to their anatomical difference. A woman's urethra is shorter and lies close in proximity to both the vagina and the anus, which allows easy access for bacteria to travel up to the bladder.UTI is further subdivided into two different categories, depending on where the infection takes place within the urinary tract:Lower Tract Infection – cystitis and urethritis when the infection occurs on the bladder and the urethra, respectively. Common infections are a result of bacteria migrating from the skin (and also from sexual organs) to the urethra and ending up in the bladder.In males, other forms of lower tract infection can result in prostatitis, epididymitis, and orchitis.Upper Tract Infection - aka pyelonephritis, is a more concerning infection that involves the upper parts of the urinary system, in other words, the ureters, and kidneys.AGE DIFFERENCES IN UTI FOR MEN:For men, the incidence of UTI increases with age. Dr. John Brusch reports UTI rarely develops in young males and the prevalence of bacteriuria is 0.1% or less. Men who are 15-50 years of age often have urethritis due to sexually transmitted infection (STI), mainly by Neisseria gonorrhoeae and Chlamydia trachomatis. Symptoms include frequency, urgency, and dysuria (most common).Men who are 50 years or older, especially those with prostatic hyperplasia, will have signs and symptoms of incomplete bladder emptying, hesitancy, slow stream, difficulty initiating urination, and dribbling after urinating. Due to the enlargement of the prostate gland, there will be partial blockage of urine flow from the bladder, which in turn, creates a reservoir where bacteria can grow and cause an infection. The most common offending microorganism for this age group is Escherichia coli.Interestingly, while UTIs are rare among men under 60, by the age of 80, both women and men have similar incidence rates. The bladder tends to have a higher residual volume in older males because the prostate grows no matter what, it´s just a part of aging for males. Some may end up with more or less lower urinary tract symptoms, but the prostate is enlarged in general.Other risk factors for UTI in males are men who are not circumcised, urethral strictures, fistulas, hydronephrosis (or dilated ureters overfilled with urine due to failure of drainage to the bladder), and the use of urinary catheters. DIFFERENT TYPES OF UTIs IN MALES:EPIDIDYMITIS:The infection starts from the retrograde ascending route from the prostatic urethra, backing up to the vas deferens, and eventually ending in the epididymis.In men who are younger than 35 years of age, the usual pathogens are C. trachomatis and N. gonorrhoeae (sexually transmitted).In men who are older than 35 years of age, the usual offending agents are Enterobacteriaceae and gram-positive cocci (E. coli as mentioned previously).ORCHITIS:This unique UTI is caused by viral pathogens, such as mumps, coxsackie B, Epstein-Barr (EBV), and varicella (VZV) viruses. Several studies have shown that patients having orchitis have a history of epididymitis. Fortunately, this infection is uncommon, and it was the main reason to develop the MMR vaccine. It is caused by viruses other than mumps, so you can still have orchitis even if you are vaccinated. Antibiotics are not prescribed for viral orchitis.BACTERIAL CYSTITIS:Having a similar pathophysiology of ascending infection mechanism, male patients in this category often present frequency, urgency, dysuria, nocturia, and suprapubic pain. On a side note, having hematuria is concerning, especially without symptoms, because it's automatically a red flag that should prompt an immediate evaluation in search of other causes besides infection, such as underlying malignancy. Possible etiologies are calculi, glomerulonephritis, and even schistosomiasis infection that can ultimately result in squamous cell carcinoma of the bladder. Arreaza: Let me share a little anecdote about hematuria. One Sunday when I was a resident I woke up with hematuria. Of course, I immediately went to urgent care, knowing hematuria means trouble in men. I had a urine dipstick test, which was normal. The first thing the nurse practitioner asked me was, “Did you eat any beets?”, and I never eat beets, but that day I had a full bag of beet chips. So, yes, that was the cause of my pseudo-hematuria. Lesson learned: Always ask about beets when you have a patient with painless hematuria with a normal dipstick. PROSTATITIS:This is an infection of the prostate gland. The most common offending agent is E. coli. Acute prostatitis will present with signs of “acute” infection, such as fever, chills, and suprapubic pain. On rectal exam, we will find a prostate that is warm, swollen, boggy, and very tender. Make sure you perform a gentle prostate exam as you may spread bacteria to the blood and cause bacteremia and potentially sepsis. Patients are normally very sick and it is not your typical cystitis, but it is more severe. Chronic Prostatitis can arise from different causes, ranging from retrograde ascending infection, “chronic” exposure to urinary pathogens, and even autoimmune etiologies. The majority of patients often are asymptomatic. URETHRITIS:This infection is further classified into two groups, gonococcal and non-gonococcal. For gonococcal urethritis, N. gonorrhoeae is the most common pathogen. Agents of non-gonococcal urethritis include C. trachomatis, Ureaplasma, trichomonas, and Herpes Simplex Virus (HSV). Patients often present symptoms of dysuria, pruritus, and purulent penile discharge.PYELONEPHRITIS:Following a retrograde ascending mechanism, an infection may travel from the bladder and make its way to the kidney, causing damage and inflammation to the renal parenchyma. According to Dr. John Brusch, E. coli is responsible for approximately 25% of cases in males. Pyelonephritis presents with chills, fever, nausea/vomiting, flank pain/costovertebral angle tenderness, and dysuria. Other findings include pyuria and bacteriuria. Pyelonephritis is a common cause of sepsis. Diagnosis of UTIs.URINE STUDIES: Urine culture remains the gold standard for diagnosis of UTI. Other studies include suprapubic aspiration, catheterization, midstream clean catch, and Gram stain. Imaging studies are not always needed, but you may order plain films, ultrasonography, CT scans, and MRIs. It will depend on the severity of your case and your clinical judgment.UTIs in women: In males, we should perform urine culture and susceptibility studies. However, in women, urine studies are not needed all the time, they should be reserved for women with recurrent infection, treatment failure, history of resistant isolates, or atypical presentation. This is done to confirm the diagnosis and guide antibiotic selection.Interestingly, in a recent evidence review, published in the American Family Physician journal, women can self-diagnose their uncomplicated cystitis. All that is needed is having typical symptoms (frequency, urgency, dysuria/burning sensation, nocturia, suprapubic pain), without vaginal discharge. If you have those elements, you have enough information to diagnose, or even the patient can self-diagnose, an uncomplicated UTI without further testing, but in males, you should ALWAYS perform urine studies.TREATMENTS:Men with UTI should ALWAYS receive antibiotics, with urine culture and susceptibility results guiding the antibiotic choice. Laboratory results will help us determine the best treatment plan. UTIs are often treated with a variety of antibiotics. Dr. Robert Shmerling, of Harvard Medical School, states that most uncomplicated lower tract infections can be eradicated with a week of treatment with antibiotics. Common antibiotics for UTI are fluoroquinolones, trimethoprim-sulfamethoxazole (TMP-SMZ), minocycline, or nitrofurantoin.On another hand, if it's an upper tract infection or prostatitis, the course of treatment can be extended for longer periods. For those patients who are hemodynamically unstable or have severe upper UTI, hospital admission is required to monitor for complications and IV antibiotics.UTIs in males are less frequent than UTIs in females, except when patients are 80 years and older when the incidence is similar in both sexes. UTIs in males must prompt further evaluation because if left untreated, they can have detrimental effects on your patients' health. As a take-home point, UTI in males is less common than in females, and it requires urine studies or other studies to identify the etiology and guide treatment. Antibiotics are always used, and you may guide your treatment depending on the results. Imaging is not always needed, but use your clinical judgment to make a more specific diagnosis and detect complications promptly. __________Conclusion: Now we conclude episode number 168, “UTI is Males.” Future Dr. Tran described the different anatomical areas that can be infected in males with UTI. She reminded us that UTIs in males always need to be treated with antibiotics and urine cultures are done to guide treatment. Dr. Arreaza mentioned a few differences in the diagnosis and treatment of UTIs in females. For example, women can self-diagnose an uncomplicated cystitis, and urine studies or antibiotics are not always needed in women. This week we thank Hector Arreaza and Di Tran. Audio editing by Adrianne Silva.Even without trying, every night you go to bed a little wiser. Thanks for listening to Rio Bravo qWeek Podcast. We want to hear from you, send us an email at RioBravoqWeek@clinicasierravista.org, or visit our website riobravofmrp.org/qweek. See you next week! _____________________References:Shmerling, R. H. (2022, December 5). Urinary tract infection in men. Harvard Health Publishing. https://www.health.harvard.edu/a_to_z/urinary-tract-infection-in-men-a-to-z.Brusch, J. L. (2023a, March 27). Urinary tract infection (UTI) in males. emedicine.medscpae.com. https://emedicine.medscape.com/article/231574-overview.Kurotschka PK, Gágyor I, Ebell MH. Acute Uncomplicated UTIs in Adults: Rapid Evidence Review. Am Fam Physician. 2024;109(2):167-174. https://www.aafp.org/pubs/afp/issues/2024/0200/acute-uncomplicated-utis-adults.htmlRoyalty-free music used for this episode: Tropicality by Gushito, downloaded on July 20, 2023, from https://www.videvo.net/royalty-free-music/
Revisiting gonorrhoea: Update on the 4CMenB vaccine for gonorrhoea prevention
You will recall a previous podcast about preventing Neisseria gonorrhoea through an effective vaccine. Neisseria gonorrhoeae is a ubiquitous sexually transmitted bacteria that can cause both localised and systemic disease if left untreated. It may be transmitted to neonates. We also reported on a rise of the gonorrhoea incidence, as well as increasing rates of antibiotic resistance. Today we will revisit the implementation of vaccinations against gonorrhoea in the UK. Here is an exciting up-date on the advice provided by UK's Joint Committee on Vaccination and Immunisation, JCVI, on using the vaccine 4CMebB OMV against Meningococcus used off-label for the prevention of gonorrhoea infection • in patients at significant risk of infection with bacterial STIs who • attend specialist sexual health services. Host: Dr. Fabiola Martin, Sexual Health HIV, HTLV Specialist, Canberra Sexual Health Services & University of Queensland, Australia Participants: Dr. Suneeta Soni, Consultant in Sexual Health and HIV, University Hospitals Sussex and Chair of the Bacterial special interest group for BASHH *British Association for Sexual health and HIV) Dr. Yen Bui, Consultant in Vaccination and Travel Health, Institut national de santé publique du Québec, Canada A/P. Dr. Kate Seib, NHMRC Leadership Fellow and Associate Director for Research, Institute for Glycomics, Griffith University, Australia
Can Gonorrhea, Chlamydia, or Mgen Spontaneously Clear?
This episode reviews five articles regarding spontaneous clearance of Neisseria gonorrhoea, Chlamydia trachomatis, and Mycoplasma genitalium without the use of antibiotics. View episode transcript and references at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW) and Program Director of the UW Infectious Diseases Fellowship Program.
Antimicrobial Resistance in Neisseria Gonorrhoeae (JCM ed.)
Gonorrhea remains one of the more common sexually transmitted infections. In North America, the number of reported cases has generally risen for over ten years, with interruptions in the early days of the COVID-19 pandemic, followed by returns to rising rates of infection. Under the selective pressure of antimicrobial treatment, antimicrobial resistance has risen, which has led to limited options for treatment Today, we will be discussing antimicrobial resistance in N. gonorrhoeae, including these questions: • How accurate is gradient diffusion susceptibility testing when compared to agar-dilution results? • Should we use analysis of whole genome sequencing results or agar dilution phenotypic results as the gold-standard for antibiotic susceptibility testing of N. gonorrhoeae? • What is the utility of beta-lactamase testing for predicting penicillin susceptibility results in N. gonorrhoeae? Guests: Dr. Tanis Dingle, Clinical Microbiologist at Alberta Precision Laboratories and a Clinical Associate Professor in the Department of Pathology and Laboratory Medicine at the University of Calgary. Dr. Angela Ma., Clinical Microbiologist at Public Health Ontario. Link: Use of genome sequencing to resolve differences in gradient diffusion and agar dilution antimicrobial susceptibility testing performance of Neisseria gonorrhoeae isolates in Alberta, Canada This episode of Editors in Conversation is brought to you by the Journal of Clinical Microbiology and hosted by JCM Editor in Chief, Alex McAdam and Dr. Elli Theel. JCM is available at https://jcm.asm.org and on https://twitter.com/JClinMicro. Visit journals.asm.org/journal/jcm to read articles and/or submit a manuscript. Follow JCM on Twitter via @JClinMicro
Dalağın fonksiyonunun çeşitli durumlar sonucunda tamamen kaybına ya da cerrahi olarak çıkarılmış olmasına aspleni, dalağın normalden az fonksiyon göstermesine hipospleni adı verilmektedir. Dalak, lenfoid sisteme ait önemli bir organ olduğu için aspleni durumu, hastalara yaklaşım açısından önem arz eder. Splenektomi ameliyatları en sık dalak yaralanmaları nedeniyle planlanır. Fonksiyonel aspleni ise en sık orak hücreli anemide görülür, hastaların neredeyse tamamında yaşamın ilerleyen evrelerinde aspleni gelişmektedir. Bu durumlar dışında kronik karaciğer hastalıklarında, hemolitik anemilerde, talasemi, maligniteler, HIV enfeksiyonu, sarkoidoz, amiloidoz, Çölyak hastalığı, Whipple hastalığı, sistemik lupus eritematozus ve romatoid artrit gibi bazı hastalıklarda farklı derecelerde hipospleni veya aspleni söz konusu olabilir. Bu yazıda acil servise başvuran asplenik hastalara yaklaşımda dikkat edilecek noktalara değinmek istedim. 1 2 3 4 İyi okumalar! Yapı ve Fonksiyon Dalak lenfatik sistemin en büyük organıdır. Diğer lenfoid organlardan farklı olarak korteks ve medullası yoktur. Beyaz pulpa, kırmızı pulpa, vasküler sistem ve destek dokudan meydana gelir. Bir dakikada toplam kalp debisinin %5'ini alır. Hem humoral hem de hücresel immünitede rol oynar. Antijen sunan hücreler ile immün yanıtı başlatır. Beyaz pulpadaki T ve B lenfositlerinin aktivasyonu ve proliferasyonu ile lökositlerin olgunlaşma ve yapım yeridir. Retiküloendotelyal sistemin bir parçası olarak, yaşlanan kan hücrelerini ve mikroorganizmaları uzaklaştırır. Opsonize edilmemiş bakterilerin ve Streptococcus pneumoniae, Neisseria meningitidis ve Haemophilus influenzae gibi kapsüllü bakterilerin uzaklaştırıldığı tek yerdir. Dalak ayrıca alternatif kompleman yolunda da rol oynar. Dalağın inflamatuar kaskadda ve pıhtılaşmada da önemli rolü vardır. Literatürde asplenik hayvanlarda sepsise gidişin ve sepsis mortalitesinin daha yüksek olduğu gözlenmiştir. Ayrıca dalağın normal fonksiyonunun olmadığı hastalarda sitokin aktivitesinin, trombin seviyelerinin, trombosit sayı ve aktivitesinin arttığı; intravasküler hemolizin ve eritrosit membran anormalliklerinin görüldüğü bilinmektedir. Bu faktörler makrovasküler ve mikrovasküler tromboz riskini artırmaktadır. Aspleni Komplikasyonları Enfeksiyon Aspleni önemli enfeksiyon riskine neden olur, bu hastalarda sepsis ve enfeksiyona bağlı ölüm riski genel popülasyona göre 2-3 kat daha fazladır. Asplenik bir hasta enfeksiyon geliştirirse, sonraki 3 yıl boyunca başka bir enfeksiyon için 6 kat daha yüksek risk altındadır. Riski azaltmak için yapılacaklar şunlardır: En önemli bileşen hasta eğitimidir. Hastalar enfeksiyon riskleri ve türleri, aşıların önemi ve ne zaman tıbbi yardıma başvurmaları gerektiği konusunda bilgilendirilmelidir. Aşılanma: Uygulanan aşılar arasında pnömokok, meningokok ve HiB aşısı bulunmaktadır. Splenektomi elektif planlanmışsa aşılamalar genellikle ameliyattan 10-12 hafta önce başlatılır, böylece tüm süreç elektif splenektomiden 2 hafta önce tamamlanır. Acil splenektomi yapılan hastalarda aşılar splenektomiden 14 gün sonra planlanmalıdır. Önerilen diğer aşılar arasında yıllık influenza aşısı da bulunmaktadır. Antibiyotik profilaksisi: Splenektomi sonrası yaklaşık 1 yıl boyunca hastalara antibiyotik profilaksisi verilmektedir. İmmünsüprese hastalara ve ciddi enfeksiyon öyküsüne sahip olanlara yaşam boyu profilaksi uygulanabilir. Profilakside genellikle penisilin V ve amoksisilin tercih edilmektedir. Gerekli durumlarda sefalosporinler, florokinolonlar veya makrolidler de kullanılabilir. Acil antibiyotikler: Ateş veya sistemik enfeksiyonu düşündüren semptomlar varlığında kullanılmak üzere hastanın yanında amoksisilin-klavulanat veya sefdinir içeren bir antibiyotiğin olması sağlanır. Bu gruplara alerjisi veya intoleransı olanlar için levofloksasin veya moksifloksasin önerilir. Hastaların acil antibiyotiğin bir dozunu hemen alıp acil servise başvurması gerekmektedir.
A statewide outbreak of meningococcal disease has infected 27 people since June 2022 and killed five of them, and Virginia Department of Health officials have declared a statewide outbreak of the disease. The illness is caused by the bacteria called Neisseria meningitidis type Y. The cases have been reported in eastern, central, and southwest Virginia during the past 15 months – about three times the expected number of cases during the same timeframe, according to VDH officials. Most cases are residents of eastern Virginia, where a regional outbreak was first announced in September 2022. The most recent notice to the...Article LinkSupport the show
ON this week's episode I sat down with Nurse practitioner damian valle to talk about a case of septic arthritis. Damo is a nurse pract with a love for teaching and training. The case is an excellent example of why getting a clinical history is important and why reassessment is always so important. On the episode we spoke why doing a complete physical exam is paramount. SHOW NOTES Disseminated gonococcal infection (DGI) results from bacteremic spread of the sexually transmitted pathogen, Neisseria gonorrhoeae, which can lead to a variety of clinical symptoms and signs, such as arthritis or arthralgias, tenosynovitis, and multiple skin lesions.click link to follow Reactive arthritis is conventionally defined as an arthritis that arises following an infection, although the pathogens cannot be cultured from the affected joints. It is generally regarded as a form of spondyloarthritis (SpA). click link to follow Septic arthritis is synonymous with an infection in a joint. Septic arthritis is usually caused by bacteria but can also be caused by other microorganisms. Septic arthritis due to bacterial infection is often a destructive form of acute arthritis. click link to follow
Neisseria gonorrhoeae, in short NG, is a ubiquitous sexually transmitted bacteria that can cause both localised and systemic disease if left untreated. NG may also be transmitted vertically from mother to baby. Over the last years, we have seen a rise in the number of people diagnosed with gonorrhoea, alongside growing rates of antibiotic resistance. New research makes us hopeful that a vaccine may soon become available to provide global, large scale benefits. In this podcast, we explore this possibility with three experts in the field: Prof Kate Seib (1), Dr Claire Dewsnap (2) and Dr Silvia Nozza (3). Would you like to know more about the topic? Please read the paper we recently published in STI: "Prior Neisseria meningitidis (Nm) proctitis does not prevent Neisseria gonorrhoeae (Ng) proctitis among men who have sex with men (MSM)": https://sti.bmj.com/content/99/3/215 (1) NHMRC Leadership Fellow and Associate Director for Research, Institute for Glycomics, Griffith University, Gold Coast, Australia (2) President of the British HIV Association for HIV & Sexual Health (BASHH) and Consultant in Genitourinary Medicine, Sheffield Teaching Hospital, Sheffield, UK (3) Consultant in Infectious Diseases, Head of Prevention Unit, San Raffaele Hospital (IRCCS), Milan, Italy
Swabs vs. Urine | More Mental Health | Siblings of Abuse | Infants and COVID | Scan Too Much
The JournalFeed podcast for the week of June 12-16, 2023.These are summaries from just 2 of the 5 article we cover every week! For access to more, please visit JournalFeed.org for details about becoming a member.Swabs vs. Urine Spoon FeedVaginal swabs are more accurate than urine samples in diagnosing Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. These results support CDC recommendations that vaginal swabs are the preferred sample modality when testing for STIs in women.Infants and COVID Spoon FeedInfants who tested positive for SARS-CoV-2 were less likely to have UTI, bacteremia, and bacterial meningitis.
This episode reviews three articles about four antimicrobial treatment options for Neisseria gonorrhoeae other than ceftriaxone. View episode transcript and references at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW) and Medical Director of the Public Health – Seattle & King County Sexual Health Clinic.
In this episode, we review the high-yield topic of Neisseria gonorrhoeae from the Microbiology section. Follow Medbullets on social media: Facebook: www.facebook.com/medbullets Instagram: www.instagram.com/medbulletsofficial Twitter: www.twitter.com/medbullets --- Send in a voice message: https://podcasters.spotify.com/pod/show/medbulletsstep1/message
Antimicrobial Resistance in Neisseria gonorrhoeae (AAC ed.)
The Center of Diseases Control and Prevention (CDC) has categorized emergent resistance in Neisseria gonorrhoeae as an “urgent” public health problem. We discuss the emerging problem of gonorrhea and implications for public health with experts in the field Topics discussed: The clinical implications of resistance to B-lactams and quinolones in Neisseria gonorrhoeae Mechanisms of resistance in these organisms Insights into therapeutic approaches to treat resistant gonococcal infections. Guests: William M. Shafer, Professor, Department of Microbiology and Immunology, Emory University School of Medicine, Co-Director, Emory Antibiotic Resistance Center Yonatan Grad, Melvin J. and Geraldine L. Glimcher Associate Professor of Immunology and Infectious Diseases, Harvard T. H. Chan School of Public Health This episode is brought to you by the Antimicrobial Agents and Chemotherapy journal available at aac.asm.org. If you plan to publish in AAC, ASM Members get up to 50% off publishing fees. Visit asm.org/membership to sign up. Visit journals.asm.org/journal/aac to browse issues and/or submit a manuscript.
3.27 Chlamydia Species Microbiology review for the USMLE Step 1 exam Chlamydia is a gram-negative bacteria that is an obligate intracellular organism. It has a two-part life cycle involving the reticular body (active form) and elementary body (inactive form). There are three main species of chlamydia that cause human infections: chlamydia trachomatis, chlamydia pneumoniae, and chlamydia psittaci. Chlamydia trachomatis is the most common sexually transmitted infection in the US and causes genital tract infections, lymphogranuloma venereum, pelvic inflammatory disease, and reactive arthritis. Treatment for chlamydia trachomatis includes azithromycin or doxycycline, and ceftriaxone is often added to cover Neisseria gonorrhoeae. Chlamydia trachomatis can also infect neonates during delivery, causing conjunctivitis and pneumonia. Chlamydia pneumoniae causes community-acquired pneumonia spread through respiratory droplets. Chlamydia psittaci is associated with pet birds and also causes pneumonia.
2022 STD Prevention Conference: Testing for Gonorrhea & Antimicrobial Resistance
This episode reviews four abstracts from the 2022 STD Prevention Conference Oral Session 1: Molecular Detection of Neisseria gonorrhoeae Antimicrobial Resistance and STI Strain Characterization. September 19, 2022. View episode transcript and download the Sexually Transmitted Diseases October 2022 issue at www.std.uw.edu.This podcast is dedicated to an STD [sexually transmitted disease] review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs. Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW) and Medical Director of the Public Health – Seattle & King County Sexual Health Clinic.
On episode #21 of the Infectious Disease Puscast, Daniel and Sara review the infectious disease literature for the previous two weeks, 1/18/23 – 2/1/23. Hosts: Daniel Griffin and Sara Dong Subscribe (free): Apple Podcasts, Google Podcasts, RSS, email Become a patron of Puscast! Links for this episode The impact of cold temperature in the pattern of influenza virus infection (OFID) Janssen to discontinue Phase 3 Mosaico HIV vaccine clinical trial (JNJ) Randomized trial of vaccines for Zaire Ebola virus disease (NEJM) PD-1 blockade and lenalidomide combination therapy for Epstein-Barr virus infection (CMI) Outcomes of Daptomycin plus Ceftaroline vs alternative therapy for persistent MRSA bacteremia (IJAA) Detection of a novel strain of multidrug-non-susceptible Neisseria gonorrhoeae (The Lancet) Impact of a device to reduce blood culture contamination and false-positive central-line bloodstream infections (ICHE) Addition of anaerobic coverage for treatment of biliary tract infections (JAC) High dose Cefepime vs Carbapenems for bacteremia caused by Enterobacterales(OFID) Assessing the diagnostic performance of IGRAs for Mycobacterium tuberculosis (CID) Infective endocarditis after transcatheter aortic valve replacement (JACC) Discordant clinical and microbiological outcomes are associated with late clinical relapse in clinical trials for complicated UTIs (CID) Real-world use of bezlotoxumab and fecal microbiota transplantation for the treatment of Cdiff (OFID) Blastomycosis in New England (OFID) Management of invasive candidiasis in hematopoietic cell transplant recipients (TCT) Short course of Antifungal therapy in patients with uncomplicated Candida Bloodstream infection (OFID) Parasites and childhood stunting (Cell) Comparing complication rates of midline catheter vs. PICC line (OFID) Novel prion strain as the cause of chronic wasting disease in a moose (EID) Agreement of respiratory viruses' detection between nasopharyngeal swab and bronchoalveolar lavage in adults with pneumonia (CMI) Music is by Ronald Jenkees
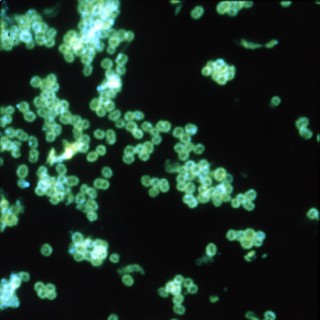
3.12 Neisseria Species Microbiology review for the USMLE Step 1 exam Neisseria species are gram negative diplococci that infect and live inside neutrophils Two main species that cause infections in humans: Neisseria gonorrhoeae and Neisseria meningitidis Neisseria gonorrhoeae causes the sexually transmitted infection gonorrhea, which is the second most common STI Risk factor for gonorrhea is unprotected sex with an infected person N. gonorrhoeae uses pilli to adhere to epithelial cells and invade, causing a local skin infection at the site of inoculation Females: cervix is the most common site of infection, causes cervicitis, symptoms include thick yellow or green vaginal discharge, dysuria, and pelvic pain. If left untreated, it can cause PID, ectopic pregnancy, infertility, and chronic pelvic pain Males: urethra is the most common site of infection, symptoms include yellow-green discharge, dysuria, and painful swollen testes (less common) If left untreated, it can infect more proximal structures and cause prostatitis Diagnosis is done by swabbing the urethra or cervix and sending it for nucleic acid amplification testing Can also cause septic arthritis (in contrast, Chlamydia causes reactive arthritis) "Gonorrhea gon go to the joints" Treatment typically involves a cephalosporin (like ceftriaxone) and azithromycin to also cover chlamydial infection Conjunctival gonorrhea can occur in newborns during the birthing process, causing conjunctivitis in the eye.
Dr. John Toney, Professor of Medicine at the USF Morsani College of Medicine, presents this STI treatment refresher updated for 2022-2023. Dr. Toney begins by reviewing the new changes to the latest 2021 STI guidelines (updated from 2015). He next discusses Chlamydia and Neisseria, Chancroid and LGV. Next, he discusses syphilis. Topics discussed related to syphilis includes differentiating primary, secondary, and latent disease, diagnostic testing and treatment. Dr. Toney closes by discussing genital Herpes and Trichomoniasis.
3.04 Gram Negative Bacteria Microbiology review for the USMLE Step 1 Exam. Gram negative bacteria are characterized by a thin cell wall surrounded by a lipid outer membrane They do not retain the violet gram stain and appear pink after staining Gram negative bacteria can be classified by shape: cocci, coccobacilli, bacilli, and spirals Gram negative cocci include Neisseria species, which can be further categorized as maltose fermenters or non maltose fermenters Gram negative coccobacilli include: Bordetella pertussis, Haemophilus influenzae, Pasteurella, Francisella tularensis, Brucella, and Acinetobacter Gram negative bacilli can be divided into lactose fermenting and non lactose fermenting categories Lactose fermenting gram negative bacilli include: Escherichia coli, Klebsiella, Enterobacter, Citrobacter, and Serratia Non lactose fermenting gram negative bacilli can be further divided into oxidase positive and oxidase negative Oxidase positive non lactose fermenting gram negative bacilli include Pseudomonas Oxidase negative non lactose fermenting gram negative bacilli include Shigella, Yersinia, and Salmonella Gram negative spirals can be divided into oxidase positive and oxidase negative categories Oxidase positive gram negative spirals include Vibrio species, Helicobacter pylori, and Campylobacter jejuni Oxidase negative gram negative spirals include Borrelia burgdorferi (cause of lyme disease) and Treponema pallidum (cause of syphilis)
The Best Clinical Microbiology Papers of 2022 (JCM Ed.)
As we enter into the holiday season, many of us look forward to celebrating long-standing traditions with family and friends, which is no different from us here on the podcast! While not necessarily as long-standing as some of the other classic holiday traditions, after 2.5 years on air, we on this podcast have established our own end-of-year tradition, which is to take a look back at some of our favorite papers or more intriguing manuscripts published in the Journal of Clinical Microbiology over the past year. And so as you'll see, thanks to the different areas of expertise and general interest among our panel today, we've selected quite a variety of papers to discuss, ranging from evaluation of new blood culture systems to use of metagenomics for infective endocarditis and to the potential application of interferon gamma release assays for detection of Histoplasma infections. And so, suffice it to say, there will be something of interest for everyone listening. But, for those watching today, you are clearly getting an extra special treat as you get to see us do this episode wearing our best holiday gear and accessories. Guest: Dr. Trish Simner. Links: Nasal Swab Performance by Collection Timing, Procedure, and Method of Transport for Patients with SARS-CoV-2. DOI: https://doi.org/10.1128/JCM.00569-21 Multicenter Postimplementation Assessment of the Positive Predictive Value of SARS-CoV-2 Antigen-Based Point-of-Care Tests Used for Screening of Asymptomatic Continuing Care Staff. DOI: https://doi.org/10.1128/JCM.01411-21 Laboratory Safety: Handling Burkholderia pseudomallei Isolates without a Biosafety Cabinet. DOI: https://doi.org/10.1128/JCM.00424-21 The clinical utility of 2 high-throughput 16S rRNA gene sequencing workflows for taxonomic assignment of unidentifiable bacterial pathogens in MALDI-TOF MS. DOI: https://doi.org/10.1128/JCM.01769-21 Performance of Fully Automated Antimicrobial Disk Diffusion Susceptibility Testing Using Copan WASP Colibri Coupled to the Radian In-Line Carousel and Expert System. DOI: 10.1128/JCM.00777-21 Benefits Derived from Full Laboratory Automation in Microbiology: A Tale of Four Laboratories. DOI https://doi.org/10.1128/JCM.01969-20 Reflex Detection of Ciprofloxacin Resistance in Neisseria gonorrhoeae by Use of the SpeeDx ResistancePlus GC Assay. DOI: https://doi.org/10.1128/JCM.00089-21 Comparative Performance of Latest-Generation and FDA-Cleared Serology Tests for the Diagnosis of Chagas Disease. DOI: https://doi.org/10.1128/JCM.00158-21 Diagnosing Pulmonary Tuberculosis by Using Sequence-Specific Purification of Urine Cell-Free DNA. DOI: https://doi.org/10.1128/JCM.00074-21 Indeterminate QuantiFERON Gold Plus Results Reveal Deficient Interferon Gamma Responses in Severely Ill COVID-19 Patients. DOI: https://doi.org/10.1128/JCM.00811-21 Visit journals.asm.org/journal/jcm to read articles and/or submit a manuscript. Follow JCM on Twitter via @JClinMicro
Educational Pearls: Most common sexually transmitted disease (STD) in North America: Human Papillomavirus (HPV) From the emergency department patients should be connected to follow-up care and educated on vaccine series Most common non-viral STD in North America: Trichomonas Vaginalis While men may be asymptomatic, they can transmit the disease to women who may experience irritation leading to increased likelihood of PID and contraction of other STDs and HIV Trichomonas is diagnosed via wet preparation with visualization of motile parasites Similarly, men's urine can be tested for visualized motile parasites Expedite lab as parasites are motile for about one hour PCR test is becoming more available Most common bacterial STD in North America: Chlamydia trachomatis Neisseria gonorrhoeae is a less common bacterial STD but does have high rates of drug resistance Empiric STD treatment includes IM Ceftriaxone and PO Doxycycline Providers should consider adding Flagyl for Trichomonas Vaginalis coverage ReferencesSexually transmitted disease surveillance, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/std/statistics/2020/default.htm. Published August 22, 2022. Accessed November 21, 2022. Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187. Published 2021 Jul 23. doi:10.15585/mmwr.rr7004a1 Summarized by Kirsten Hughes, MS4 | Edited by John Spartz, MD, & Erik Verzemnieks, MD In an effort to promote diversity, equity, and inclusion in Emergency Medicine, The Emergency Medical Minute is proud to present our 2nd annual Diversity and Inclusion Award. We support increasing the representation of underrepresented groups in medicine and extend this award to individuals applying to emergency medicine residencies during the 2022-2023 cycle. For information on award eligibility and the application process, visit https://emergencymedicalminute.com/edi-award/ Donate to EMM today!
Dr. Carole Keim MD takes listeners through vaccines in today's episode. She explains everything from how vaccines are created to common myths and misconceptions about them. She then details each baby and childhood vaccine, and what disease each prevents.Dr. Keim breaks down how vaccines work and what criteria they must meet in disease to be effective. She explains the four main types of vaccines and lays each vaccination out in a clear manner, covering what age your baby or child will be when they receive the vaccine and how the immune response works. These vaccines are proven to protect your baby against everything from tetanus to mumps to pertussis and more.This episode will cover: How vaccines workCriteria to create a vaccineThe 4 different types of vaccinesCommon myths or misconceptions about vaccinesSpecific vaccines (all routine childhood vaccines)Total number of vaccinesCommon side effects and red flags, how to treat How vaccines work: 00:44The purpose of vaccines is to trigger an immune response faster and with less harm than the original disease.The immune system is a lot like a microscopic team of superheroes, made up of white blood cells, antibodies, the complement system, and a few others. These superheroes fight villains such as bacteria, viruses, and other pathogens. If they cannot fight them fast enough, the villains will multiply and cause symptoms of disease. Vaccines give your superhero team information about what the villains look like, so they can recognize them as soon as they enter the body, and fight them off quicker and easier.Vaccine criteria: 01:26In order to make a vaccine, certain conditions must be metIt has to be effective. We must be able to become immune to the pathogen; diseases like RSV and HFM are ones we can catch multiple times. Chickenpox is one that you become immune to after catching it once.The pathogen must not be able to mutate faster than the vaccine can be given - we do flu boosters annually because the flu virus mutates about that often. HIV and common cold mutate too fast for a vaccine to be developed.The vaccine must be cost-effective; it has to be cheaper to prevent the disease than to treat itThere are 4 main types of vaccines: 02:31Inactivated (killed pathogens)Live attenuated (weakened pathogens)Toxoid (a piece of what's inside the pathogen)mRNA vaccines Inactivated vaccines 03:44Most common typeThe bacteria or viruses in the vaccine are killed, so your immune system can safely learn to recognize the pathogen that it is trying to fight off. These vaccines do not have the potential to cause actual disease. What they do is cause the immune system superheroes to practice fighting the villains, kind of like practicing on dummies, which may cause mild signs of illness - fever, sore muscles, crankiness, or other symptoms. Examples: IPV (polio), HPV (human papillomavirus), HiB (Haemophilus influenzae B), pneumococcus (Streptococcus pneumoniae), meningococcus (Neisseria meningitidis), and Hepatitis A and B vaccines.Live attenuated vaccines 04:02Made from bacteria or viruses that have been exposed to chemicals that make them weaker than the natural or “wild type” bacteria or virus. Since these pathogens are not killed completely, your superheroes aren't just practicing on dummies, they are actually fighting the weakened villains. So it is possible to have symptoms of the disease, but milder. Some people with weakened immune systems may not be able to fight them off, and can get the actual disease. People taking steroid medications or immune suppressants, or who have HIV or other immune deficiencies should consult a doctor about whether it is safe to receive these vaccines. Examples: oral polio vaccine, MMR (measles, mumps, and rubella), Varicella zoster (chickenpox), and rotavirus vaccines.Toxoid vaccines 04:55Made from just part of the pathogen, and protect against the kinds of bacteria that cause symptoms after the toxins inside them are released. These toxin-carrying bacteria are like villains carrying around a bottle of poison, and the toxoid vaccine gives the superheroes the poison to sample and build up resistance to it. Example: DTaP (diphtheria, tetanus, and acellular pertussis).MRNA vaccines 05:23Newest typemRNA is like a copy of instructions. These give your immune system something like a sewing pattern to print out and make the dummies for your body to fightExample: some COVID vaccinesMyths and misconceptions about vaccines: 05:45Many parents have concerns about vaccinating their children. It only takes one serious reaction to call into question the safety of vaccines. And it has been so long since the vaccine-preventable diseases have run rampant that we in the United States don't fully understand the scope of what is being prevented. Here are some of the top concerns that I have heard from parents, and the truth behind them.Aluminum. There is aluminum in vaccines, but the amount is far less than babies get from other sources. The total amount of aluminum that babies get from vaccines in the first 6 months is 4.4mg. Breastfed babies consume 7mg, formula-fed babies consume 38mg, and babies on soy formula consume 114mg of aluminum in the first 6 months of life. Consuming aluminum vs. having it injected in a vaccine looks the same to the body, so the tiny amount of aluminum in vaccines will not harm your babyAntigens. An antigen is any microscopic substance that has the possibility to elicit an immune response. Babies are exposed to over a trillion antigens in the first year that naturally occur in the environment. The entire vaccine series that children receive today contains just over 150 antigens. A young baby's immune system can easily recognize these few antigens and make antibodies to the diseases without getting sick.Autism. It has been proven that vaccines do NOT cause autism. The age that children first start showing signs and can be tested for autism is 15-24 months. This is the same age that children receive booster vaccines, so it is understandable that some parents think they are related. Long-term protection. Vaccines will protect a person for just as long as if they got the original disease. So a person who had chickenpox as a child is just as protected from getting it again as a person who has received the chickenpox vaccine. Some people do not seroconvert (develop antibodies to that disease) - that depends on their immune system and is not a failure of the vaccine itself.Mercury. There used to be a preservative called thimerosal in vaccines. That preservative (which contains mercury) has been removed from all vaccines in the US that children receive. The only vaccine that still contains thimerosal is the adult flu vaccine.Unnatural exposure. Some people worry that getting exposed to a disease through an injection is not the same as getting it “naturally” by being exposed to a sick person. This is not true; any disease will get into your bloodstream, which is where it is recognized by the body, and once in there the body has no idea how it got in. So getting an injection looks exactly the same to your immune system as getting the disease from a sick person.Doctors DO NOT get paid to vaccinate childrenVaccines are NOT a punishment for children who are behaving badlySpecific vaccines: 10:47Hep B - 0, 2, 6 mos. Hepatitis B is a viral infection that can be passed from mom to baby through the placenta or during delivery. 90% of babies born with HepB will develop chronic infection and are at risk of liver cancer later in life.DTaP - 2, 4, 6, 15 mos, 4 years. Tdap - age 11, every 10 years. DTaP has more diphtheria, Tdap has more tetanus. Bacterial infections. Diphtheria causes severe sore throat and enlarged tonsils, and can block the airway from swelling/tonsils being so enlarged. Tetanus makes spores that live in soil; any penetrating wound could have tetanus in it (nail/thumbtack, dog or cat bite) and tetanus is not killed by antibiotics so it must be prevented. Pertussis is whooping cough and causes babies less than a year old to stop breathing. Everyone who takes care of the baby should be current on their TDaP (within 10 years). Polio - 2, 4, 6 mos, 4 years. Polio is a virus that attacks nerves and causes paralysis. Sometimes it's minor, and sometimes it's the diaphragm that's affected and they stop breathing. There is no specific treatment for polio.HiB - 2, 4, 6, 12-18 mos. HiB (haemophilus influenzae B) bacterial infection that affects children less than 5 years, and especially those under 1 year of age. It used to cause severe infections like epiglottitis, sepsis, pneumonia, and meningitis. PCV - 2, 4, 6, 12-18 mos. PCV = pneumococcal conjugate vaccine, pneumococcus is another name for streptococcus pneumonia, which is a kind of strep that gets into the bloodstream and causes sepsis, pneumonia, and meningitis. PCV has 13 strains of strep in it right now.Rotavirus - 2, 4, 6 mos. Viral infection that causes severe diarrhea and dehydration in babies. Hep A - 12 and 18 mos. Hep A is a type of food poisoning, there's no specific treatment. MMR - 1 and 4 years. Measles causes high fever, rash, and can cause brain damage, hearing loss, and death. Mumps causes parotitis (infection of salivary glands), but in boys also causes orchitis (inflammation of testicles) and can lead to sterility. Rubella is a fever and rash; more dangerous to unborn babies, causes miscarriages and birth defects.VZV - 1 and 4 years. Varicella Zoster virus (chickenpox) causes cold symptoms, fever, and an itchy and painful rash in children, and shingles in adults. VZV in pregnancy causes miscarriages and birth defects.MCV - 11 and 16 years. Meningitis A, C, W, Y are viruses that cause inflammation around the brain that develops quickly and can be fatal. HPV - 11 years. Human papilloma virus causes warts and dysplasia and can lead to cancer of the mouth, throat, anus, cervix, and penis. Currently 9 strains of HPV in the vaccine. Flu: recommended annually COVID: recommendations are still evolvingVaccines that are available but not given routinely: MenB, PPSV23, Dengue, Typhoid, japanese encephalitis, yellow fever, rabiesTotal numbers of vaccines: 22:351 at birth (Hep B)2 mos: DTaP, polio, HiB, Hep B, PCV, rotavirus - 1 or 2 combo vaccines, PCV and rota = 2 or 3 shots plus an oral vaccine4 mos: DTaP, polio, HiB, PCV, rotavirus - 1 combo plus PCV and rota = 2 shots and one oral6 mos: DTaP, polio, HiB, Hep B, PCV, rotavirus - 1 or 2 combo vaccines, PCV and rota = 2 or 3 shots plus an oral vaccine6+ mos: flu vaccine annually12-18 mos: 2 doses Hep A, 1 of DTaP, HiB, PCV, MMR, VZV. 5-7 shots depending on combos.4-6 years: DTaP, polio, MMR, VZV, typically given as 2 combo vaccines11 years: Tdap, MCV, 2 doses HPV16 years: MCV21+ years: Tdap every 10 years; booster if you have a wound and it's been less than 5 years, booster while pregnant9 shots and 3 oral before 1 year of age, 5-7 shots from age 1-2, 2 shots age 4-6, 4 at age 11, 1 at age 16 = 21-23 total shots before adulthood. 18 flu shots. Common vaccine reactions: 23:53Birth: nothing; sometimes redness/swelling2-6 mos: redness and swelling (local reaction), can be as much as the entire thigh and still be considered normal. Low grade fevers.12-18 mos and 4-6 years: muscle soreness, MMR and VZV cause fevers, VZV sometimes causes rash, other vaccines can cause local reactions11yrs: muscle soreness, local reaction with Tdap and MCV, fainting with HPV16 yrs: local reaction from MCVTdap boosters: muscle sorenessFlu, COVID: flu-like symptomsIt is NOT normal to have a body rash or vomiting after vaccines; those are signs of allergyLarge local reactions and muscle soreness can be treated with cool compresses (wet washcloth) and/or acetaminophen or ibuprofen. Fever or flu-like symptoms: acetaminophen or ibuprofenI DON'T recommend pre-medicating your child before vaccinesIf your child has an adverse reaction to a vaccine, you should report it to VAERS (vaccine adverse event reporting system). Remember that VAERS is like Yelp for vaccines, so take that about as seriously as you would a Yelp review.All of this information is also in The Baby Manual book, which is available for purchase. Remember it is always okay to call your doctor or emergency services if you have concerns about your baby's health. Resources discussed in this episode:The Baby Manual - Available on AmazonVAERS--Dr. Carole Keim MD: linktree | tiktok | instagram
The Centers for Disease Control and Prevention just updated guidelines for sexually transmitted infections (previously sexually transmitted diseases) for everything by HIV. In this multi-part series, host Geoff Wall will break down what's new and what's changing in practice.The GameChangerA 7-day course of doxycycline in the treatment of urogenital chlamydia is preferred and has been shown to be more efficacious compared to azithromycin. Ceftriaxone should be the treatment of choice for gonorrhea as there have been no “resistance”-related treatment failures identified in the United States at any anatomical site. Show Segments00:00 – Introduction01:45 – STI Guidelines02:34 – Chlamydia 14:56 – Gonorrhea 28:57 – Closing RemarksHost Geoff Wall, PharmD., BCPS, FCCP, CGP Professor of Pharmacy Practice, Drake University Internal Medicine/Critical Care, UnityPoint Health All relevant financial relationships have been mitigated. References and Resources CDC Sexually Transmitted Infections Treatment Guidelines, 2021Redeem your CPE or CMECPE (Pharmacist)CME (Physicians) Get a membership & earn CE for GameChangers Podcast episodes (30 mins/episode)Pharmacists: Get a membershipPrescribers: Get a membership CE Information Learning Objectives Describe the treatment of Neisseria gonorrhea based on the 2021 recommendationsDiscuss pharmacotherapy options for patients with chlamydia with or without concomitant gonorrhea infections0.05 CEU/0.5 Hr UAN: 0107-0000-22-224-H01-P Initial release date: 06/062022 Expiration date: 06/06/2023 Additional CPE and CME details can be found here.
Episode 89: Gonorrhea Basics. Written by Robert BensacenezRobert, Dr. Schlaerth, and Dr. Arreaza discuss the basics of gonorrhea, including presentation, treatment, and even a potential gonococcal vaccine.Introduction: Gonorrhea is commonly known as “the clap” or “the drip”. This ancient disease, described as “the perilous infirmity of burning” in a book called The History of Prostitution, has been treated with many remedies throughout history, including mercury, sulfur, silver, multiple plants, and even gold. Today we will discuss the clinical features, diagnosis, and current therapy of gonorrhea. By the way, did you know that gonorrhea in Spanish is used as an insult in Colombia? Well, now you know it. Definition: Gonorrhea is a sexually transmitted disease caused by the bacterium Neisseria gonorrhoeae (common name gonococcus), which is a gram-negative, intracellular, aerobic, diplococci. This disease leads to genitourinary tract infections such as urethritis, cervicitis, pelvic inflammatory disease (PID), and epididymitis. This is Rio Bravo qWeek, your weekly dose of knowledge brought to you by the Rio Bravo Family Medicine Residency Program from Bakersfield, California. Our program is affiliated with UCLA, and it's sponsored by Clinica Sierra Vista, Let Us Be Your Healthcare Home. ___________________________Gonorrhea. Written by Robert Besancenez, MS4, Ross University School of Medicine. Moderated and edited by Hector Arreaza, MD. Discussion participation by Katherine Schlaerth, MD. Epidemiology: The disease primarily affects individuals between 15–24 years of age (half of the STI patients in the US). CDC estimates that approximately 1.6 million new gonococcal infections occurred in 2018. Incidence rates are highest among African Americans, American Indians, and Hispanic populations.Transmission is sexual (oral, genital, or anal) or perinatal (causing gonococcal conjunctivitis in neonates). Risk factors include unsafe sexual behaviors (lack of barrier protection, multiple partners, men who have sex with men (MSM), and asplenia, complement deficiencies. Individuals with low socioeconomic status are at the highest risk: poor access to medical treatment and screening, poor education, substance use, and sex work. Presentation: The incubation period is ~ 2–7 days, and sometimes patients do not develop any symptoms. Urogenital infection: Gonorrhea is commonly asymptomatic, especially in women, which increases the chance of further spreading and complications. When symptoms are present, typical symptoms include purulent vaginal or urethral discharge (purulent, yellow-green, possibly blood-tinged). Discharge is less common in female patients. Urinary symptoms include dysuria, urinary frequency, and urgency. Male: - Typical presentation is urethritis. - Penile shaft edema without other signs of inflammation.- Epididymitis: unilateral scrotal fullness sensation, scrotal swelling, redness, tenderness, relief of pain with elevation of scrotum —Prehn Sign— and positive cremasteric reflex.- Robert: Prostatitis: fever, chills, general malaise, pelvic or perineal pain, cloudy urine, prostate tenderness (examine prostate gently). Female: - Cervicitis: Friable cervix and discharge (purulent, yellow, malodorous), - PID: pelvic or lower abdominal pain, dyspareunia, fever, cervical discharge, cervical motion tenderness but also uterine or adnexal tenderness, abnormal intermenstrual bleeding. PID can be subclinical and diagnosed retroactively when tubal occlusion is discovered as part of a workup for infertility. PID can cause Fitz-Hugh-Curtis syndrome (perihepatitis with RUQ pain).- Bartholinitis presents with introitus pain, edema, and discharge from the labia. - Vulvovaginitis may occur but is rare (due to the tissue preference of gonococci)Extragenital infection: Proctitis: Rectal purulent discharge, possible anorectal bleeding and pain, rectal mucosa inflammation, or rectal abscess (less common).Pharyngitis: sore throat, pharyngeal exudate, cervical lymphadenitis. Disseminated gonococcal infection (DGI): Triad of arthritis, pustular skin lesions, and tenosynovitis. As mentioned in Episode 46, on December 23, 2020, the California Department of Public Health (CDPH) sent a “Dear Colleague” letter to warn the medical community about the increased cases of DGI in California and Michigan. Increased cases may be caused by decreased STD testing and treatment because of the COVID-19 pandemic, and not necessarily because of a more virulent strain of gonorrhea. Later, treatment of gonorrhea was updated because of resistance. Epidemiology: ∼ 2% of cases. Most common in individuals younger than 40 years old, the female to male ratio is 4:1. A history of recent symptomatic genital infection is uncommon. Asymptomatic infections increase the risk of dissemination due to delayed diagnosis and treatment. Clinical features: Two distinct clinical presentations are possible. Arthritis-dermatitis syndrome:Polyarthralgias: migratory, asymmetric arthritis that may become purulent.Tenosynovitis: simultaneous inflammation of several tendons (e.g. fingers, toes, wrist, ankle).Dermatitis: vesicular, pustular, or maculopapular lesions, possibly with a necrotic or hemorrhagic center. Most commonly distributed on the trunk, extremities (sometimes involving the palms and soles). Typically, < 10 lesions with a transient course (subside in 3–4 days). Additional manifestations: fever and chills (especially in the acute phase). Purulent gonococcal arthritis: Abrupt inflammation in up to 4 joints (commonly knees, ankles, and wrists). No skin manifestations, rarely tenosynovitis. Genitourinary manifestations in only 25% of affected individuals. Not to be confused with reactive arthritis. Health care providers living in California: Order Nucleic acid amplification test (NAAT) and culture specimens from urogenital, extragenital mucosal sites (e.g., pharyngeal and rectal), and from disseminated sites (e.g., skin, synovial fluid, blood, and cerebrospinal fluid) before initiating empiric antimicrobial treatment for patients with suspected DGI. Report within 24 hours of diagnosis to the California Department of Public Health. Complications of DGI: sepsis with endocarditis, meningitis, osteomyelitis, or pneumonia. Diagnosis of gonorrhea: The test of choice is Nucleic acid amplification testing (NAAT) of first-catch urine or swabs of urethra, endocervix and pharynx, and synovial fluid in disseminated infection. Other possible tests: gram stains and bacterial cultures (Thayer-Martin agar, useful for antibiotic resistance, results may take 48 hours, sensitivity is lower than NAAT.)Synovial fluid analysis: Appearance of fluid can be clear or cloudy (purulent), high Leukocyte count (up to 50,000 cells/mm3): especially segmented neutrophils, gram stain positive in < 25% of cases. Treatment: Ceftriaxone and doxycycline for uncomplicated cases, but may require different approaches in case of allergies or intolerance to these antibiotics, or in severe cases. Uncomplicated gonorrhea (affecting cervix, urethra, rectum, pharynx)First-line treatment: single-dose ceftriaxone 500 mg IM (1 G for patients >150 Kg) PLUS doxycycline 100 mg PO twice a day for 7 days If a chlamydial infection has not been excluded.During pregnancy: Ceftriaxone PLUS single-dose azithromycin 1 gram PO(doxy is contraindicated – teratogen) Complicated gonorrhea (salpingitis, adnexitis, PID/ epididymitis, orchitis)Single-dose ceftriaxone IM PLUS doxycycline PO for 10–14 days (women may require additional administration of Metronidazole PO for 14 days). DGICeftriaxone IV every 24 hours for 7 days In case Chlamydia infection has not been ruled out: PLUS doxycycline PO twice a day for 7 daysDrainage of purulent joint(s) Sequelae: Without treatment, a prolonged infection may lead to complications, such as hymenal and tubal synechiae that lead to infertility in women. Prevention:-Screening for gonorrhea (USPSTF recommendations, September 2021, Grade B): Annual NAAT screening of gonorrhea AND chlamydia for sexually active women ≤ 24 years (including pregnant persons) or > 25 years with risk factors (e.g. new or multiple sex partners, sex partner with an STI, etc.). Evaluate for other STIs if positive (e.g. chlamydia, syphilis, and HIV). There is insufficient evidence to recommend for or against screening gonorrhea in asymptomatic males (Grade I).In all patients: Evaluate and treat the patient's sexual partners from the past 60 days. Provide expedited partner therapy if the timely evaluation of sexual partners is not feasible. Single-dose cefixime PO (if chlamydia has been excluded in the patient) OR Single-dose cefixime PO PLUS doxycycline PO for 7 days. Sexual partners must be treated simultaneously to avoid reinfections. A possible gonococcal vaccine: A gonococcal vaccine is theoretically possible, let's remember that the meningococcal vaccine exists. Meningococcus is closely related to gonococcus. A study published in 2017 showed that MeNZB® (a vaccine used in New Zealand until 2011 to fight against a meningitis epidemic) provided partial protection against gonorrhea. Food for thought for you guys. Conclusion: Let's remember to screen asymptomatic women for gonorrhea, identify symptomatic patients and start treatment promptly, and prevent serious complications, and more importantly, let's promote safe sex practices to prevent this disease.Now we conclude our episode number 89 “Gonorrhea Basics”. Gonorrhea affects mainly the urogenital area, but it can spread to the pharynx, rectum, skin, and even joints. When you see septic arthritis in patients with high risk for gonorrhea, suspect disseminated gonococcal infection and start treatment promptly. Even without trying, every night you go to bed being a little wiser.Thanks for listening to Rio Bravo qWeek. If you have any feedback about this podcast, contact us by email at RioBravoqWeek@clinicasierravista.org, or visit our website riobravofmrp.org/qweek. This podcast was created for educational purposes only. Visit your primary care physician for additional medical advice. This week we thank Hector Arreaza, Robert Besancenez, and Katherine Schlaerth. Audio edition: Suraj Amrutia. See you next week! _____________________References:Seña, Arlene C, MD, MPH; and Myron S Cohen, MD. Treatment of uncomplicated Neisseria gonorrhoeae infections, UpToDate, updated on Jan 27, 2022. Accessed on April 5, 2022. https://www.uptodate.com/contents/treatment-of-uncomplicated-neisseria-gonorrhoeae-infections Ghanem, Khalil G, MD, PhD. Clinical manifestations and diagnosis of Neisseria gonorrhoeae infection in adults and adolescents, UpToDate, updated on Sep 17, 2021, accessed on April 5, 2022. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-neisseria-gonorrhoeae-infection-in-adults-and-adolescents Klausner, Jeffrey D, MD, MPH. Disseminated gonococcal infection, UpToDate, updated on March 3, 2022. Accessed on April 5, 2022. https://www.uptodate.com/contents/disseminated-gonococcal-infection Petousis-Harris H, Paynter J, Morgan J, et al. Effectiveness of a group B OMV meningococcal vaccine on gonorrhea in New Zealand – a case control study. Abstract presented at: 20th International Pathogenic Neisseria Conference. Manchester, UK; 2016.
This episode features an interview with Dr. Charlene Kahler from the Marshall Centre for Infectious Diseases Research and Training at the University of Western Australia. She discusses and article titled "Neisseria species and their complicated relationships with human health". Tune in to this episode to find out more information about different species of Neisseria and their significance in the human body.Link to article: https://www.publish.csiro.au/ma/fulltext/ma21024
In this episode Jame and Callum talk through the two most medically important Gram negative cocci: Neisseria meningitidis and Neisseria gonorrhoeae.Send suggestions to idiotspodcasting@gmail.com
Development of an effective vaccine against Neisseria gonorrhoeae has been difficult, but there has been recent progress in the field. This episode will cover some updates published in the literature on this topic. View episode transcript and references at www.std.uw.edu.Editor and host Dr. Meena Ramchandani is an Assistant Professor of Medicine at the University of Washington (UW) and Medical Director of the Public Health – Seattle & King County Sexual Health Clinic. This podcast is dedicated to an STD [sexually transmitted disease] literature review for health care professionals who are interested in remaining up-to-date on the diagnosis, management, and prevention of STDs
Cabello, R. R., Feregrino, R. R., & Feregrino, R. R. (2018). Microbiología y parasitología humana: Bases etiológicas de las enfermedades infecciosas y parasitarias. Editorial Médica Panamericana. --- Send in a voice message: https://anchor.fm/las-poderosas-celulas-nk/message
Gonorrhea: An unusual, accidental and non-sexual case with Prof. Felicity Goodyear-Smith
In a recent article published in the Journal of Medical Case Reports, the authors report the unusual case of a girl diagnosed with Neisseria gonorrhoeae after bathing in a heavily frequented hot pool at the edge of the crater lake Specchio di Venere (“Mirror of Venus”) on Pantelleria Island, Italy. Joining me today to discuss the case is Professor Felicity Goodyear-Smith. Dr. Goodyear Smith is with the Department of General Practice & Primary Health Care, University of Auckland and coauthor of the case report. Gonococcus infection probably acquired from bathing in a natural thermal pool: a case report https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-021-03043-6
Neisseria gonorrhoeae is the second most common bacterial sexually transmitted infection in the world, and it has become a superbug. It has developed resistance to every antibiotic currently approved for treatment, and multidrug-resistant strains have been identified globally. Hear from clinicians advocating for their patients, a global leader, and a leading expert in drug development on actions needed to combat resistant gonorrhea. Learn more about our guests this episode: Teodora Wi: https://www.who.int/campaigns/world-antimicrobial-awareness-week/2018/features-from-around-the-world/super-gonorrhoea-q-a-with-dr.-teodora-wi Matthew Hamill: https://www.hopkinsmedicine.org/profiles/details/matthew-hamill Yuka Manabe: https://www.hopkinsmedicine.org/profiles/details/yukari-manabe Edward Hook: https://apps.medicine.uab.edu/FacultyDirectory/FacultyData.asp?FID=7333 This podcast is co-created by CIDRAP-ASP and the Antimicrobial Resistance Fighter Coalition (ARFC). Theme music Artist: Derek Sandbeck Song Title: Power Plugs & Superbugs
Contributor: Peter Bakes, MD Educational Pearls: Ophthalmia Neonatorum encompasses any conjunctivitis that presents within the first 28 days of life Neonates often receive prophylactic silver nitrate eye drops for gonorrhea prophylaxis, but the drops can cause chemical conjunctivitis Etiology & Timing of Presentation: Silver nitrate conjunctivitis presents 0-2 days after birth Neisseria gonorrhae presents 2-5 days after birth Chlamydia trachomatis presents 5 days to 5 weeks Neisseria gonorrhoeae conjunctivitis is vision-threatening, typically requiring admission and IV antibiotics with a 3rd generation cephalosporin References Castro Ochoa KJ, Mendez MD. Ophthalmia Neonatorum. [Updated 2021 Jul 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551572/ US Preventive Services Task Force, Curry SJ, Krist AH, et al. Ocular Prophylaxis for Gonococcal Ophthalmia Neonatorum: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA. 2019;321(4):394-398. doi:10.1001/jama.2018.21367 Summarized by John Spartz, MS4 | Edited by Erik Verzemnieks, MD The Emergency Medical Minute is excited to announce that we are now offering AMA PRA Category 1 credits™ via online course modules. To access these and for more information, visit our website at https://emergencymedicalminute.org/cme-courses/ and create an account. Donate to EMM today! Diversity and Inclusion Award
In Season 2 of Superbugs and You, we continue to focus on the threat of antimicrobial resistance, which occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to antibiotics and other medicines. In other words, they become “Superbugs”. This season, we will focus on Methicillin-resistant Staphylococcus aureus, Clostridioides difficile infections, resistant Neisseria gonorrhoeae, and the impact of antimicrobial resistance on modern medicine. Each episode will feature discussions with patients, physicians, and scientists to find out what's causing antimicrobial resistance, how it affects the lives of ordinary people, and most importantly, what we can do to stop it. Subscribe for new episodes beginning on October 20th! This podcast is co-created by the Center for Infectious Disease Research & Policy (CIDRAP) and the Antimicrobial Resistance Fighter Coalition. Visit the CIDRAP Antimicrobial Stewardship Project website: https://www.cidrap.umn.edu/asp Visit the Antimicrobial Resistance Fighter Coalition website: https://antimicrobialresistancefighters.org/ Theme music Artist: Derek Sandbeck Song Title: Power Plugs & Superbugs
Update From the CDC: New Gonorrhea Guidelines - Frankly Speaking Ep 239
Credits: 0.25 AMA PRA Category 1 Credit™ CME/CE Information and Claim Credit: https://www.pri-med.com/online-education/podcast/frankly-speaking-cme-239 Overview: Join us to discuss the CDC's new guidelines for the management of sexually transmitted infections due to Neisseria gonorrhoeae. You'll walk away with recommendations for how to address urogenital, rectal, and pharyngeal infections. You'll also discover alternative regimens for patients allergic to first-line therapy and understand how to manage coinfection with chlamydia. Episode resource links: St. Cyr S, Barbee L, Workowski KA, et al. Update to CDC's Treatment Guidelines for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911–191 Guest: Alan Ehrlich MD, FAAFP Music Credit: Richard Onorato
Update From the CDC: New Gonorrhea Guidelines - Frankly Speaking Ep 239
Credits: 0.25 AMA PRA Category 1 Credit™ CME/CE Information and Claim Credit: https://www.pri-med.com/online-education/podcast/frankly-speaking-cme-239 Overview: Join us to discuss the CDC's new guidelines for the management of sexually transmitted infections due to Neisseria gonorrhoeae. You'll walk away with recommendations for how to address urogenital, rectal, and pharyngeal infections. You'll also discover alternative regimens for patients allergic to first-line therapy and understand how to manage coinfection with chlamydia. Episode resource links: St. Cyr S, Barbee L, Workowski KA, et al. Update to CDC's Treatment Guidelines for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911–191 Guest: Alan Ehrlich MD, FAAFP Music Credit: Richard Onorato
Contributor: Jared Scott, MD Educational Pearls: Recent study evaluated vaginal self swab testing for STIs to determine if they are equally sensitive to provider-obtained swab 515 patients consented to both tests and 95% agreement was found between the two methods of obtaining samples 75% of participants who preferred this over the pelvic exam, although some patients were concerned they did not perform the self swab correctly Consider vaginal self swab with proper coaching as an option for patients References Chinnock B, Yore M, Mason J, et al. Self-obtained vaginal swabs are not inferior to provider-performed endocervical sampling for emergency department diagnosis of Neisseria gonorrhoeae and Chlamydia trachomatis [published online ahead of print, 2021 Jan 18]. Acad Emerg Med. 2021;10.1111/acem.14213. doi:10.1111/acem.14213 Summarized by John Spartz, MS4 | Edited by Erik Verzemnieks, MD The Emergency Medical Minute is excited to announce that we are now offering AMA PRA Category 1 credits™ via online course modules. To access these and for more information, visit our website at www.emergencymedicalminute.org/cme-courses/ and create an account. Donate to EMM today!
SGEM#335: Sisters are Doin’ It for Themselves…Self-Obtained Vaginal Swabs for STIs
Date: June 25th, 2021 Guest Skeptic: Dr. Chris Bond is an emergency medicine physician and assistant Professor at the University of Calgary. He is also an avid FOAM supporter/producer through various online outlets including TheSGEM. Reference: Chinnock et al. Self-obtained vaginal swabs are not inferior to provider-performed endocervical sampling for emergency department diagnosis of Neisseria gonorrhoeae and Chlamydia […]
Meningococcal disease is caused by Neisseria meningitidis, a gram negative diplococcus. The two most common presentations of meningococcal infection are meningococcal meningitis and meningococcaemia. An individual may present with one or both of these. Rapid recognition and treatment is vital, requiring IV antibiotics, but even with treatment, up to 15% of cases result in fatality. Listen in to find out more about meningococcal! Links and resources: Follow us on Instagram @yourekiddingrightdoctors Facebook: https://www.facebook.com/yourekiddingrightpod-107273607638323/ Our email is yourekiddingrightpod@gmail.com Make sure you hit SUBSCRIBE/FOLLOW so you don't miss out on any pearls of wisdom and RATE if you can to help other people find us! (This isn't individual medical advice, please use your own clinical judgement and local guidelines when caring for your patients)
Episode 69: Case Study #8: 16-Year-Old Female Presenting to Clinic with Greenish Vaginal Discharge
A 16-year-old adolescent girl presents to your office with the complaint of greenish vaginal discharge for the past two months and the recent onset of lower abdominal pain. She reports that her last period was about two and a half months ago. She is sexually active with two partners and has never used a condom or any other contraception with either. On physical examination, she is not febrile with normal blood pressure and pulse. She has greenish discharge from the cervix with friability and cervicitis. There is no cervical motion tenderness. Her urine pregnancy test is positive. A cervical sample is positive for chlamydia and negative for Neisseria gonorrhoeae. Her rapid plasma reagin (RPR) is non-reactive and an HIV test is negative. The patient is treated with appropriate antibiotics and counseled concerning safer sex practices. You also inform the patient regarding her risk for HIV conversion, even though today's test was negative. The patient asks if you are going to tell her mother that she is pregnant and has this infection. You inform the patient that because of patient confidentiality and ethical considerations you will not disclose this information to her mother without her consent. She tells you that she does not want her mother and boyfriends to know that she is infected. Be sure to listen until the end when I will be presenting four questions with multiple choice answers and check back on Friday to the May's Anatomy Podcast instagram page for the answers! If you are interested in starting your OWN podcast, but are not sure where to start, try the Operation Podcast Course for 30% off using code "MAY30" Case Files: Family Medicine To try my absolute favorite CBD product line from Cured Nutrition, use code "MAY10" at checkout for 10% off your entire order or simply click the link here Cured Nutrition If you're interested in consuming slow-release caffeinated vanilla or matcha lattes, or if you're a coffee drinker who wants a little more collagen and protein in their diet, use code "MAY15" at checkout for 15% off your entire order or simply click the link here Strong Coffee Use my WearFigs code to get a $20 gift card on purchases of $100+ http://fbuy.me/ofl13 For nursing tips, my experiences, and more musings on the show, follow our Instagram @maysanatomypodcast or follow my personal account @mayyazdi This is an Operation Podcast production. chase@operationpodcast.com
¡Bienvenido Galeno! ⚕ Te invito a que visites mi https://linktr.ee/dra.espinoza para tener acceso a mayor contenido bibliográfico y te sea de mayor utilidad. ¡ÉXITO EN TODO!
Today we'll be covering Innate Immunodeficiencies, going along with this month's theme, Immunology. If you haven't listened to our podcast before, each week we have a case-based discussion about a medical topic to help you study for the pediatric medicine board exam. Episodes are released every weekend, and the case is then reviewed and reinforced on social media throughout the week. Follow the podcast on social media: Facebook- @portablepeds (www.facebook.com/portablepeds) Twitter- @portablepeds (www.twitter.com/portablepeds) We'd love to hear from you via email at portablepeds@gmail.com! Also, feel free to visit our website, www.portablepeds.com, for more content. Today's Case: A 12 year-old male presented to the ED for fever and appearing “very ill” according to his mother. On history, the mother states he has had multiple episodes of skin abscesses, sinusitis, and pneumonia since birth. This patient was subsequently admitted to the PICU and diagnosed with an immunodeficiency in the accelerated phase based on a blood smear showing giant azurophilic granules in neutrophils. Unfortunately, he passed away shortly after admission. Which of the following organisms was likely the cause of this child's death? Neisseria meningitidis Staphylococcus aureus Nocardia Epstein-Barr Virus Aspergillus We would like to give an enormous thank you to Zack Goldmann for designing this podcast's logo and accompanying artwork. You can find more of his work at www.zackgoldmann.com. The intro and outro of this podcast is a public domain song obtained from scottholmesmusic.com. Intro/Outro- Hotshot by Scott Holmes Disclaimer: This podcast is intended for healthcare professionals. The information presented is for general educational purposes only and should NOT be used as professional medical advice or for the diagnosis or treatment of medical conditions. The views and opinions expressed do not represent the views and opinions of our employer or any affiliated institution. Expressed opinions are based on specific facts, under certain conditions, and subject to certain assumptions and should not be used or relied upon for any other purpose, including, but not limited to, the diagnosis or treatment of medical conditions or in any legal proceeding. Full terms and conditions can be found at portablepeds.com. Thanks for listening! As always, please Rate and Review this podcast on Apple Podcasts, Facebook, or your favorite podcasting platform. Also, Subscribe to get all the latest episodes, and Share this episode with someone you think would enjoy it! Hope to see you real soon!
In this episode, we review the high-yield topic of Neisseria meningitidis from the Microbiology section. --- Send in a voice message: https://anchor.fm/medbulletsstep1/message
1- make sure pts follow up on positive FIT test 2. symptom severity — driven particularly by catching/locking and clicking/popping — correlated significantly with the burden of cartilage damage. CARTILAGE DAMAGE!! 3. U.S. Food and Drug Administration announced it is allowing the use of the Binx Health Assay for point-of-care testing for Chlamydia trachomatis and Neisseria gonorrhoeae 4. In patients with atrial fibrillation and a bioprosthetic mitral valve, rivaroxaban was noninferior to warfarin 5. ADHD- “results favored using methylphenidate in children and adolescents, and amphetamines in adults as first-line, short-term (12 weeks or under) treatment.” 6. when it comes to PAD it is true what they say! no pain no gain- but maybe they should say no walking pain less loss and more walking pain much bigger gains in 6minute walking distance The Push for Timely Follow-up After Abnormal At-home Colon Cancer Screening Results | Cancer Screening, Prevention, Control | JAMA | JAMA Network The pandemic has brough on way more things done at home which Is good and bad More stay at home school- bad More stay at home colon cancer screening- good Article talked about a need to make sure pts if positive then get the colonoscopy. Poit out one study where only 44% completed a colonoscopy within 6 months of a positive FIT result even though 89% received a referral, Reasons for the low rates are complex. Patients who are reluctant to get a colonoscopy. and physicians don’t always convey the importance of follow-up. Other factors such as inadequate insurance, lack of transportation, or a facility backlog may be out of a patient’s control. I think in the end we just have to make sure we do our part and while I wouldn’t say scare them make sure they know the importance of this test and how likely it is that they have colon cancer based on it being positive And as a reminder Zorzi M, Hassan C, Capodaglio G, et al. Long-term performance of colorectal cancer screening programmes based on the faecal immunochemical test. Gut 2018;67(12):2124-2130. Over a 10-year period, the rates of detection of colorectal cancer (CRC) and advanced adenomas using fecal immunochemical testing (FIT) are similar to those seen in studies of screening colonoscopy. But how good is it you ask? Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Multitarget Stool DNA Testing for Colorectal-Cancer Screening. N Engl J Med 2014;370(14):1287-1297. FIT was 74% sensitive and 95% specific. Which in pt terms means for every 11 positive FIT there was 1 cancer detected on colonoscopy A positive fit has you down to a 1 in 10 chance of cancer—get the follow up! And speaking of follow up Patient-reported catching or locking of the knee and other “mechanical symptoms” (i.e., popping, clicking, or pain on pivoting) Usually gets a follow up with an ortho surgeon That patient usually goes to get an arthroscopic knee surgery for symptoms attributed to meniscal tears. BUT BUT BUT what if the text book and board question of pain or instabilitiy with (i.e., popping, clicking, or pain on pivoting) Isn’t a meniscus problem at all?? Meniscal and Mechanical Symptoms Are Associated with Cartila... : JBJS (lww.com) Farina EM et al. Meniscal and mechanical symptoms are associated with cartilage damage, not meniscal pathology. J Bone Joint Surg Am 2021 Mar 3; 103:381. (https://doi.org/10.2106/JBJS.20.01193) Researchers prospectively evaluated 565 patients (mean age, 48) who had arthroscopic knee surgery for symptoms connected to meniscus pathology. Pts were asked about the presence and severity of symptoms prior to surgery and then while in surgery, the surgeon recorded characteristics of meniscal tears and the severity of cartilage damage. In the end “We did not observe an association between meniscal pathology and preoperative patient-reported knee symptoms." Instead they found overall symptom severity — driven particularly by catching/locking and clicking/popping — correlated significantly with the burden of cartilage damage. CARTILAGE DAMAGE!! And if you had tricompartmental cartilage damage (i.e., medial, lateral, and patellofemoral). Then there was even greater symptoms severity…almost a dose response of cartilage damage to symptoms severity Perhaps the observations in this study help to explain why arthroscopic meniscal surgery has not consistently proven to be better than conservative management in randomized trials FDA Allows for First Point-of-Care Chlamydia and Gonorrhea Test to be Used in More Near-Patient Care Settings | FDA the U.S. Food and Drug Administration announced it is allowing the use of the Binx Health Assay for point-of-care testing for Chlamydia trachomatis and Neisseria gonorrhoeae, The test, which uses female vaginal swabs and male urine specimens, takes about 30 minutes and can be done right there in the office This is the first point of care test approved for Chlamydia trachomatis and Neisseria gonorrhoeae testing And I have no idea how much it will cost but my guess is a pretty penny Next article Rivaroxaban in Patients with Atrial Fibrillation and a Bioprosthetic Mitral Valve | NEJM The primary outcome was a composite of death, major cardiovascular events (stroke, transient ischemic attack, systemic embolism, valve thrombosis, or hospitalization for heart failure), or major bleeding at 12 months. In this open-label design Randomized trial of 1005 patients who were randomized to either 20 mg once daily rivaroxaban vs dose-adjusted warfarin in patients with atrial fibrillation and a bioprosthetic mitral valve In the end In patients with atrial fibrillation and a bioprosthetic mitral valve, rivaroxaban was noninferior to warfarin When it came to the composite primary outcome of death, major cardiovascular events, or major bleeding at 12 months. I have a couple problems Industry funded and open-label design – immediate bias into event rates. People doing the trial get paid ot do the trial and enroll people. They want this to work, they will try to show benefit as much as possible whenever possible. Nothing wrong with them, just human nature. This is for bioprosthetic mitral valves NOT mechanical valves HOWEVER This does seem to be consistent with observational and subgroup analysis from other studies and likely will change practice going forward. ADHD is real and what do you write for- well what if we could just get a large meta-analysis of almost 24K people Well we are in luck Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis - The Lancet Psychiatry Researchers examined efficacy and tolerability of data of the drugs used to treat attention-deficit/hyperactivity disorder from published and unpublished double-blind, randomized, controlled trials. In total they had 133 trials and included close to 14,000 children and 10,000 adults. They analysis was able to do indirect comparison which is when you take one study active arm and compare it to another study active arm and in the bit of statistical magic you get what appears to be results between the two active arms. So aspirin vs placebo and then Plavix vs placebo and then you can do an indirection comparison and BOOM stat magic and you have results for aspirin vs Plavix. Is it perfect? NO but is it better than nothing, usually. Some interesting results For children based on teachers' ratings only methylphenidate and modafinil were more effective compared to placebo BUT In adults modafinil didn’t beat placebo The best drug for adults was amphetamines I think one of the authors who commented on this said it best “results favored using methylphenidate in children and adolescents, and amphetamines in adults as first-line, short-term (12 weeks or under) treatment.” The authors did look for data at 26 and 52 weeks but found insufficient evidence. Which is to be expected as most mental health drugs only show improvement in the short instead of long duration but it also speaks to the importance of drug holidays when possible. These drugs have evidence for 12 weeks we have no idea what the good or bad long term effects are when taken for 12, 22, 32, or 42 years. Effect of Low-Intensity vs High-Intensity Home-Based Walking Exercise on Walk Distance in Patients With Peripheral Artery Disease: The LITE Randomized Clinical Trial | Cardiology | JAMA | JAMA Network How long or fast do you need to walk if you have PAD Does a low-intensity work just as good at high intensity? 305 participants with PAD Randomized to either low-intensity exercise, high-intensity exercise, and a nonexercise control group Participants in the walk groups were asked to walk 5 times per week for up to 50 minutes per session wearing an accelerometer to document exercise intensity and time. low-intensity group walked at a pace without ischemic leg symptoms. The high-intensity group walked at a pace eliciting moderate to severe ischemic leg symptoms. There were weekly phone calls with their ‘coach’ to help with adherence. Adherence was pretty good at around 85%!!! THAT ALONE IS IMPRESSIVE All participants did a 6 minute walk test at the beginning of the study and then again at the end of the study The primary outcome was mean change in 6-minute walk distance at 12 months In the end if you did Nothing then you decreased in for walk test distance by −15m, high intensity group GAIN 35m on their 6 minute walk test, but what about the low intensity- that is what we all care about is just a little bit of exercise beneficial. Is it ok to walk at a pace that is slow and doesn’t produce any pain and THOSE randomized to the load intensity group showed a DECREASE in their 6minute walk distance! They went down by -6.4M! No pain no gain! If you have PAD you can just lolly gag your walk around the block you have to push it. Sure a lolly gag pace wont lose you as much as doing nothing but if you push it you will see gains! I guess when it comes to PAD it is true what they say! no pain no gain but maybe they should say no walking pain less loss and more walking pain much bigger gains in 6minute walking distance
Hepatic encephalopathy basics, disseminated gonococcal infections, polyarthralgia question winner, jokes.Today is March 29, 2021.On December 23, 2020, the California Department of Public Health (CDPH) sent a “Dear Colleague” letter because of the increasing reports of disseminated gonococcal infections (DGI). Today, we want to share with you parts of that letter. CDPH is working with local health departments to investigate these cases of DGI, where some patients have experienced homelessness or using illicit drugs, particularly methamphetamine. The CDC noted a similar increase in cases in Michigan in late 2019.What is DGI? DGI is an uncommon but severe complication of untreated gonorrhea. DGI occurs when the sexually transmitted pathogen Neisseria gonorrhoeae invades the bloodstream and spreads to distant sites in the body, leading to clinical manifestations such as septic arthritis, polyarthralgia, tenosynovitis, petechial/pustular skin lesions, bacteremia, or, on rare occasions, endocarditis or meningitis. Patients have initially presented with joint pain attributed to another cause, which was only later determined to be due to DGI. Why is DGI increasing? Increased cases may be caused by decreased STD testing and treatment because of the COVID-19 pandemic, and not necessarily because of a more virulent strain of gonorrhea. What do we need to do as medical providers?Screen: Reinstate routine screening recommendations for STDs in females
An antibiotic-resistance conferring mutation in a neisserial porin: Structure, ion flux, and ampicillin binding
Link to bioRxiv paper: http://biorxiv.org/cgi/content/short/2020.11.06.369579v1?rss=1 Authors: Bartsch, A., Ives, C. M., Kattner, C., Pein, F., Tanabe, M., Munk, A., Zachariae, U., Steinem, C., Llabres, S. Abstract: Gram-negative bacteria cause the majority of highly drug-resistant bacterial infections. To cross the outer membrane of the complex Gram-negative cell envelope, antibiotics permeate through porins, trimeric channel proteins that enable the exchange of small polar molecules. Mutations in porins contribute to the development of drug-resistant phenotypes. In this work, we show that a single point mutation in the porin PorB from Neisseria meningitidis, the causative agent of bacterial meningitis, can strongly affect the binding and permeation of beta-lactam antibiotics. Using X-ray crystallography, high-resolution electrophysiology, atomistic biomolecular simulation, and liposome swelling experiments, we demonstrate differences in drug binding affinity, ion selectivity and drug permeability of PorB. Our work further reveals distinct interactions between the transversal electric field in the porin eyelet and the zwitterionic drugs, which manifest themselves under applied electric fields in electrophysiology and are altered by the mutation. These observations may apply more broadly to drug-porin interactions in other channels. Our results improve the molecular understanding of porin-based drug-resistance in Gram-negative bacteria. Copy rights belong to original authors. Visit the link for more info
Episode 32: VertigoThe sun rises over the San Joaquin Valley, California, today is October 20, 2020.It’s time to talk about vaccines again. The ACIP (Advisory Committee on Immunization Practices) posted new recommendations for meningococcal vaccinations on September 25, 2020. There are two kinds of meningococcal vaccines in the US: 1. Meningococcal conjugate or MenACWY vaccines (Menactra®, Menveo®, and MenQuadfi®)2. Serogroup B meningococcal or MenB vaccines (Bexsero® and Trumenba®). Let’s discuss how they are given.MenACWY: Menactra (MenACWY-D), Menveo (MenACWY-CRW), and MenQuadfi (MenACWY-TT) MenACWY routine: The meningococcal conjugate vaccine should be given to ALL PATIENTS at 11 to 12 years old, with a booster dose at age 16. Remember, it’s a two-dose series, the booster dose at age 16 is important to provide protection during the ages of highest risk of infection. So, that was easy. The hardest part is for patients younger than 10 years old because only patients who are at risk receive routine meningococcal conjugate vaccines before age 11. MenACWY in special groups: This vaccine is given to patients older than 2 months old only if they are at increased risk for meningitis (i.e., persistent complement component deficiencies; persons receiving a complement inhibitor such as eculizumab [Soliris] or ravulizumab [Ultomiris]); persons who have anatomic or functional asplenia; persons with HIV infection; microbiologists routinely exposed to Neisseria meningitidis; persons at increased risk in an outbreak; persons who travel to or live in hyperendemic or epidemic areas; unvaccinated or incompletely vaccinated first-year college students living in residence halls; and military recruits.) I invite you to consult ACIP recommendations regarding vaccination in special groups. MenB: Trumenba (MenB-FHbp), Bexsero (MenB-4C) MenB shared decision: MenB vaccination is not routinely recommended for all adolescents. It may be given to adolescents and young adults (16 through 23 years old, preferred age is 16-18 years old) on the basis of shared clinical decision. Those who decide to receive MenB vaccine, receive two doses 1-6 months apart depending on the brand name you use. MenB vaccines are not recommended before age 10 in any case. Adults older than 24 and older don’t need MenB unless they are at increased risk.MenB in special groups:Patients with certain medical conditions (persons with persistent complement component deficiencies; receiving a complement inhibitor; with anatomic or functional asplenia; microbiologists exposed to isolates of N. meningitidis; and persons at risk in outbreaks) should receive MenB vaccine. These recommendations will be included in the updated 2021 immunization schedules, and the AAFP will review changes to the schedules once they are available (1).This is Rio Bravo qWeek, your weekly dose of knowledge brought to you by the Rio Bravo Family Medicine Residency Program, from Bakersfield, California. Sponsored by Clinica Sierra Vista, Providing compassionate and affordable care since 1971.____________________________“A man is who he thinks about all day long” –Waldo Emerson.If you think you are not good enough, you may not reach your goals. So, think positive about yourself all day long, and you will become that person you think you are and will reach your goals.Hi, this is Dr Carranza, I’m a PGY3, and today I will interview a special guest.Question Number 1: Who are you? Hello, I’m Jagdeep Sandhu. I’m a 4th year medical student from Ross University, currently doing a sub-internship in family medicine. I’m originally from Seattle, Washington. I have an Indian ancestry, so I enjoy meditating and cooking Indian dishes.Question number 2: What did you learn this week? Lightheadedness vs VertigoThis week we learned about dizziness and its differentials. It is important to differentiate dizziness vs lightheaded because a lot of patients will say they are dizzy when they are truly lightheaded. To be honest dizziness (at least for me) is one of the toughest complaints to get from a patient as it is hard to pinpoint its etiology.Important questions to ask the patient are:Do you feel like you’re going to pass out? Do you experience a sense of darkness in front of your eyes? (points to syncope)Is the room spinning? Are you having nausea or vomiting? Ringing in your ears? (points to vertigo) Peripheral VertigoPeripheral refers to vertigo originated from the ear structures, whereas central from the brainstem. Differentials of peripheral vertigo include:Benign paroxysmal positional vertigo: Transient episodes of vertigo caused by stimulation of vestibular sense organs, this is most commonly due to calcium debris within the posterior semicircular canal, known as canalithiasis. It affects middle-age and older patients; and twice as many women than men. Classically, patients describe a brief spinning sensation brought on when turning in bed or tilting the head backward to look up. The dizziness is quite brief, usually seconds, rarely minutes.The way to Evaluate/diagnose BPPV is with Dix-Hallpike maneuver (turn the patient’s head 45 degrees to one side, then you help you lie back quickly so their head hangs slightly over the edge of the table. If horizontal or rotation nystagmus is noted, the patient has BPPV) and can be cured with Epley’s maneuver.Vestibular neuritis: This is inflammation of the vestibular nerve, which is usually caused by a viral infection. It’s characterized by rapid onset of severe, persistent vertigo, nausea, vomiting, and gait instability. Hearing is preserved but if there is hearing loss(unilateral), then it is diagnosed as labrynthitis. You can Evaluate/diagnose with a positive head impulse (or head thrust) test and gait instability but know that the patient is still able to ambulate. (lasts a few days and resolves spontaneously) Herpes zoster oticus: It is also known as Ramsay Hunt syndrome when it causes facial paralysis; it occurs due to latent VZV virus in the geniculate ganglion. The patient will complain of ear pain and vertigo. On exam, you will find vesicles in the auditory canal and auricle along with ipsilateral facial palsy. You can treat with Acyclovir or Corticosteroids. Meniere disease: Itoccursdue to excess endolymphatic fluid pressure, which causes episodic inner ear dysfunctionresulting in the classic triad of vertigo lasting for minutes to hours, usually associated with unilateral tinnitus and hearing loss. Unfortunately, the hearing loss can sometimes be permanent. It usually affects one ear and although it can occur at any age, most cases start between young adults and middle age adults. Evaluate and diagnose clinical features, get an audiogram for hearing loss. Patients go into remission spontaneously but it can reoccur. Other causes of peripheral vertigo: Labyrinthine concussion (traumatic peripheral vestibular injury)Perilymphatic fistula (complication of head injury, barotrauma, or heavy lifting in which a fistula develops at the otic capsule)Aminoglycoside toxicityVestibular schwannoma (unilateral hearing loss associated with neurofibromatosis type 2) Central VertigoVestibular migraine: The mechanism is unknown, so you have to rely on the patient's history of vertigo associated with migraine headache and classic migraine symptoms such as visual aura, photophobia, or phonophobia.Brainstem ischemia: which is due to embolic, atherosclerotic occlusions of the vertebra-basilar arterial system. A few things fall under this category such as TIA, Wallenberg syndrome (lateral medullary infarction), Labyrinthine infarction (Anterior Inferior cerebellar artery) etc. Evaluate and diagnose with Imaging of the head and treat according to diagnosis. Question number 3: Why is that knowledge important for you and your patients? It is important for when we are working at both the clinic and at the hospital as recognizing serious vertigo can help us plan for intervention. For example, if a patient presents with vertigo and on exam you find vesicles on their ear and facial paralysis then you can immediately begin therapy with a combination of Valacyclovir and Prednisone but if it is a severe case then the patient might need IV treatment.Also, if the patient has vascular risk factors then it is important to keep ischemia as part of your differential when your patient presents with acute sustained vertigo. Remember that for any stroke time of onset is KEY! CT should be done if MRI is not available but MRI is more sensitive for cerebellar infarctions.Question number 4: How did you get that knowledge? (learning habits)I did an ENT rotation in my 3rd yeard of medical school and learned from Dr Trang. I recommend that rotation to all medical students. I also searched in UpToDate, FP notebook app, AAFP and my attendings. See details below.____________________________Speaking Medical: Otolith by Gina Cha, MDStones are located in many unsuspected places in the body. Such is the case of otoliths. An otolith is a calcium carbonate structure in the saccule or utricle of the inner ear, specifically in the vestibular system of vertebrates. The saccule and utricle, in turn, together make the otolith organs. An otolith can cause great trouble if it’s out of its regular place. When otoliths are dislodged from their usual position within the utricle, and migrate into one of the semicircular canals (most commonly the posterior canal), moving the head causes movement of the heavier otolith debris in the affected canal causing abnormal endolymph fluid displacement and a resultant sensation of vertigo.____________________________Espanish Por Favor: Serenoby Claudia Carranza, MD, and Hector Arreaza, MDHi! This is Dr Carranza with our section “Espanish Por Favor”. The word of the week is SERENO (maybe we can have beach waves crushing in the background). SERENO is a state of mind, a peaceful feeling. To be SERENO means to be calm, peaceful, untroubled, tranquil. Sometimes when people are frustrated or too excited you can say: “Sereno, no te preocupes,” which you can loosely translate as “chill, don’t worry.”Sometimes you might ask someone how they are doing and they can say: “Sereno, sin preocupaciones,” which means “calm, without worries.” Nowadays not many people might actually feel that way but you can always remind them to lay back, relax, and take a deep breath “SERENO!”Another meanings of the word sereno includes “humidity on the atmosphere at night.” In some Latin American countries, sereno can make you sick if you, for example, shower and go outside at night, or you can get worse if you are sick and go outside. The sereno can also be used in folk medicine to “macerate” some herbal teas or remedies giving it a special property to cure illnesses. This may not be used in all countries but at least I know it’s true in Mexico and Venezuela.____________________________For your Sanity: Supermanby Tana Parker, MD Friend 1: Do you want to hear a really good Batman impression?Friend 2: Sure, go on. Friend 1: NOT THE KRYPTONITE!Friend 2: That’s Superman.Friend 1: Thanks, man, I've been practicing. “eBay is so useless. I tried to look up lighters and all they had was 13,749 matches.”“I just saw my wife trip and fall while carrying a laundry basket full of ironed clothes. I watched it all unfold.”I made a playlist for hiking. It has music from Peanuts , the Cranberries, and Eminem. I call it my trail mix._________________________Conclusion: Now we conclude our episode number 32 “Vertigo.” Dr Carranza and Jagdeep had an entertaining conversation about the differential diagnosis of peripheral and central vertigo. Don’t forget to practice the Dix-Hallpike and Epley’s maneuvers for BPPV. Otolith is a tiny stone located in the inner ear that can cause vertigo when it gets stuck in the semicircular canals. The word sereno (pronounced (say-RAY-noe) as an adjective is pretty much the same as the English serene, however, Dr Arreaza explained that sereno as a noun refers to the humidity on the air thought to be the “cause” of many ailments in some Latin cultures. Thanks for listening to Rio Bravo qWeek. If you have any feedback about this podcast, contact us by email RBresidency@clinicasierravista.org, or visit our website riobravofmrp.org/qweek. This podcast was created with educational purposes only. Visit your primary care physician for additional medical advice. This week we thank Hector Arreaza, Arianna Lundquist, Claudia Carranza, Jagdeep Sandhu, Gina Cha, and Tana Parker. Audio edition: Suraj Amrutia. See you next week! _____________________References:Meningococcal vaccine updates: https://www.aafp.org/news/health-of-the-public/20201007meningococcalvacc.html. Review full article at: https://www.cdc.gov/mmwr/volumes/69/rr/rr6909a1.htm?s_cid=rr6909a1_w Labuguen, Ronald H., M.D., University of Southern California, Los Angeles, California, Initial Evaluation of Vertigo, Am Fam Physician. 2006 Jan 15;73(2):244-251. https://www.aafp.org/afp/2006/0115/p244.html Furman, Joseph M, MD, PhD, and Jason JS Barton, MD, PhD, FRCPC, Evaluation of the patient with vertigo, UptoDate, last updated: Feb 11, 2020. https://www.uptodate.com/contents/causes-of-vertigo?search=vertigo§ionRank=1&usage_type=default&anchor=H5&source=machineLearning&selectedTitle=3~150&display_rank=3#H20
This free iTunes segment is just one tiny snippet of the fully-loaded 3-hour monthly Peds RAP show. Earn CME on your commute while getting the latest practice-changing peds information: journal article breakdowns, evidence-based topic reviews, critical guideline updates, conversations with experts, and so much more. Sign up for the full show at hippoed.com/PEDSRAPPOD. Pediatric ID specialist Michael Neely, MD, and Michael Cosimini, MD discuss how cephalosporins work and which bugs they do and do not kill. Pearls: In general, cephalosporins do not cover anaerobes, enterococcus, listeria and MRSA. Oral cephalosporins are generally not first line in pediatrics. Some exceptions include the treatment of UTIs and some skin and soft tissue infections; group A strep and sinopulmonary infections in penicillin allergic patients are other common indications. 1st generation cephalosporins do have gram positive coverage, but do not work well against strep pneumo, MRSA, enterococcus. They do cover some enteric gram negative bacteria, the “PECK” organisms. What are cephalosporin antibiotics and how do they compare to penicillins? Chemically, both penicillins and cephalosporins are beta-lactam antibiotics, with the beta-lactam portion responsible for bacterial killing. The chemical portions off the beta-lactam ring make the antibiotics different. Beta-lactam antibiotics work by binding to the penicillin-binding protein on the bacterial cell wall. These proteins have structural functions that maintain the integrity of the bacterial cell wall and therefore, when these antibiotics bind, the penicillin-binding protein is disrupted, the cell wall falls apart and the bacterial dies. How do you keep a straight spectrum of activity for antibiotics? To help with this, think of bacteria into big categories: gram-positive, gram-negative and “other”. Gram-positive bacteria include: Staph aureus (MSSA, MRSA), Streptococcus (Group A Strep, Group B Strep, Strep pyogenes, Strep viridans), Enterococcus, Pneumococcus, Listeria Gram-negative bacteria are a much bigger group and can be divided into: Respiratory gram-negatives include Moraxella, Haemophilus, Meningococcus Enteric gram-negatives include the “PECK” bacteria: Proteus, E.coli, Klebsiella What bacteria do cephalosporins not cover? In general, cephalosporins do not cover anaerobic bacteria, enterococcus, listeria and MRSA. There are a few exceptions to this rule. Cefoxitin (a second generation cephalosporin), for example, does have anaerobic coverage. It is commonly used in the treatment of PID as it covers enteric anaerobes and Neisseria gonorrhea. There is a 5th generation cephalosporin that does cover MRSA (discussed later). Are cephalosporins well absorbed? Generally speaking, cephalosporins in oral formulations are not as well absorbed as penicillins and are more difficult to get where they need to go outside the urinary tract. Also, generally speaking, no beta-lactam really gets into the spinal fluid in very high concentrations; all of them do have better penetration when there is inflammation. Practically, remember that the penetration into the CSF between ampicillin and ceftriaxone is negligible. What bacteria do first generation cephalosporins cover? Although the classic teaching is that cephalosporins are good for gram-positive coverage (staph and strep), this is not a hard and fast rule. As stated, enterococcus is not covered by any cephalosporin and MRSA is not covered by most cephalosporins. First generation cephalosporins are also good for coverage of the “PECK” enteric gram negative bacteria, but not good for coverage of other gram negative bacteria. These organisms tend to cause UTIs and therefore, first generation cephalosporins (for example, cephalexin) are frequently used for UTI treatment. Of course, resistance can occur. Even though strep pneumo is a gram-positive organism, when it comes to first generation cephalosporins, it acts like a gram-negative organism and therefore, first generation cephalosporins do not work well against strep pneumo. What about bacteria that develop resistance? A patient with an E. Coli UTI, for example, may have a microbiology laboratory report stating that the E. Coli is resistant to a first generation cephalosporin but the patient is still getting better. This may have to do with the type of infection the patient had; for example, a healthy patient with a simple cystitis may have been able to stay well hydrated and the normal immune system was able to clear the E. Coli. This question can also be answered in the context of breakpoints, that is when the bacteria become susceptible or resistant to the antibiotic depending on the site of infection. Some labs will actually label a bacteria resistant or susceptible depending on whether the infection is in the urine, spinal fluid or blood. Therefore, if a lab that reports site-specific breakpoints suggests that an E. Coli is resistant to a first generation cephalosporin in the urine, the lab has already taken into account the higher concentration of drug in the urine. Similarly, a pneumococcal isolate that may be resistant to ceftriaxone in the CNS may be susceptible to ceftriaxone as a pneumonia because there are much higher concentrations of ceftriaxone in the lungs than in the spinal fluid. When should a skin or soft tissue infection be treated with a first-generation cephalosporin? When should MRSA be suspected? This can be a tricky question as an outpatient, but there are some clues to gauge whether or not the infection may be caused by MRSA. One, it is helpful to know the community prevalence of MRSA. In some communities, community acquired staph aureus infections are up to 80-90% MRSA. In these communities, MRSA coverage should of course be given. If the prevalence is much lower, using a first generation cephalosporin, such as cephalexin may be reasonable. Other clues can be more specific to the patient the their families. Is the patient or family known to be colonized with MRSA? Have they had an MRSA infection in the past? If MRSA coverage is needed, either trimethoprim-sulfa or clindamycin generally is a good approach. A randomized controlled trial published in the NEJM showed no difference in outcomes when treating a known MRSA infection. Miller LG et al. Clindamycin versus trimethoprim-sulfamethoxazole for uncomplicated skin infections. N Engl J Med. 2015 Mar 19;372(12): 1093-103. https://www.ncbi.nlm.nih.gov/pubmed/25785967 In general, the quality of the infection does not help point to MRSA or not. There is some suggestion that if there is a soft-tissue abscess this is more likely staph aureus and if there is just pure erythema, tenderness and warmth without abscess, this is more likely to be Group A strep. Remember, no matter what antibiotic is started for cellulitis (or any infection, for that matter), follow up is essential. If you are on the right antibiotics, cellulitis should be improving within 24 hours.
Evolution of ST-4821 clonal complex hyperinvasive and quinolone-resistant meningococci: the next meningococcal pandemic?
Link to bioRxiv paper: http://biorxiv.org/cgi/content/short/2020.09.24.312546v1?rss=1 Authors: Chen, M., Harrison, O., Bratcher, H., Bo, Z., Jolley, K. A., Rodrigues, C. M., Bray, J., Guo, Q., Zhang, X., Chen, M., Maiden, M. C. Abstract: The expansion of quinolone-resistant Neisseria meningitidis clone ChinaCC4821-R1-C/B from ST-4821 clonal complex (cc4821) caused a serogroup shift from serogroup A to C in invasive meningococcal disease (IMD) in China. To establish the relationship among globally distributed cc4821 meningococci, we analysed whole genome sequence data from 173 cc4821 meningococci isolated in four continents from 1972-2019. These meningococci clustered into four sub-lineages (1-4), with sub-lineage 1 primarily comprising serogroup C IMD isolates (82%, 41/50). Most isolates from outside China formed a distinct sub-lineage (81.6%, 40/49, the Europe-USA cluster), with the typical strain designation B:P1.17-6,23:F3-36:ST-3200(cc4821) and harbouring mutations in penicillin-binding protein 2. These data show that the quinolone-resistant clone ChinaCC4821-R1-C/B has expanded to other countries. The increasing global distribution of B:cc4821 meningococci raises concern that cc4821 has the potential to cause a global pandemic and, this would be challenging to control though there is indirect evidence that Trumenba vaccine might afford some protection. Copy rights belong to original authors. Visit the link for more info
In dieser Folge von Mildly Interesting decken Sam und Caro auf, wie viel Kaffee noch gesund ist, was die Anzahl von Ertrunkenen mit Atomkraftwerken zu tun hat und wie CRISPR die Welt verändern könnte. Quellen: Kaffee & Raucher: Kast, B. (2018). Der Ernährungskompass: Das Fazit aller wissenschaftlichen Studien zum Thema Ernährung. München: C. Bertelsmann. Komische Korrelationen: http://www.tylervigen.com/spurious-correlations AIMS Public health study Sc, Y., & Muralidhara. (2016). Beneficial Role of Coffee and Caffeine in Neurodegenerative Diseases: A Minireview. AIMS Public Health, 3(2), 407-422. doi:10.3934/publichealth.2016.2.407 LEMMA, B. (2019). CRISPR DREAMS: THE POTENTIAL FOR GENE EDITING. Harvard International Review, 40(1), 6-7. doi:10.2307/26617383 Hille, F., & Charpentier, E. (2016). CRISPR-Cas: Biology, mechanisms and relevance. Philosophical Transactions: Biological Sciences, 371(1707), 1-12. Retrieved August 30, 2020, from http://www.jstor.org/stable/26143993 LEVY, S. (2016). New Hope for Malaria Control. BioScience, 66(6), 439-445. doi:10.2307/90007608 Bündins90/Die Grünen. (2020) WIR SORGEN FÜR GESUNDE LEBENSMITTEL OHNE GIFT UND TIERQUÄLEREI https://www.gruene.de/themen/agrarwende Scudellari, M. (2019). Self-destructing mosquitoes and sterilized rodents: the promise of gene drives. Nature. Retrieved 30.08.2020 from https://www.nature.com/articles/d41586-019-02087-5 Patrão Neves M, Druml C (2017) Ethical implications of fighting malaria with CRISPR/Cas9 BMJ Global Health 2017 (2; 3):e000396. Protocol for a controlled human infection with genetically modified Neisseria lactamica expressing the meningococcal vaccine antigen NadA: a potent new technique for experimental medicine. Laver, Jay Robert; de Graaf, Hans; Ibrahim, Muktar; Vaughan, Andrew BMJ Open 9(4) BMJ Group 2019-01 2044-6055 Beyond Halal: Maqasid al-Shari'ah to Assess Bioethical Issues Arising from Genetically Modified Crops. Majeed, Abu Bakar Abdul; Chang, Lee Wei Science and Engineering Ethics 26(3):1463-1476 Springer Netherlands 2020 1353-3452 Idris, S.H., Abdul Majeed, A.B. & Chang, L.W. Beyond Halal: Maqasid al-Shari'ah to Assess Bioethical Issues Arising from Genetically Modified Crops. Sci Eng Ethics 26, 1463–1476 (2020). https://doi-org.ezproxy.ub.unimaas.nl/10.1007/s11948-020-00177-6 Andy Rees. (2006). Genetically Modified Food : A Short Guide For the Confused. Pluto Press. Tutelyan, V. (2013). Genetically modified food sources : safety assessment and control. Elsevier/Academic Press
Neisseria meningitidis and Neisseria gonorrhea
Today we'll talk about two Gram-negative cocci: one that causes meningitis and one that causes an STD. --- Send in a voice message: https://anchor.fm/bradleysmicroboardreview/message Support this podcast: https://anchor.fm/bradleysmicroboardreview/support
Episode 270: Gram negative cocci - Neisseria meningitides
Gram negative cocci - Neisseria meningitides
Gram negative cocci - Neisseria gonorrhea
Episode 264: Gram positive branching filamentous rods - Neisseria overview
Neisseria overview
Episódio sobre um assunto muito prevalente! Discutimos os principais tópicos de Uretrite, comparando referências nacionais e internacionais e trazendo novidades sobre o assunto. Um tema de saúde pública relevante para todos! MINUTAGEM [02:28] salves [03:32] IST x DST, uretrite x cervicite [07:08] etiologias principais [10:00] manifestações clinicas [13:32] investigação etiologica [18:20] tratamento farmacológico inicial [25:00] uretrite persistente [30:22] outras condutas [36:07] desafio REFERÊNCIAS: Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis. Protocolo Clínico e Diretrizes Terapêuticas para Atenção Integral às Pessoas com Infecções Sexualmente Transmissíveis (IST). - Brasília, 2019 Moi, Harald, Karla Blee, and Patrick J. Horner. "Management of non-gonococcal urethritis." BMC infectious diseases 15.1 (2015): 294. Bazzo, M. L., et al. "First nationwide antimicrobial susceptibility surveillance for Neisseria gonorrhoeae in Brazil, 2015–16." Journal of Antimicrobial Chemotherapy 73.7 (2018): 1854-1861. UPTODATE Urethritis in adult men Laura H Bachmann Oct 31 2019.
This episode: DNA from related species can kill certain pathogens when they incorporate it into their genome! Download Episode (7.9 MB, 11.5 minutes) Show notes: Microbe of the episode: Ungulate tetraparvovirus 3 Paper summary (paywall) Takeaways Neisseria gonorrhoeae, the bacteria that cause gonorrhea, have the unusual ability of taking up DNA from their surroundings at any time and making use of it in their own genome. This helps them acquire useful traits that help them survive better, such as antibiotic resistance. But it turns out that the ability is also a secret weakness! This study showed that when N. gonorrhoeae takes up DNA from harmless, commensal species of Neisseria in the body, the DNA is similar enough to be incorporated into the genome but different enough that it kills the pathogen. This effect also occurs with a serious pathogen in the same genus, N. meningitidis. Journal Paper: Kim WJ, Higashi D, Goytia M, Rendón MA, Pilligua-Lucas M, Bronnimann M, McLean JA, Duncan J, Trees D, Jerse AE, So M. 2019. Commensal Neisseria Kill Neisseria gonorrhoeae through a DNA-Dependent Mechanism. Cell Host Microbe 26:228-239.e8. Other interesting stories: Kombucha could be good model system for studying microbial cooperation Antidepressants can modify bacterial metabolism of serotonin in the gut Email questions or comments to bacteriofiles at gmail dot com. Thanks for listening! Subscribe: Apple Podcasts, Google Podcasts, Android, or RSS. Support the show at Patreon, or check out the show at Twitter or Facebook.
Sonic Assault - 12 - Dischavizer, Smashing Dreams, Unabomber, Teorias do Amor Moderno, Neisseria, Kenfoikeumato e Deadfish.
No dia 30.12.2019 aconteceu no Contêiner Pub, em Diadema, o show das bandas Dischavizer, Smashing Dreams, Unabomber, Teorias do Amor Moderno, Neisseria, Kenfoikeumato e Deadfish, e Bloody J e Briseno Blaster estiveram lá para conferir essa confluência de bandas que vão do rock alternativo, passam pelo ska, o punk tradicional e o hardcore.
Neisseria gonorrhoeae („Gonokokken“) werden sexuell übertragen, verursachen weltweit eine hohe Morbidität und werden zunehmend gegen Antibiotika resistent. Till Koch und Axel Baumgarten diskutieren über die Gonorrhoe (Tripper), die durch Gonokokken verursacht wird. Dr. Axel Baumgarten ist Facharzt für Allgemeinmedizin im Zentrum für Infektiologie Berlin Prenzlauer Berg (ZIBP) und im Vorstand der DAGNÄ (Deutsche Arbeitsgemeinschaft niedergelassener … „Infektiopod#09 – Gonorrhoe“ weiterlesen
Emerging Infections: Sexually Transmitted Infections
Dr. Kami Kim, Chief of Infectious Diseases at the University of South Florida College of Medicine, discusses an important subset of emerging infections: sexually transmitted diseases (STIs). She initially reviews the current epidemiology of STIs in the U.S. She differentiates the more common and less common STIs. She goes on to discuss risk factors for sexually transmitted infections. She focuses on Neisseria gonorrhea infections, and discusses epidemiology, drug resistance, and treatment changes. She closes by sharing information on the diverse syndromes associated with Chlamydia trachomatis, including genital ulcer disease, urethritis, and cervicitis, extragenital infections, and pelvic inflammatory disease, and shares general treatment strategies and pitfalls.
164. Neisseria meningitidis & Waterhouse-Friederichsen syndrome
Neisseria meningitidis & Waterhouse-Friederichsen syndrome
This bug deserves a big round of applause and not just because it’s nicknamed “The Clap”. Check out this week’s episode to gasp in wonder at the tricks that Neisseria gonorrhoeae uses to tiptoe past your immune system. Then prepare to cringe at some old-timey treatments for the disease while we trace the history of this ancient pathogen. Finally, make sure you have a quarantini or placeborita in hand for when we chat about the not-so-cheery outlook for this particular sexually-transmitted infection. Believe us, this is one episode you’re not gonn(orrhe)a want to miss.
If you fell down yesterday, stand up today. –H. G. Wells Welcome back to RoshCast for Episode 47! Let’s kick off this episode with a review of Neisseria meningitides, an important topic for clinical practice and personal safety. Neisseria meningitides is highly contagious and antibiotic prophylaxis is indicated for close contacts of an infected patient, including read more... The post Podcast Ep 47: Salicylate Toxicity, Carbon Monoxide Poisoning, & More appeared first on RoshReview.com.
El programa de hoy lo dedicamos a hablar sobre la Neisseria gonorrhoeae, bacteria a la que se le esta asignando el calificativo de superbacteria al encontrarse cepas multiresistentes y porque al parecer nos acercamos a una era en la que no tendremos antibioticoterapia efectiva contra este microorganismo. Revisamos la microbiologías, epidemiologia y tratamiento de la misma. Referencia: Magnus Unemo y William M. Shafer Antimicrobial Resistance in Neisseria gonorrhoeae in the 21st Century: Past, Evolution, and Future. Clin Microbiol Rev. Julio 2014. Simon R. Harris y colaboradores. Public health surveillance of multidrug-resistant clones of Neisseria gonorrhoeae in Europe: a genomic survey. Lancet Infect Dis. May 2018. Frase de la Semana: Esta semana la tomamos de Andrew M. Greeley (5 de febrero de 1928 - 29 de mayo de 2013) quien fuera un sacerdote católico, sociólogo, periodista y novelista estadounidense. La frase dice: “Nacemos con dos enfermedades incurables, la vida, de la que morimos, y la esperanza, que dice que tal vez la muerte no sea el final”
071: Neglected Tropical Diseases and Vaccine Advocacy with Peter Hotez
Peter Hotez talks about neglected tropical diseases: what are they, where are they found, and where did the term “neglected tropical disease” come from, anyway? Hotez discusses some of the strategies his and other groups are using for vaccine development, and his work as an advocate for childhood vaccines and global health. Host: Julie Wolf Subscribe (free) on iPhone, Android, RSS, or by email. You can also listen on your mobile device with the ASM Podcast app. Julie's biggest takeaways: Renaming “other diseases” - a large collection of disparate diseases such as schistosomiasis, leishmaniasis, and onchocerciasis (also called river blindness) - as “neglected tropical diseases” by Hotez and colleagues was integral to bringing attention to the diseases of the bottom billion, people that live on less than one U.S. Dollar per day. Neglected tropical diseases are often chronic and debilitating without high mortality. These diseases trap people in poverty due to their long-term effects. The NTDs are often associated with terrible stigma that can lead to additional challenges for affected populations. Neglected tropical diseases are found worldwide, in rich and poor countries. The poorest peoples living in the G20 countries (and Nigeria) now account for most of the world’s NTDs. Parasitic infections present challenges for vaccine design, but reverse vaccinology may be a useful strategy. Reverse vaccinology mines genomes to identify promising vaccine candidates in silico, which are then narrowed sequentially for those that are expressed on the bacterial surface, immunogenic, and ultimately protective against disease. This strategy has worked for Neisseria meningitidis, and Hotez is hopeful that it will produce effective vaccines for the parasitic infections he studies. The tradition of individual fields and departments, combined with the old-fashioned notion that scientists needn’t spend their time engaging with the public, has led to flatlined budgets and the rise of anti-science movements. Scientists need to engage the public to ensure the future of science and science-based policy. Featured Quotes (in order of appearance): “The concept of ‘neglected tropical diseases’ was very much born out of the Millennium Development Goals launched in the year 2000.” “Treating NTDs in rich countries “is not a resource problem; it’s an awareness problem.” “If you want to enter global health, we need as many people with a scientific background to go into business and law and international relations as we need to go into traditional scientific pathways” “Many involved in the antivaccine movement disproportionately involve either parents who are affluent or educated, or both: those who know just enough to do a google search but without the background to separate the garbage from the important stuff. And of course the anti-vaccine groups are deliberately misleading.” “Research America found that 81% of Americans can’t name a living scientist. That’s our fault. We’re so inward looking that we aren’t taking the time to do public engagement.” Links for this episode Peter Hotez at Baylor College of Medicine Peter Hotez website Millennium Development Goals published by the World Health Organization in 2000 WHO list of Neglected Tropical Diseases Forgotten People, Forgotten Diseases by Peter Hotez Blue Marble Health by Peter Hotez Public Health United episode featuring Hotez HOM Tidbit: Oncocerciasis now: 1986 British Medical Journal report Send your stories about our guests and/or your comments to jwolf@asmusa.org.
Invasive Meningococcal Vaccination for Canadian Children and Youth - CPS Podcast
This podcast was produced by PedsCases and the Canadian Paediatric Society (CPS), and aims to summarize the 2017 CPS Practice Point: Update on invasive meningococcal vaccination for Canadian children and youth. In this episode, listeners will learn the clinical presentation and epidemiology of Neisseria meningitidis in Canada, the current vaccination schedule and guidelines for vaccination, and how to identify children and adolescents who may need extra vaccinations. This podcast was developed by Dr. Sarah Johnson, a first-year paediatrics resident at the Stollery Children’s Hospital at the University of Alberta, in collaboration with Dr. Joan Robinson, a paediatric infectious diseases specialist and associate professor at the University of Alberta.
This time on the ‘Gluten Free RN’ podcast, Nadine explores the connection between gluten intolerance and antibiotic-resistant threats. Because damaged intestines compromise the immune system, undiagnosed celiac patients are more likely to develop infections that necessitate antibiotics. Nadine summarizes the 2013 CDC report, Antibiotic Resistance Threats in the United States, explaining the three microorganisms identified in the report with a Threat Level of Urgent. Listen and learn how to protect yourself and your family from the public health threat posed by these bacteria! What’s Discussed: The prevalence of undiagnosed celiac disease and gluten intolerance 30-50% of the population carry the HLA-DQ2 and/or DQ8 genes The importance of healthy intestinal tissue 70-90% of the immune system is in your intestines The soldier analogy Healthy villi are like rested soldiers with loaded weapons on a clear day who can easily take out antigens that don’t belong Damaged villi are like soldiers on a bender with inadequate weaponry, operating in smoke and fire – they either don’t work at all or fire randomly at antigens The need for a more judicious approach to prescribing antibiotics Overuse of antibiotics wipes out good microbiome along with bad How to rebuild microbiome Kombucha High-quality probiotics Fermented foods Apple cider vinegar The need for IgA and IgG testing to complement a celiac panel The public health threat posed by antibiotic-resistant bacteria The 2013 CDC report details 2 million illnesses and 23,000 deaths yearly The connection between damaged intestines and a higher risk of bacterial infection requiring antibiotics The three microorganisms with a Threat Level of Urgent Clostridium difficile (causes profuse diarrhea, 14,000 deaths/year) Carbapenem-resistant Enterobacteriaceae (50% fatal, 600 deaths/year) Neisseria gonorrhoeae The causes of inflammation in your intestines Gluten Dairy Sugar Why Nadine has concerns about the potential pandemic and huge loss of life presented by large numbers of undiagnosed celiac patients who are susceptible to bacterial infections Resources Mentioned: CDC Report: Antibiotic Resistance Threats in the United States, 2013 Enterolab Website Cyrex Laboratories Website PubMed Connect with Nadine: Instagram Facebook Contact via Email Books by Nadine: Dough Nation: A Nurse's Memoir of Celiac Disease from Missed Diagnosis to Food and Health Activism
Welcome back to another episode of Roshcast. This week are are adding a new level of spaced repetition by doing a brief review of the previous week's key take away points before diving into the new material. In this episode we cover important topics including ketamine, Bell's palsy, tachydysrhythmias, jellyfish sting, type I error, meningitis prophylaxis, and postpartum hemorrhage. Enjoy. The post Podcast Ep 5: Neisseria meningitidis, Bell’s Palsy, Peripartum Hemorrhage, & More appeared first on RoshReview.com.
Hosts: Vincent Racaniello, Michael Schmidt, Elio Schaechter and Michele Swanson. The TWiM team is amazed by the ocelloid, and an evolutionary battle for iron between mammalian transferrin and bacterial transferrin-binding protein. Subscribe to TWiM (free) on iTunes, Stitcher, RSS, or by email. You can also listen on your mobile device with the Microbeworld app. Links for this episode A unicellular camera-type eye structure (PLoS One) Escape from iron piracy (Science) Iron in infection and immunity (Cell Host Micr) Nutritional immunity (Nat Rev Micro) Evolutionary Path (Matthew Barber) Image credit: Janet Iwasa Sponsors for this episode: SciMedSolutions, ICAAC-ICC Send your microbiology questions and comments (email or mp3 file) to twim@twiv.tv, or call them in to 908-312-0760. You can also post articles that you would like us to discuss at microbeworld.org and tag them with twim.
Gonorrhoea and chlamydia screening in HIV clinics: time for new tools and targets
Prevalence studies indicate approximately 10% of patients in HIV clinics may be infected with Neisseria gonorrhoeae (NG) and/or Chlamydia trachomatis (CT) at any given time, and a study recently published in STI by Burchell and colleagues reveals that a modest increase in testing in their clinic did not improve detection of CT and NG. Khalil Ghanem, STI associate editor, asks Stephen Berry, Division of Infectious Diseases, Johns Hopkins University School of Medicine, to comment on the paper and what can be done to improve detection of NG and CT. Read Dr Berry's full editorial: http://goo.gl/ABefHz Read Burchell et al's paper: Modest rise in chlamydia and gonorrhoea testing did not increase case detection in a clinical HIV cohort in Ontario, Canada http://goo.gl/JPsp2e
Nuestro sistema digestivo está colonizado por miles de millones de bacterias, de cientos de especies diferentes. Donde más abundan es en el estómago y el intestino pero también las hay en las fosas nasales y la faringe. Una de esas bacterias es Neisseria meningiditis, vulgarmente llamada meningococo, causante de infecciones de la sangre y de meningitis. Evidentemente, si la bacteria puede vivir normalmente en la mucosa nasofaríngea, sin causar estas terribles enfermedades, es porque nuestro sistema inmune la mantiene controlada ¿Qué origina que el meningococo se convierta en una bacteria virulenta causante de enfermedad?
Vincent, Elio, and Michael discuss how temperature triggers Neisseria menigitidis immune evasion, and protection of mice from ionizing radiation by feeding them black mushrooms.
Vincent, Elio, Michael, and Michele discuss the curious outer membrane vesicles of Neisseria meningitides, and sources of Clostridium difficile infection revealed by genome sequencing.
Summary of the March 5, 2013 issue, including articles on colorectal cancer screening, Neisseria gonorrhoeae, hepatitis C virus and hepatocellular carcinoma, and cognitive impairment and atrial fibrillation, as well as a commentary on access to care for undocumented migrants and an accompanying supplement, "Making Health Care Safer: A Critical Review of Evidence Supporting Strategies to Improve Patient Safety."
Chlamydia trachomatis and Neisseria gonorrhea: A Clinical Review
An overview of CT/NG, including bacteriology and disease burden, infection epidemiology and diagnosis, screening guidelines, treatment, and prevention.
On episode #1 of the podcast This Week in Microbiology, Vincent, Cliff, Michael, and Stan discuss transfer of DNA from a human host to a bacterial pathogen, and the ability of dry copper to kill bacteria on contact.
Normalflora der Bindehaut Neugeborener in zwei Krankenhäusern in Argentinien und Paraguay
Medizinische Fakultät - Digitale Hochschulschriften der LMU - Teil 07/19
In vorliegender prospektiver Arbeit konnten koagulase-negative Staphylokokken und anaerobe Propionibakterien als die häufigsten Vertreter der Normalflora auf der Bindehaut von insgesamt 190 vaginal- und per Kaiserschnitt geborenen Neugeborenen in den beiden Krankenhäusern Asunción (Paraguay) und Clorinda (Nord-Argentinien) aufgezeigt werden. Der Untersuchungszeitraum lag in Asuncion zwischen dem 01. August und dem 06. Oktober, in Clorinda zwischen 15. September und dem 14. Oktober 2002. Hinsichtlich der untersuchten Antibiotika-Resistenzspektren von aus Neugeborenenaugen isolierten Staphylokokken stehen hohe Sensibilitätsraten bezüglich in der Studienregion noch wenig eingesetzter Substanzen wie Fluorchinolone, sowie eine Vollsensibilität gegenüber Imipenem und Vancomycin, ausgeprägtem Resistenzverhalten bezüglich Penicillinen gegenüber. Eine äußerst wichtige Feststellung in vorliegender Arbeit ist der fehlende Nachweis von Neisseria gonorrhoeae in den Augen von Neugeborener sowie in den Proben aus dem unteren Genitaltrakt untersuchter Mütter. Der fehlende Chlamydiennachweis im unteren Genitaltrakt der 81 untersuchten schwangeren Patientinnen weist auf eine niedrige Prävalenzraten dieser Mikroorganismen in untersuchtem Studienkollektiv hin, eine Tatsache, deren endgültige Bestätigung jedoch noch auf weitere Studien in der Zukunft angewiesen ist. Aus letzteren Aspekten könnte ein Verzicht auf den Einsatz von Silbernitratlösung als Prophylaxe von ophthalmia neonatorum (Prophylaxe nach Credé) gerechtfertigt werden, eine Maßnahme, welche innerhalb der letzten zehn Jahre durch den Einsatz alternativer antibiotisch wirksamer Substanzen bereits an Bedeutung verloren hat. Der Vorteil jener Alternativpräparate ist die deutlich geringere lokale Reizung des Auges nach Verabreichung im Vergleich zu hohen Raten von Silbernitrat-induzierten chemischen Konjunktividen. Der Einsatz von Povidon-Jod als eine wirksame, neue Form der Prophylaxe sollte jedoch in weiteren Studien in unserer Studienregion klinisch noch weiter untersucht werden.
A summary of the July 17, 2007 issue. Includes in-depth summaries of articles on changes in hospital mortality associated with implementation of residency work hour regulations, national trends in antibiotic susceptibility of Neisseria gonorrheae isolates, and the recent update of the US Preventives Services Task Force clinical guidelines on screening for chlamydia. From the July 17, 2007 issue.
Untersuchungen über die Interaktion von Meningokokken mit Zellen der Blut-Hirn-Schranke
Tierärztliche Fakultät - Digitale Hochschulschriften der LMU - Teil 01/07
Neisseria meningitidis, ein Gram negatives pathogenes Bakterium ist eine der Ursachen für schwere Septikämie und Meningokokkenmeningitis. Nach Besiedelung des menschlichen Nasopharynx und Übertritt in die Blutbahn besteht ein zentraler Schritt in der Pathogenese der durch N. meningitidis verursachten bakteriellen Meningitis in der Interaktion der Bakterien mit Zellen der Blut-Hirn-Schranke. Die Schwere der Erkrankung scheint direkt mit der Produktion proinflammatorischer Zytokine, Chemokine und Wachstumsfaktoren zu korrelieren. Daher wurde in der vorliegenden Studie mit Hilfe eines Zellkulturmodells die Freisetzung von Tumornekrosefaktor alpha (TNF-a), Interleukin-1b (IL-1b), Interleukin-6 (IL-6), Interleukin-8 (IL-8), Monocyten-attrahierendem Protein-1 (MCP-1) und transformierendem Wachstumsfaktor beta (TGF-b) durch Gehirnendothelzellen nach Infektion mit Meningokokken analysiert. Mit ELISA und RT-PCR wurde die Freisetzung von Zytokinen und die Transkription der Zytokin-codierenden Gene von humanen Gehirnendothelzellen (HBMEC) nach Infektion mit dem Meningokokkenstamm MC58* und seiner unbekapselten isogenen Mutante MC58 siaD der Serogruppe B nachgewiesen. In Übereinstimmung mit der Zytokinfreisetzung wurde dabei ein typisches Genexpressionsmuster festgestellt. Beide Bakterienstämme beeinflußten die Transkription der Gene, die für IL-6 und IL-8 kodieren, wobei die Transkription bei den Zellen, die mit dem unbekapselten Stamm infiziert wurden, früher nachzuweisen war. Die Transkription des TNF-a Gens wurde nur nach der Infektion mit der unbekapselten Mutante nachgewiesen. Für IL-1b und MCP-1 wurde keine verstärkte Transkription festgestellt, wogegen das Gen, welches für TGF-b codiert, von infizierten wie uninfizierten Zellen gleichermaßen exprimiert wurde. Neben den intakten Bakterien führte auch die Stimulation mit Außenmembranproteinen zu einer Induktion der Zytokinfreisetzung. Die Verhinderung der Internalisierung der Bakterien in die Zellen bzw. die Blockade des a5b1 Integrin Rezeptors reduzierte die Freisetzung von IL-8 und TNF-a, nicht jedoch die Freisetzung von IL-6. Während durch die IL-6 oder IL-8 Prästimulation der HBMEC keine Veränderung des Invasionsverhaltens der Meningokokken beobachtet werden konnte, führte eine Prästimulation mit TNF-a zu einer deutlich gesteigerten Invasion der Bakterien in die Zellen. Diese Ergebnisse machen deutlich, daß der Entzündungsprozeß im Gehirn eine komplexe Interaktion zwischen Bakterium und Wirtszelle erfordert. Dabei spielen die Gehirnendothelzellen offensichtlich eine wichtige Rolle in der interzellulären Kommunikation der beteiligten Zellen, indem sie Zytokine als Immunmodulatoren freisetzen, die ihrerseits zu veränderter Expression von Adhäsionsmolekülen führen könnten.






























































